Hospitalizations for acute exacerbation of COPD (AECOPD) generate high consumption of health resources, frequent readmissions and high mortality. The MAG-1 study aims to identify critical points to improve the care process of severe AECOPD requiring hospitalization.
MethodsObservational study, with review of clinical records of patients admitted to hospitals of the Catalan public network for AECOPD. The centers were classified into 3 groups according to the number of discharges/year. Demographic and descriptive data of the previous year, pharmacological treatment, care during hospitalization and discharge process and follow-up, mortality and readmission at 30 and 90 days were analyzed.
ResultsA total of 910 patients (83% male) with a mean age of 74.3 (+10.1) years and a response rate of 70% were included. Smoking habit was determined in only 45% of cases, of which 9% were active smokers. In 31% of cases, no previous lung function data were available. Median hospital stay was 7 days (IQR 4–10), increasing according the complexity of the hospital. Mortality from admission to 90 days was 12.4% with a readmission rate of 49%. An inverse relationship between length of hospital stay and readmission within 90 days was observed.
ConclusionsIn a large number of medical records, smoking habit and lung function tests were not appropriately reported. Average hospital stay increases with the complexity of the hospital, but longer stays appear to be associated with lower mortality at follow-up.
Las hospitalizaciones por exacerbación aguda de EPOC (EAEPOC) generan un elevado consumo de recursos sanitarios, frecuentes reingresos y una alta mortalidad. El estudio MAG-1 pretende identificar aquellos puntos críticos y mejorables en el proceso asistencial de la EAEPOC que requiere ingreso hospitalario.
MetodologíaEstudio observacional, de revisión de historias clínicas de pacientes ingresados en hospitales de la red pública por EAEPOC. Los centros se clasificaron en 3 grupos según el número de altas/año. Se analizaron datos demográficos y descriptivos del año previo, tratamiento farmacológico, atención durante la hospitalización y proceso de alta, así como mortalidad y reingresos a los 30 y 90 días.
ResultadosSe estudió a 910 pacientes (83% varones), con una edad media de 74,3 (+10,1) años y una tasa de respuesta del 70%. Solo constaba el hábito tabáquico actual en un 45% de los casos y de estos un 9,8% eran fumadores activos. En un 31% de los casos no constaban datos espirométricos previos. La mediana de la estancia fue de 7 días (RIQ: 4-10), aumentando con la complejidad del centro. La mortalidad observada desde el ingreso a los 90 días fue del 12,4% con una tasa de reingresos del 49%. Se observó una relación inversa entre los días de estancia hospitalaria y las readmisiones a 90 días.
ConclusionesEn un elevado número de historias clínicas no consta adecuadamente el hábito tabáquico ni las pruebas de función pulmonar. La estancia media aumenta con la complejidad del hospital, aunque mayores estancias parecen asociarse con menor mortalidad en el seguimiento.
Chronic obstructive pulmonary disease (COPD) affects more than 10% of the Spanish population aged over 40 years, and is often underdiagnosed.1,2 Despite marked improvements in treatment, overall mortality has not declined significantly, and severe exacerbations continue to be a major health problem.3
Acute exacerbations of COPD (AECOPD) are key features in the natural history of the disease.4 Mortality is known to increase with the frequency of exacerbations,5,6 especially if these are severe enough to require hospitalization.7 Comorbidities, which are very common in these patients, also increase mortality and hospital readmission rates.8 AECOPDs worsen quality of life9 and in most patients, recovery to baseline levels takes over 1 month.10 Discharge plans, integrated care and alternatives to conventional hospitalization are crucial in order to improve the care given to patients admitted for AECOPD.11–13
Despite their importance, only partial and often fragmented data are available on the clinical management of COPD in patients hospitalized for exacerbations.14
The Master Plan for Respiratory Diseases (PDMAR) is a strategy developed by the Catalan Government Department of Health to introduce improvements in the care of patients with respiratory diseases.15 Within this context, the MPOC Aguditzat Greu (MAG-1 [Exacerbated Severe COPD]) study was designed as an audit to identify areas for improvement in the entire hospital care process, encompassing arrival at the emergency department, admission, and follow-up at 30 and 90 days post-discharge. It also analyzed differences between hospitals according to the volume of admissions and hospital complexity level.
MethodologyStudy DesignObservational, medical record review study of patients admitted for AECOPD. Patients admitted to hospital or in hospital-at-home programs were included. Participating hospitals were assigned a quota of patients to include in the study, based on their annual discharge rates. Patients were consecutively evaluated from 15 January 2011 until the quota had been reached.
