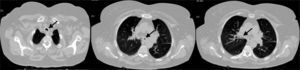
A 68-year-old female with a diagnosis of childhood asthma, was referred to the pulmonologist for recurrent episodes of acute severe dyspnoea and wheezing for the last three years. These were treated as asthma, with inhaled bronchodilators and corticosteroids, but without significant clinical improvement. She performed lung function tests, which showed a moderate bronchial obstruction, with limited response to bronchodilation. Chest CT revealed tracheal and bronchial wall thickening and luminal narrowing (Fig. 1). This tracheobronchial stenosis was also observed in bronchoscopy. In the subsequent year of follow up, she developed red eye episodes, polyarthritis, recurrent ear pain and saddle nose deformity. Autoimmunity was negative, but sedimentation rate was elevated (26mm). Relapsing polychondritis was then diagnosed, according to the criteria developed by McAdams et al.1 The patient started treatment with oral corticosteroids and methotrexate, with good clinical response. No specific treatment for tracheobronchial stenosis has yet been required. We highlight the clinical challenge of this diagnosis, due to insidious manifestations of the disease, and raise awareness of tracheobronchial involvement in relapsing polychondritis, which in some cases can lead to critical airway stenosis.2
The Impact Factor measures the average number of citations received in a particular year by papers published in the journal during the two preceding years.
© Clarivate Analytics, Journal Citation Reports 2025
SRJ is a prestige metric based on the idea that not all citations are the same. SJR uses a similar algorithm as the Google page rank; it provides a quantitative and qualitative measure of the journal's impact.
See moreSNIP measures contextual citation impact by wighting citations based on the total number of citations in a subject field.
See more