Pneumoconioses are a group of interstitial lung diseases secondary to the inhalation and deposition of inorganic dusts. Classic forms include silicosis, asbestosis, and coal workers’ pneumoconiosis, although less common entities related to atypical occupational exposures have also been described. Calcium stearate, a metallic salt of stearic acid, is widely used as a lubricant and anti-caking agent in the plastics industry, paints, pharmaceuticals, cosmetics, and in metallurgical processes such as wire drawing. It has traditionally been considered a compound of low toxicity and, to date, no cases of pneumoconiosis with mineralogical confirmation attributable to its inhalation have been published.
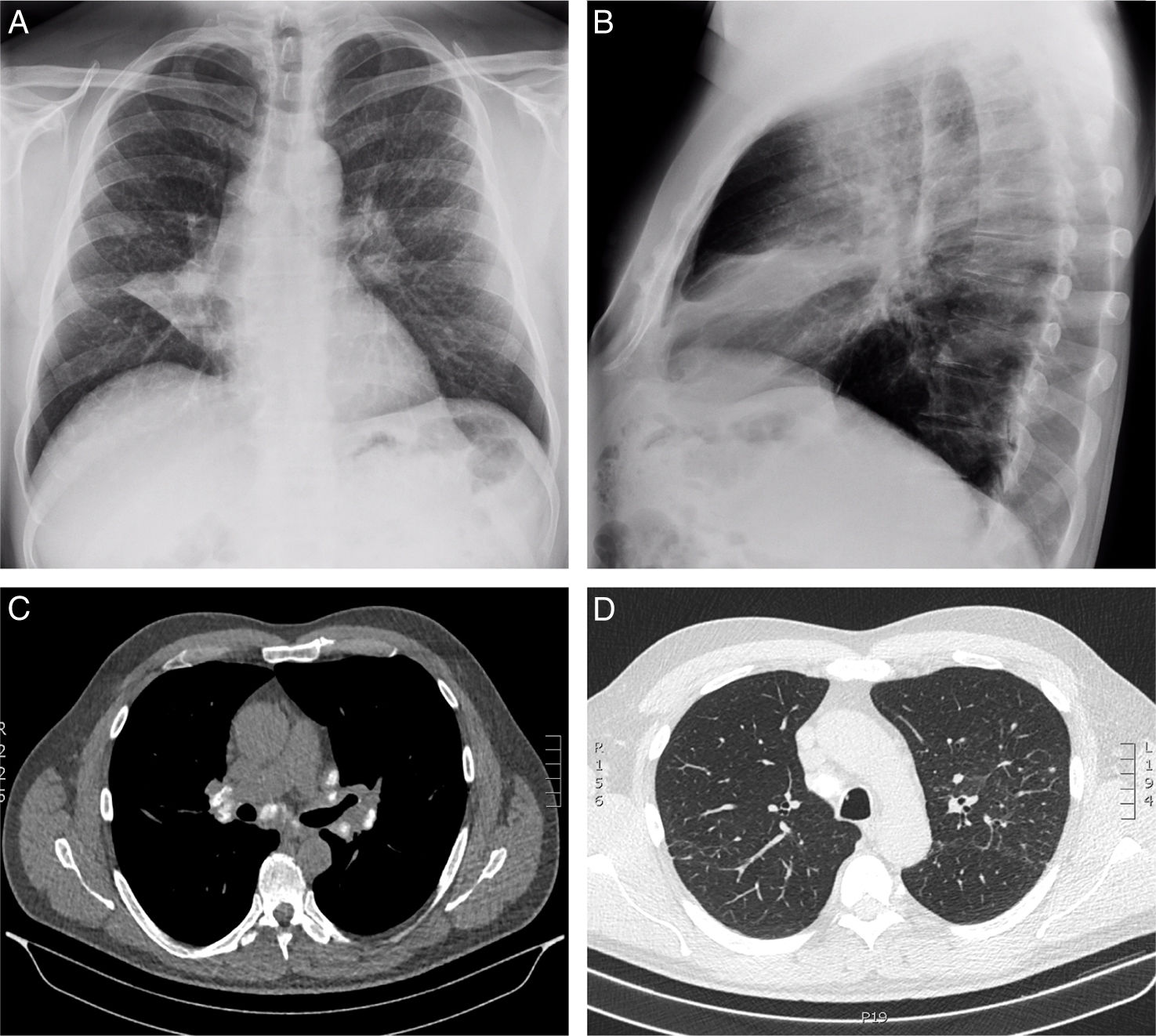
We report the case of a 60-year-old man, a wire-drawing worker with 29 years of occupational exposure to calcium stearate, who presented to the Pulmonology Department with pleuritic pain in the right hemithorax. Spirometry values were within normal limits. Chest radiography revealed bilateral reticulonodular opacities, hilar lymphadenopathy, and increased density with atelectasis of the middle lobe. CT scan showed a partially calcified progressive massive fibrosis mass in the right upper lobe with major fissure retraction, a bilateral micronodular interstitial pattern, and calcified mediastinal and hilar lymphadenopathy (Fig. 1). Bronchoscopy demonstrated partial stenosis of the middle lobe bronchus due to extrinsic compression. Bronchoalveolar lavage (BAL) was performed in the lingula, and five transbronchial cryobiopsies were obtained from the left upper lobe. BAL cytology showed: neutrophils 51%, lymphocytes 32%, eosinophils 8%, macrophages 4%, with a CD4/CD8 ratio of 2.04. Histological examination (Masson's stain) revealed peribronchiolar fibrosis, granulomas with multinucleated giant cells (CD68 positive), and an inflammatory infiltrate (CD45 positive), with no evidence of malignancy. Mineralogical analysis by infrared spectroscopy identified calcium stearate in lung tissue, establishing the diagnosis of pneumoconiosis due to calcium stearate. The patient was referred to the Occupational Pulmonology Unit for follow-up.
(A) Posteroanterior and (B) lateral chest radiographs showing bilateral reticulonodular opacities, hilar lymphadenopathy, and increased density with middle lobe atelectasis. (C) Chest CT scan in mediastinal window showing calcified mediastinal and hilar lymph nodes bilaterally. (D) Chest CT scan in lung window showing a bilateral micronodular interstitial pattern.
Classical pneumoconioses are well characterized, but new entities continue to be reported in association with industrial dusts previously considered innocuous [1,2]. In this context, calcium stearate, despite its widespread industrial use and classification as a low-toxicity compound, is shown in this case to induce granulomatous inflammation and pulmonary fibrosis. The probable pathophysiology involves macrophage activation leading to granuloma formation and progression to fibrosis, paralleling observations in other pneumoconioses [3]. The use of techniques such as cryobiopsy and mineralogical analysis was particularly useful in this case to exclude malignancy and to establish the occupational etiology [4]. In conclusion, we present the first reported case of pneumoconiosis due to calcium stearate with mineralogical confirmation, emphasizing the importance of considering non-classical industrial exposures in the differential diagnosis of pulmonary lesions and the utility of advanced tissue analysis techniques in atypical presentations.
AuthorshipBoth authors contributed substantially to the conception, drafting, and revision of the manuscript and approved its final version for submission.
Ethical approvalOur institution does not require ethical approval for reporting individual cases or case series.
Informed consentWritten informed consent was obtained from the patient for the anonymous information to be published in this article.
Use of artificial intelligenceArtificial intelligence tools were not used in the generation of the manuscript's content, data analysis, or figure creation.
FundingThe authors declare that they received no financial support for the research, authorship, and/or publication of this article.
Conflicts of interestThe authors declare that there are no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.