Study SettingAll public hospitals in Catalonia that treated more than 50 cases admitted for COPD exacerbation in 2010 were invited to participate in the study by the Catalan Department of Health (CatSalut).
Hospital ClassificationHospitals that agreed to participate were classified according to the number of discharges for COPD exacerbation recorded in the CatSalut minimum basic data set16 for the year 2010. Hospitals were classified into 3 groups:
- •
Level I hospital: fewer than 100 discharges/year for AECOPD.
- •
Level II hospital: between 100 and 400 discharges/year for AECOPD.
- •
Level III hospital: more than 400 discharges/year for AECOPD.
Two hundred variables were studied, grouped into 7 categories:
- 1.
Demographic and descriptive data on the patient's condition in the 12 months prior to admission using a specifically designed questionnaire, which included questions on previous diagnosis, clinical follow-up, admissions for COPD, and number of chronic diseases described in the primary and secondary diagnosis in the discharge reports.
- 2.
Pharmacological treatment prior to hospital admission, including home oxygen therapy and other home respiratory therapies.
- 3.
Data related with care in the emergency department as the source of the referral, clinical status on admission and care process in the emergency department.
- 4.
Data related with the hospital stay, admission from the emergency department to the ward, use of non-invasive mechanical ventilation (NIV), department that treated the patient or early mobilization, among others.
- 5.
Information on the discharge process, such as clinical assessment, information received by the patient in the discharge report and destination on discharge.
- 6.
Outcome variables related with admission and follow-up at 30 and 90 days, including mean stay, mortality and readmissions.
- 7.
Comparison between hospitals by level.
COPD severity was assessed on the basis of FEV1, expressed as a percentage of predicted, when spirometric data were available. BODE cut-off points were used to define the categories, combining the severe and very severe categories; mild COPD was considered as FEV1 between 65% and 80%, moderate between 50% and 64%, and severe ≤49%.
Data CollectionEach hospital appointed a member of staff to review the hospital medical records. All professionals who carried out the fieldwork had received appropriate training and followed a procedure manual. During the data collection period, they were also provided with a contact telephone number for the research team in order to resolve any problems. One of the investigators (ET) was responsible for monitoring and supporting each site throughout the study.
A specific database was created for the study. Quality control was carried out to detect possible inconsistent values, in which case the person appointed to review the data was contacted to correct errors.
Ethical AspectsThis study was part of the healthcare quality control strategies put in place by CatSalut. The study design complied with international ethical guidelines, and patient and data confidentiality was guaranteed in accordance with Spanish organic law on Personal Data Protection (15/1999, 13 December). Those responsible for analyzing the information had no access to data that might allow them to identify the patients.
Statistical AnalysisA descriptive study of the data was performed using SPSS v18.
Univariate StudyFrequency and valid percent were determined in the case of the qualitative variables, detailing missing values and discarding outliers. Central tendency (mean, median), position (quartiles) and dispersion (standard deviation and interquartile range) measures were used for the quantitative variables. Data were classified for analysis into: variables on admission, during hospitalization, on discharge, and follow-up at 30 and 90 days.
Study of “Missing Values”The percentage of NOT RECORDED and NO as a response in each of the questions collected was considered to detect the variables least recorded in each center.
Bivariate StudyBivariate analysis was performed to assess differences in the information collected according to the type of hospital. The difference between groups and hospital stay, severity, mortality and readmission variables was determined using the Chi-squared test (in the case of comparison between qualitative variables) or Fisher's test (if the frequency observed was less than 5). In the case of ordinal variables, the linear trend was calculated using Kendall's Tau-c coefficient. The ANOVA test was used for quantitative variables, assessing the linear trend using the Pearson/Spearman correlation test. A P value <.05 was considered significant.
A preliminary study on possible confounding and interaction factors was conducted, adjusting for clinical or bibliographically relevant variables. Interaction was studied using the likelihood ratio. Finally, a multivariate linear regression model was created to detect hospital stay variables. The following variables were entered in the final model: hospital level, age, admissions during the previous year, and number of comorbidities as independent variables.
Finally, possible factors related with mortality and hospital readmission at 30 and 90 days were analyzed using multivariate logistic regression models, adjusted for severity of COPD, measured as use of long-term home oxygen therapy and FEV1 levels (%).
