The persistent air leaks due to alveolopleural fistula is not an uncommon complication of pneumothorax, particularly secondary ones. Unidirectional flow endobronchial valves initially designed for lung volume reduction are the latest tool in the therapeutic armamentarium.
We present a patient with chronic obstructive pulmonary disease (COPD) with a persistent pneumothorax in spite of three pleurodesis, which was able to be resolved with the placement of two IBV™ valves.
La fuga aérea persistente por fístula alveolopleural no es una complicación infrecuente del neumotórax, sobre todo de los secundarios. Las válvulas endobronquiales de flujo unidireccional diseñadas para la reducción del volumen pulmonar son la última incorporación en el arsenal terapéutico.
Se presenta el caso de un paciente con enfermedad pulmonar obstructiva crónica (EPOC), con un neumotórax persistente a pesar del tratamiento con tres pleurodesis, y que pudo resolverse con la implantación de dos válvulas tipo IBV.
Persistent air leaks due to alveolar-pleural fistula are not an infrequent complication of pneumothorax, especially secondary pneumothorax. It may affect up to 20% of COPD patients,1,2 while in patients with pulmonary emphysema who have undergone lung volume reduction surgery, it is reported in up to 45% of cases.3 This complication carries with it morbidity and mortality, long hospital stays and added costs. Unidirectional-flow endobronchial valves designed for lung volume reduction are the latest incorporation to the therapeutic armamentarium. We present the first case in Spain (and the second case internationally) of the placement of IBV® valves (Olympus Corp., Tokyo, Japan) for the treatment of persistent air leak.
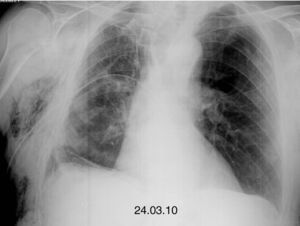
Clinical NotesThe patient is an 88-year-old male, ex-smoker with moderate COPD (FEV1 53%) who had not required previous hospitalizations, having systemic arterial hypertension, right hip prosthesis surgery and glaucoma, with a good quality of life and performing daily activities with complete independence. He consulted for dyspnea at his district hospital, where pulse-oximetry while breathing room air confirmed a saturation of <90% and simple chest radiography showed right pneumothorax occupying 1/3 of the hemithorax as well as chronic changes of bronchopneumopathy with apical hyperclarity. A pleural drain was placed, but given the persistence of the air leak, the patient was transferred to the reference hospital for elective surgical treatment. Two weeks later, we carried out apical bullectomy and talc pleurodesis using video-assisted thoracoscopy, and the patient was discharged with lung reexpansion a week later. However, 48h afterwards, the patient was re-hospitalized at his district hospital for right basal pneumonia in bacterial filiation that became complicated three days later with hydropneumothorax. He was sent once again to the reference hospital, where pleuroscopy was performed with a second talc pleurodesis that was not effective, and at 15 days a third pleurodesis was done with autologous blood, with no success. Given the persistence of the air leak, the patient was sent to our center. Upon arrival, the conventional water-seal drainage system was withdrawn and replaced with the Thopaz™ electric aspiration system (Medela, Baar, Switzerland), with an observed debit of approximately 330ml/min under aspiration of −20cm of water. The patient was intubated with an orotracheal tube with an internal diameter of 9mm to avoid a low tidal volume that could diminish the air leak. With an Olympus BF-1T180 therapeutic video-assisted bronchoscope (Tokyo, Japan) and a number 4 Fogarty arterial balloon (Edwards Lifesciences LLC, Irvine, CA, USA) the lobar bronchi were sequentially occluded and, in the case of decline of the air leak, so were the pertaining segmental bronchi. LSD certified a significant fall in the debit during the occlusion of the anterior and apical segments, which was mild (40ml/min) in the posterior segment. It was decided to implant valves only in the first two. After measuring the diameters with a previously calibrated balloon for the IBV® system, a 7-mm diameter valve was placed in the anterior segment and a 6-mm valve in the apical segment (Fig. 1), to stop the air leak. However, a few hours later, the air leak re-initiated with a leak of about 150ml/min under continuous aspiration −20cm of water. Simple chest radiograph after the procedure with continuous aspiration showed a practical reexpansion of the right pneumothorax (Fig. 2). The patient was derived to his hospital of origin, where he was discharged with a drain tube connected to a Heimlich valve that was withdrawn after 10 days. Six months after the medical discharge, the patient is stable without having removed the valves, and their future extraction would only be considered in the event that a possible pulmonary complication was associated with them.
