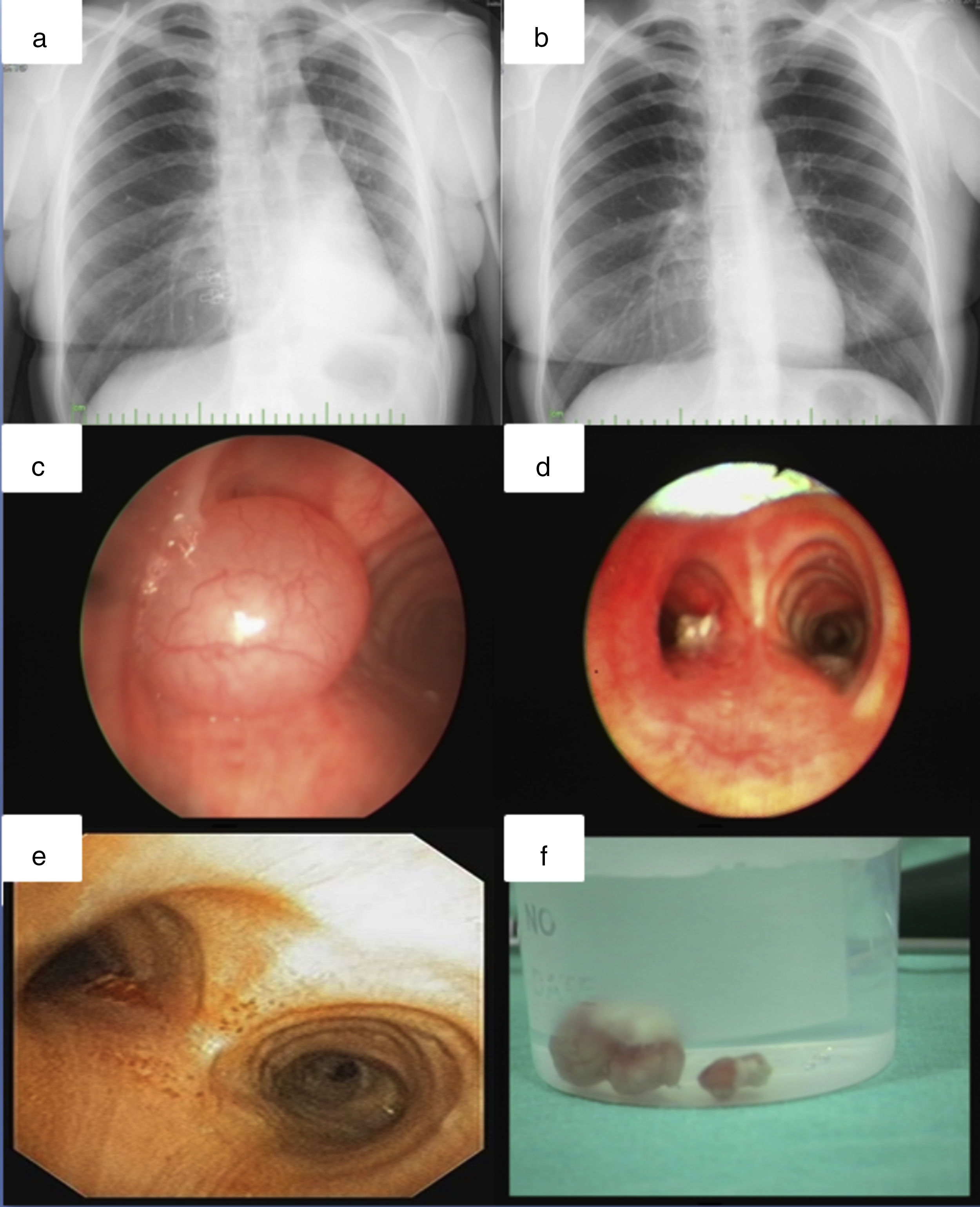
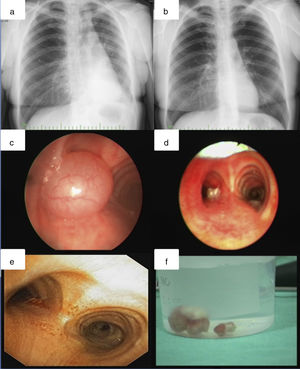
Hamartomas are benign tumor-like malformations which was originally described by Albrecht.1 Hamartomas of the lung can be pulmonary or endobronchially. A 37-year-old female was admitted to our hospital with a 3-month history of progressive dyspnea. She had a 20 pack-year smoking history. Physical examination revealed decreased respiratory sounds in the left lung field. The chest X-ray showed atelectasis of the left lower lobe (Fig. 1a). Computed tomography revealed a 2cm×3cm×1.5cm homogeneous mass, obstructing the left lower bronchus. Rigid bronchocopy was done for diagnosis and treatment to maintain airway safety. A vegetating, pedunculated lesion covered with a normal bronchial epithelium was observed obstructing the entrance of the left main bronchus (Fig. 1c). Distal bronchus was observed to be patent. The tumor was extracted with the snare prob and cryotherapy was applied to the base of the tumor (Fig. 1d). Postoperatively, the dyspnea subsided and the atelectasis in the left lower lobe disappeared (Fig. 1b). Pathological examination of the tumor provided a diagnosis of hamartoma (Fig. 1f). In the control broncoscopy done 1 month later, a tumoral surface containing a cartilaginous component was observed 1cm distally from the main carina at the posteromedial wall. Cryotherapy was applied to the base of the lesion but because of the cartilaginous component it was ineffective (Fig. 1e). The patient is on follow-up and asymptomatic. Hamartomas are the most common benign pulmonary neoplasms but of them only 10% are endobronchial.2 Usually patients are at their 6th decade at the time of diagnosis and a male predominance (4 to 1) is observed.3 In case series no difference in the bronchial distribution was observed.4 Most endobronchial hamartomas were asymptomatic but they can also present with hemoptysis, cough or dyspnea, or with radiological findings of pneumonia, atelectasis, and intrabronchial tumor.4 Some endobronchial hamartomas presented with symptoms and findings of airway obstruction that resembled bronchogenic carcinoma.. Like our case, most of them originated from a larger bronchi, growing into the lumen and obstructing the airway.4 The management of these tumors by endobronchial interventions can be diagnostic and therapeutic in a same session. Heat-based methods like laser or argon plasma coagulation are recommended for endobronchial hamartomas, especially in symptomatic patients.4,5 Early removal of these tumors is important before the occurrence of parenchymal findings. Therefore, bronchoscopic interventional approach for endobronchial hamartomas not only controls symptoms but also can might avoid the need for thoracotomy. Surgical therapy should be reserved for cases where the hamartomas cannot be approached by endoscopy. In our case, our patient benefited from endobronchial treatment due to the location of the lesion and surgery was avoided.
Chest X-ray before (a) and after intervention (b), showing disappearance of left lower lobe atelectasis. On bronchoscopy (c), a vegetating, pedunculated lesion covered with a normal bronchial epithelium was obstructing the left main bronchus. Bronchoscopic view after resection (d) and after one month (e). Resected material (f).