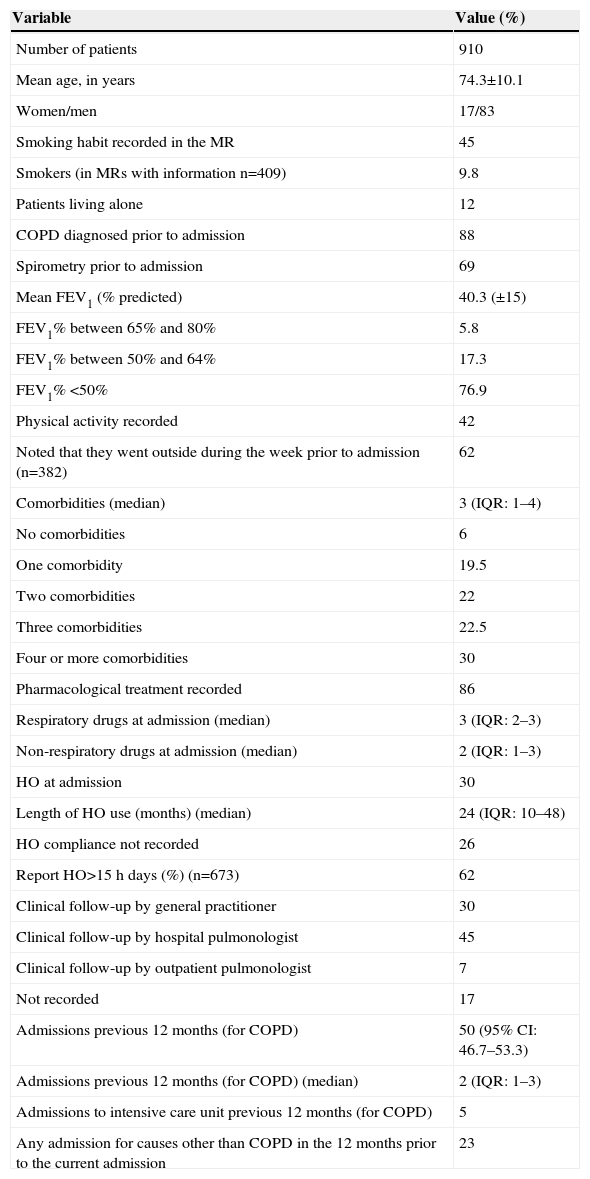
ResultsResponse Rate and General CharacteristicsOf the 48 hospitals contacted, 30 (62.5%) agreed to take part in the study. A total of 910 patients were included, which accounts for more than 70% of the target population. The distribution of responses represents all healthcare regions, in accordance with the population. Mean patient age was 74.3 (+10.1) years; 83% were men. Current smokers made up 45% of cases, and of these, 9.8% continued to smoke. A total of 88% had been previously diagnosed with COPD, although previous spirometric data were recorded in only 65% of medical records. Table 1 describes the general characteristics of the patients evaluated.
General Characteristics of Study Patients.
| Variable | Value (%) |
|---|---|
| Number of patients | 910 |
| Mean age, in years | 74.3±10.1 |
| Women/men | 17/83 |
| Smoking habit recorded in the MR | 45 |
| Smokers (in MRs with information n=409) | 9.8 |
| Patients living alone | 12 |
| COPD diagnosed prior to admission | 88 |
| Spirometry prior to admission | 69 |
| Mean FEV1 (% predicted) | 40.3 (±15) |
| FEV1% between 65% and 80% | 5.8 |
| FEV1% between 50% and 64% | 17.3 |
| FEV1% <50% | 76.9 |
| Physical activity recorded | 42 |
| Noted that they went outside during the week prior to admission (n=382) | 62 |
| Comorbidities (median) | 3 (IQR: 1–4) |
| No comorbidities | 6 |
| One comorbidity | 19.5 |
| Two comorbidities | 22 |
| Three comorbidities | 22.5 |
| Four or more comorbidities | 30 |
| Pharmacological treatment recorded | 86 |
| Respiratory drugs at admission (median) | 3 (IQR: 2–3) |
| Non-respiratory drugs at admission (median) | 2 (IQR: 1–3) |
| HO at admission | 30 |
| Length of HO use (months) (median) | 24 (IQR: 10–48) |
| HO compliance not recorded | 26 |
| Report HO>15h days (%) (n=673) | 62 |
| Clinical follow-up by general practitioner | 30 |
| Clinical follow-up by hospital pulmonologist | 45 |
| Clinical follow-up by outpatient pulmonologist | 7 |
| Not recorded | 17 |
| Admissions previous 12 months (for COPD) | 50 (95% CI: 46.7–53.3) |
| Admissions previous 12 months (for COPD) (median) | 2 (IQR: 1–3) |
| Admissions to intensive care unit previous 12 months (for COPD) | 5 |
| Any admission for causes other than COPD in the 12 months prior to the current admission | 23 |
COPD: chronic obstructive pulmonary disease; HO: home oxygen therapy; interquartile range; MR: medical record; IQR.