DiscussionAlveolar-pleural fistulas are caused by lung resections, bullous emphysema, advanced-stage sarcoidosis, post-radiotherapy fibrotic changes or ablation by radiofrequency. An air leak is defined, by consensus, as being persistent if it does not stop in 7 days. There is no physiological base to consider that this time it is required in order to consider initiating therapeutic actions, while other variables such as the patient's baseline disease, clinical repercussions or magnitude of the air leak should also be considered. In this manner, if the debit of the leak is small or moderate, a conservative approach with maintenance of the drainage tube after the 7 days can be adequate. For important leaks or those with clinical repercussions in the patient, early surgical treatment before the 7 days is the best option. According to current guidelines on the management of pneumothorax, when surgery is not possible due to either advanced baseline disease, unstable clinical situation or the refusal of the patient, alternative treatments can be contemplated, such as endoscopic interventions. However, given the progressive evidence of its effectiveness, it is possible that future guideline editions may even recommend endoscopic treatment with unidirectional valves before surgery. The overall cost of the procedure (approximately 2200€ per valve in Europe) also favors their implantation. There are different types of endoscopic treatment for persistent air leak due to alveolar-pleural fistula. These include the application of adhesive substances, such as fibrin, albumin or glutaraldehyde, other proinflammatory irritants, such as ethanol or antibiotics, and a third group made up of the implantation of endobronchial blockers, such as Watanabe spigots (Novatech, Cedex, France) and more recently unidirectional flow valves like Zephyr® by Pulmonx (Redwood City, CA, USA) and IBV® by Olympus Corp (Tokyo, Japan).
The Watanabe spigots are specifically designed for reducing air leaks by means of total occlusion of the affected bronchus. They are manufactured out of radiopaque silicone and are made in various diameters (5, 6, and 7mm) with a length of 1 and 1.5cm. Watanabe et al. reached in 60 patients a resolution in 40% and a reduction of the debit in 38% of the cases, with a mean of 4 spigots per patient.4 The Zephyr® and IBV® unidirectional valves allow for the centripetal flow of air and secretions, and were initially designed for lung volume reduction treatment in emphysema. After incorporating sufficient bibliographic evidence, the Food and Drug Administration (FDA) in the United States approved the indication of IBV® as a treatment for air leaks in 2006. The Zephyr® valve has an aperture in its center and works by means of a system similar to the Heimlich valve. On the other hand, the IBV® valve allows for the flow of air and secretions around its perimeter by a system of flexible metallic umbrella-like rods. Travaline et al. used the Zephyr® valves in the treatment of 40 subjects affected by persistent alveolar-pleural air leak of varying etiologies (25 spontaneous, 7 post-surgery, 6 iatrogenic, 1 volume reduction surgery, 1 traumatic), reaching complete resolution in 47.5% of the cases and a reduction of the leak in 45%.5 A mean of between 2 and 3 valves were used per patient, ranging between 1 and 9 valves. Apart from this publication, another 13 patients were reported in 6 different articles with a high success rate. The only case published using the IBV® valves corresponds with a patient who presented pneumothorax and massive subcutaneous emphysema 8 days later due to radiofrequency ablation of a local relapse after atypical resection due to squamous carcinoma three years before. The authors report a significant reduction of the leak with the implantation of two valves, measured 15min after the procedure.6
All the endoscopic approaches require the localization of the most distal bronchus possible on which the entering air flow depends. The most widely used system is the consecutive occlusion of the bronchial openings from larger to smaller caliber during a time ranging between 30s and 3min, depending on the authors. The visualization of the variation in intensity of the bubbling of the conventional water-seal aspiration systems is to date the procedure used to guide the pulmonologist during balloon occlusion. The incorporation of electrical suction systems with digital screens, such as Thopaz™ (Medela), enables the specialist to numerically check the real-time air debit, and therefore it is an advancement in the management of these situations.
The cases published verify two facts that indirectly reflect the complexity of persistent air leaks. First of all, the fact that complete resolution of the air leak is not reached in all patients upon implantation and, second of all that the number of valves necessary oscillates between 2 and 4 on an average. The model with one fistulous orifice depending on one segmental bronchus would represent a simplistic model. The incomplete reduction of the air leak, either during balloon occlusion or after the implantation of the valves, could be explained by the intrapulmonary air circulation7 or the presence of multiple fistulous orifices. Complementary explorations such as CT,8 bronchography by CT9 or ventilation gammagraphy with Tc99m10 can be useful for localizing and determining the number of fistulas. Recently, the Pulmonx company has made available the Chartis® system, a pneumotachometer coupled to an endobronquial balloon, that could be a useful tool for determining the existence of collateral circulation.11 The impossibility of complete occlusion of the fistula after the placement of the valves should not be initially considered a failure. The simple reduction of the air debit may transform an incontrollable air leak into a situation for conservative management until it heals, as occurred in our patient as described.
Conflict of interestThe authors declare having no conflict of interests.
We would like to thank Dr. X. González for his comments.
Please cite this article as: Rosell A, et al. Tratamiento endoscópico de la fuga aérea persistente alveolo-pleural con una válvula endobronquial unidireccional. Arch Bronconeumol. 2011;47:371–3.