The patient's first assessment in the emergency department was performed by a nurse in 52% of cases and by a doctor in 28.6%; this information was not recorded in 19.4%.
Information on dyspnea was not collected in 32% of cases at the time of admission. The respiratory rate was recorded in 52% of patients and the temperature in 85%. Arterial blood gas (ABG) measurement was performed in 80% of cases. The median time from arrival at the emergency department until the ABG was performed was 1h (IQR: 0.3–2.1). FiO2 was recorded at the time the sample was taken in 52% of the ABGs performed; this was 21% in 70% of the ABGs. The mean values obtained were pH 7.41±0.07, PO2 60±10mmHg and PCO2 48±15mmHg. The pH was less than 7.35 in 14.5% of cases. Pulse oximetry was recorded in 74% of patients. Only 25 patients (2.5%) did not have ABG or pulse oximetry on admission.
No changes were recorded in the quantity or color of sputum in 28% and 27% of cases, respectively. Sputum gram staining was carried out in 32%, and cultured in 94% of these cases. Chest X-ray was performed in 99.5% of cases, ECG in 69% and routine laboratory tests in 93%.
Admission DataPatients were admitted from the emergency department to internal medicine (47%), respiratory medicine (37%) and other departments (12%), and 4% were included in a hospital-at-home program. The median time from arrival at the emergency department to admission was 10h (IQR: 5–23); 22% of patients remained there for more than 24h. A total of 9.6% of patients were treated with NIV, which was started in the emergency department in 57% of cases.
Mean hospital stay was 8.3 (7.7) days, with a median of 7 days (IQR: 4–10). The mean stay was longer than 8 days in 33.4% of patients, between 5–8 days in 37.4% and less than 5 days in 29.2%.
Care During Admission and Discharge StatusAdministration of a sedative or hypnotic between arrival at the emergency department and discharge was recorded in 19% of cases. According to the information available, the patient was confined to bed for a median of 2 days (IQR: 1–3).
On discharge, the mean number of respiratory drugs prescribed was 3.8 (+1.8), and 1.4 (+1.4) in the case of non-respiratory drugs. At discharge, 62% of patients were receiving 4 or more drugs related with their respiratory disease (at the time of admission, 21.7% of patients were receiving 4 or more respiratory drugs). There were no significant differences between admission and discharge as regards the number of non-respiratory pharmacological treatments.
Of the patients admitted to hospital for AECOPD, 80.2% were discharged home, 7% continued their hospital-at-home program, 5.6% were transferred to a nursing home, 2.8% to other care systems and 4.4% died during admission.
Ninety-five percent of patients received a discharge report. An appointment for a follow-up visit within 2 months was recorded in 35% of patients, 40% of these with the hospital pulmonologist, 34% with their general practitioner, and 26% to others. The discharge report recommended smoking cessation in all of the active smokers (100%), specifying recommendations on diet in 21%, physical activity in 13%, alcohol consumption in 3%, and on dealing with exacerbations in 11%. The inhalation technique was noted as reviewed in 24% of discharges, detection of social problems was noted in 20%, and there was a formal mechanism to ensure continuity of care in 24% of cases.
ABG was performed at discharge in 21% of patients; test conditions were indicated in 83% of cases, and in 77% of these it was performed in baseline conditions. The mean ABG values available at discharge were: pH 7.42±0.04, PO2 64.5±13mmHg and PCO2 49±9.7mmHg. Pulse oximetry at discharge was recorded in 61%. Home NIV was maintained in 3% of patients after discharge, and 46 patients were prescribed home oxygen therapy for the first time.
Follow-upThe overall mortality, from admission in the emergency department to 90 days after discharge, was 12.4%, while hospital readmissions were 25% at 1 month and 49% at 3 months, 74% due to respiratory causes.
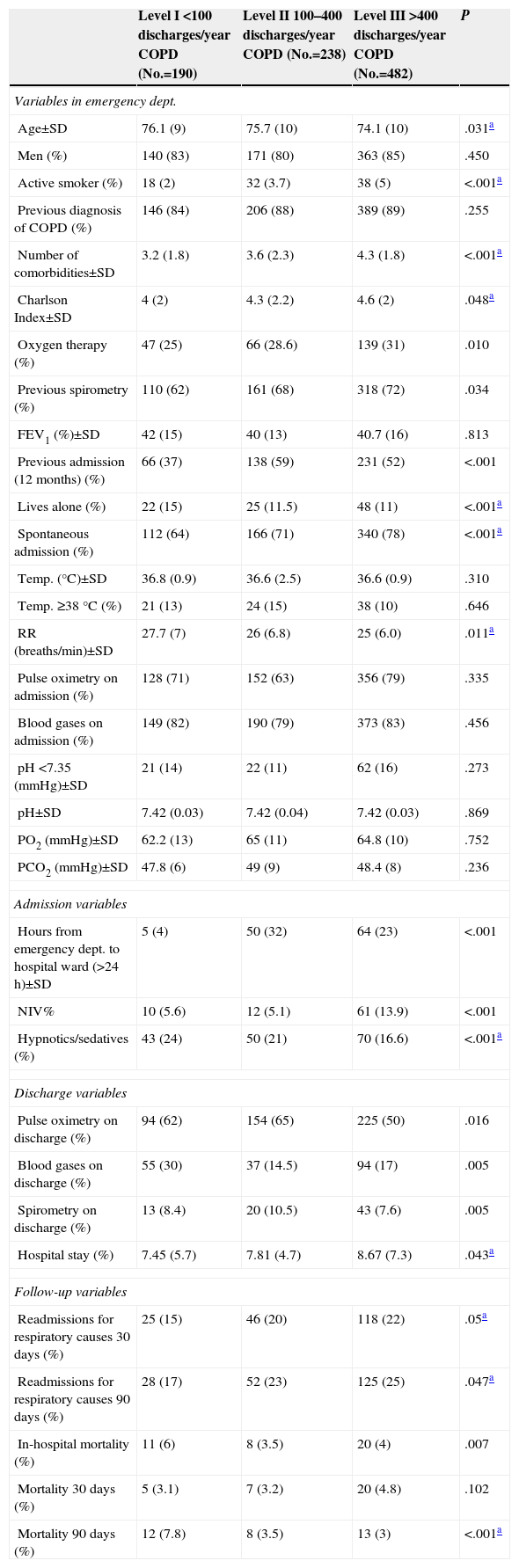
Differences According to Type of HospitalOf the patients studied, 190 (21%) were admitted to level I hospitals, 238 (26%) to level II hospitals and 482 (53%) to level III centers. The mean lung function did not differ significantly between different hospital levels, although patients admitted to level III hospitals were more frequently on home oxygen therapy (P=.01). Objective assessment at discharge (ABG or forced spirometry) was significantly lower in type III hospitals. Level III hospitals attended patients with a higher number of comorbidities (P<.001), and significantly longer stays (linear P=.020). This difference remained after adjusting for hospital level, age, admissions in the previous year and number of comorbidities in a multivariate linear regression model, with the stay increasing by 0.8 days as the hospital level increased (P=.049). The other variables analyzed are detailed in Table 2.
Differences According to the Type of Hospital.
| Level I <100 discharges/year COPD (No.=190) | Level II 100–400 discharges/year COPD (No.=238) | Level III >400 discharges/year COPD (No.=482) | P | |
|---|---|---|---|---|
| Variables in emergency dept. | ||||
| Age±SD | 76.1 (9) | 75.7 (10) | 74.1 (10) | .031a |
| Men (%) | 140 (83) | 171 (80) | 363 (85) | .450 |
| Active smoker (%) | 18 (2) | 32 (3.7) | 38 (5) | <.001a |
| Previous diagnosis of COPD (%) | 146 (84) | 206 (88) | 389 (89) | .255 |
| Number of comorbidities±SD | 3.2 (1.8) | 3.6 (2.3) | 4.3 (1.8) | <.001a |
| Charlson Index±SD | 4 (2) | 4.3 (2.2) | 4.6 (2) | .048a |
| Oxygen therapy (%) | 47 (25) | 66 (28.6) | 139 (31) | .010 |
| Previous spirometry (%) | 110 (62) | 161 (68) | 318 (72) | .034 |
| FEV1 (%)±SD | 42 (15) | 40 (13) | 40.7 (16) | .813 |
| Previous admission (12 months) (%) | 66 (37) | 138 (59) | 231 (52) | <.001 |
| Lives alone (%) | 22 (15) | 25 (11.5) | 48 (11) | <.001a |
| Spontaneous admission (%) | 112 (64) | 166 (71) | 340 (78) | <.001a |
| Temp. (°C)±SD | 36.8 (0.9) | 36.6 (2.5) | 36.6 (0.9) | .310 |
| Temp. ≥38°C (%) | 21 (13) | 24 (15) | 38 (10) | .646 |
| RR (breaths/min)±SD | 27.7 (7) | 26 (6.8) | 25 (6.0) | .011a |
| Pulse oximetry on admission (%) | 128 (71) | 152 (63) | 356 (79) | .335 |
| Blood gases on admission (%) | 149 (82) | 190 (79) | 373 (83) | .456 |
| pH <7.35 (mmHg)±SD | 21 (14) | 22 (11) | 62 (16) | .273 |
| pH±SD | 7.42 (0.03) | 7.42 (0.04) | 7.42 (0.03) | .869 |
| PO2 (mmHg)±SD | 62.2 (13) | 65 (11) | 64.8 (10) | .752 |
| PCO2 (mmHg)±SD | 47.8 (6) | 49 (9) | 48.4 (8) | .236 |
| Admission variables | ||||
| Hours from emergency dept. to hospital ward (>24h)±SD | 5 (4) | 50 (32) | 64 (23) | <.001 |
| NIV% | 10 (5.6) | 12 (5.1) | 61 (13.9) | <.001 |
| Hypnotics/sedatives (%) | 43 (24) | 50 (21) | 70 (16.6) | <.001a |
| Discharge variables | ||||
| Pulse oximetry on discharge (%) | 94 (62) | 154 (65) | 225 (50) | .016 |
| Blood gases on discharge (%) | 55 (30) | 37 (14.5) | 94 (17) | .005 |
| Spirometry on discharge (%) | 13 (8.4) | 20 (10.5) | 43 (7.6) | .005 |
| Hospital stay (%) | 7.45 (5.7) | 7.81 (4.7) | 8.67 (7.3) | .043a |
| Follow-up variables | ||||
| Readmissions for respiratory causes 30 days (%) | 25 (15) | 46 (20) | 118 (22) | .05a |
| Readmissions for respiratory causes 90 days (%) | 28 (17) | 52 (23) | 125 (25) | .047a |
| In-hospital mortality (%) | 11 (6) | 8 (3.5) | 20 (4) | .007 |
| Mortality 30 days (%) | 5 (3.1) | 7 (3.2) | 20 (4.8) | .102 |
| Mortality 90 days (%) | 12 (7.8) | 8 (3.5) | 13 (3) | <.001a |
Results are shown as mean±SD or %.
COPD: chronic obstructive pulmonary disease; NIV: non-invasive mechanical ventilation; RR: respiratory rate; SD: standard deviation; Temp.; temperature.
Analysis of the 30- and 90-day readmission variables for respiratory problems showed an inverse linear relationship between the number of readmissions and length of stay. As the length of the hospital stay increased, the number of admissions at 90 days for respiratory causes decreased (r=−0.152; P=.039). The logistic regression model also showed that patients with a previous diagnosis of COPD were less likely to be readmitted (OR=0.406; P=.015); this was also true of those on long-term home oxygen therapy (OR=0.406; P=.015) and with better FEV1 values (OR=0.977; P=.010), while age increased the likelihood of readmission (OR=1.028; P=.051). Regular physical activity was more frequently found in patients who were not readmitted than in the rest (71% vs 58%; P=.028). We did not observe any relationship between the risk of readmission and living alone. Inclusion in a hospital-at-home program reduced the probability of readmission at 30 days (5.7% vs 13%; P=.002), but not at 90 days.
Factors that increased the probability of dying at 30 and 90 days were age (OR=1.110; P=.004) and length of hospital stay (OR=1.214; P≤.001).
DiscussionOur results confirm and build on those of other recent studies conducted in different geographical areas, underlining the differences between hospitals in terms of care strategies and results obtained in EACOPD admissions, as well poor adherence to treatment guidelines.17–19 This study, like others based on clinical audits, enables weak points in healthcare to be identified, based on analysis of data obtained from routine clinical practice. The response rate was good, and different hospital levels and healthcare regions were well represented. These factors allowed us to identify key points in the care process that can help define strategies for improvement.
One of the shortcomings of our study is the quality of information in basic medical records. Spirometric data was only available in 65% of cases. This percentage is higher than that observed by Pellicer et al.20 in the Valencia region of Spain (45%) and by Roberts et al. (42%)21 and Pretto et al. (34%)22 in the UK and Australia, respectively, and very similar to those found in Canada and in a European audit.23,24 Forty-five percent of medical records did not contain information on smoking habits. Data collection in the emergency department was inconsistent and incomplete, particularly as regards the respiratory rate (52%) and information on the conditions in which the ABG was performed (the FiO2 of the ABG was known to be 0.21 in fewer than one third of patients).
Analysis of care process variables revealed opportunities for improvement in care time management: it took a long time to perform the ABG (median time was 1h, but it took more than 2h in 25% of patients), and 22% of patients who were admitted remained in the emergency department for more than 24h.
General practitioners (GPs) play a very important role in the management of COPD. Thirty percent of patients admitted are only seen by their GP, while this was true of 18% of patients the EFRAM study.25 Only 37% of patients admitted were treated in respiratory medicine wards, and in 57% of cases, NIV was initiated in the emergency department without the direct intervention of a pulmonologist.
More than one third of patients remained in hospital for more than 8 days, and only 4% of patients benefited from alternatives to conventional hospitalization, despite the positive results shown for hospital-at-home programs in our setting.26
The discharge reports of patients admitted for COPD exacerbations contain insufficient recommendations on physical exercise (13%), how to deal with new exacerbations (11%) and use of inhalers (24%). In the case of active smokers, there was a formal recommendation in all cases to quit smoking, but specific treatment was not recorded. ABG at discharge is predictive of future exacerbations, and we noted that it only appeared in 21% of cases. Hypercapnia at discharge is a factor that increases the risk of readmission at 1 year.27,28 Neale et al.29 observed that 18% of the adverse events in 2 university hospitals in London occurred at the time of discharge, therefore more clinical importance should be given to the content of the discharge report.
Hospital admission has a direct impact on the medication received by the patient. After admission, the number of patients with 4 or more prescriptions for drugs related with their respiratory disease had increased three-fold.
Comparing MAG-1 data with other similar studies (UK COPD Audit 200830 and the European COPD Audit 201231) showed that patient characteristics (mean age over 72 years and median FEV1 less than 41%, with previous admissions in more than 50% of cases) and medium-term results (mortality and readmissions) were largely similar, although in the UK the mean stay is shorter, there are more alternatives to conventional hospitalization, and some records are better (e.g. records of smoking habits). All 3 audits found that more than one third of patients were readmitted 90 days after discharge, and more than 12% died. All 3 record a high percentage of patients admitted for COPD exacerbation in whom previous spirometry results were not available (>40% in all cases).
Analyzing the differences between hospitals, we observed that patients admitted to type III hospitals (with more than 400 discharges per year for exacerbation) had more severe illness compared to other hospitals. They were younger, with more comorbidities, and a higher percentage of patients received home oxygen. The percentage of patients with severe COPD was also higher. However, lung function in the group of patients treated at each center (measured via the FEV1%) and the percentage of patients with pH <7.35 was largely similar in all types of hospital. The mean stay was longer and readmissions significantly higher in type III hospitals.32
Some of these factors could have a bearing on higher mortality rates in type I hospitals (an increase in mortality could partially explain the reduction in readmissions). However, further analysis is required to explain these data, as non-respiratory causes (e.g. aging and a higher percentage of patients who live alone) could affect the increase in mortality in type I hospitals.
The hospital stay was longer as the complexity of the hospital and number of discharges for COPD exacerbation increased. It is hard to find objective arguments to explain this trend. However, the higher number of professionals involved in the treatment of these patients in level III hospitals could explain these differences. Patients more likely to be readmitted were older, had lower FEV1%, shorter stays, no objective diagnosis of COPD, and no home oxygen.
As regards mortality, age and length of stay were the variables best related with mortality at 90 days. The role of the comorbidity must be carefully considered when analyzing factors related with mortality.33
Clinical audits are a good method for benchmarking healthcare organizations. However, they sometimes yield little information on essential interventions to improve the care process. Over-generalized information or extensive delays between analysis and reporting are of little use for taking decisions. The challenge consists of identifying which key aspects of the process affect results, and implementing processes for improving the quality of care. The first goal should be to improve the quality of information recorded in the medical records, in terms of both diagnosis (lung function and smoking) and functional situation on discharge (ABG), as well as specific treatment recommendations.
Conflict of InterestThe authors state that they do not have any conflicts of interest directly or indirectly related with the contents of the manuscript.
Escarrabill J. Hospital Clínic (Barcelona).
Hernández C. Hospital Clínic (Barcelona).
Jiménez J. Servei Català de la Salut (CatSalut).
Llauger MA, EAP Encants. Institut Català de la Salut. (Barcelona).
Roger N. Consorci Hospitalari de Vic. Vic (Barcelona).
Rosas A. Departamento de Salud (Generalitat de Catalunya).
Torrente E. Departamento de Salud (Generalitat de Catalunya).
Tresserras R. Departamento de Salud (Generalitat de Catalunya).
Saltó E. Agència de Salut Pública. Departamento de Salud (Generalitat de Catalunya).
MAG-1 Working Group
- •
Carme Santiveri Gilabert, Rafael Calvet Madrigal y Olga Delgado. Hospital Dos de Maig
- •
Nuria Roger Casals y Joan Serra Batlles. Hospital General de Vic
- •
Beatriz Lara y Cristina Esquinas. Hospital Universitari Arnau de Vilanova de Lérida
- •
Marta Rodó Muñoz. Hospital Comarcal Sant Jaume de Calella
- •
Carles Sabadell Nieto, Rosa Jolis Olivè, Marc Bonnin Vilaplana. Hospital de Figueres Fundació Privada
- •
Amalia Moreno, Laia Setó y Eduard Monsó. Hospital Universitari del Parc Taulí de Sabadell
- •
Virginia Pajares Ruiz, Vicente Plaza Moral. Hospital de la Santa Creu i Sant Pau
- •
Jesus Ribas Sola, Salud Santos Pérez, Jordi Dorca Sargatal. Hospital Universitari de Bellvitge
- •
Carles Prats Sánchez, Noelia Pablos Mateos, Jordi Esplugas Abós. Hospital Sant Joan de Déu de Martorell
- •
Nuria Celorrio Jiménez, Joan Anton Lloret Queraltó, Mercè Palau Benavent. Hospital de Viladecans
- •
Júlia Tàrrega Camarasa, Yolanda Galea Colon, Enric Barbeta Sànchez. Hospital General de Granollers
- •
Luis Lores Obradors. Hospital de Sant Boi
- •
Antoni Sancho-Muñoz, Roser Pedreny, Joaquim Gea. Hospital del Mar - IMIM. UPF. Barcelona.
- •
Yoni Loza Medrano, Eugeni Rodríguez Flores, Miquel Torres Salinas. Fundació Hospital de l’Esperit Sant.
- •
Angels Barrio, Eugenia Bueno, Esther Rodríguez. Hospital Universitari General de la Vall d’Hebron.
- •
Sílvia Molina. Hospital de Campdevànol.
- •
Concepción Cañete Ramos. Hospital General de L’Hospitalet.
- •
Carmen Abeledo Núñez y Josep M. Vidal Balañà. Fundació Hospital Residència Sant Camil.
- •
Antònia Llunell Casanovas, César Valdés Castiello. Hospital de Terrassa.
- •
José Alberto Martos Velasco. Hospital San Rafael.
- •
Jesús Alvarez Albó, Esther Salvador Milian, Eduard Sanjurjo Golpe. Hospital Comarcal del Pallars.
- •
Salvador Hernàndez Flix, Anna M. Texidó Bruguera, Luis Fernando Casas Méndez. Hospital Universitari Sant Joan de Reus.
- •
Sandra Sangenís Diez y Raquel Català Perez. Hospital Sant Joan de Reus.
- •
Óscar Ros Garrigos. Hospital Comarcal Móra d’Ebre.
- •
Carme Viñas, Pere Almagro. Hospital Universitario Mútua de Terrassa.
- •
Vicenta Bisbe Company y Joan Carles Trullàs Vila. Hospital Sant Jaume d’Olot.
- •
Elena Caldentey Ysern. Hospital de Sant Pau i Santa Tecla de Tarragona.
- •
Carme Josep Candelich y María del Pilar Ortega Castillo. Hospital de Mataró.
- •
Maria Josep Cardona Iguacen y Erika Tavera Gomez, Hospital d’Igualada.
- •
Emili Marquilles, Óscar Bernadich, Anna Capsada y Amalia Molina. Centre Hospitalari de Manresa.
- •
Rebeca Domingo, Nuria Seijas y Néstor Soler. Hospital Clinic i Provincial de Barcelona.
The list of group members found in Appendix.
Please cite this article as: Escarrabill J, Torrente E, Esquinas C, Hernández C, Monsó E, Freixas M, et al. Auditoría clínica de los pacientes que ingresan en el hospital por agudización de EPOC. Estudio MAG-1. Arch Bronconeumol. 2015;51:483–489.