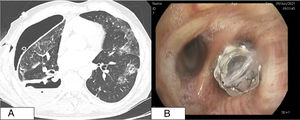
We report the case of a 62-year-old man, smoker (45 pack-years), with COPD and recent diagnosis of right lower lobe epidermoid lung carcinoma T4N2M0 (stage IIIB), receiving chemotherapy and radiation therapy. He was admitted for right hydropneumothorax and a chest tube was placed. His subsequent progress was poor, with Staphylococcus aureus empyema and persistent air leak, diagnosed as a bronchopleural fistula (Fig. 1A). Endoscopic treatment was performed using a Zephyr one-way endobronchial valve in the right lower lobe. Seven days later, the air leak occurred again, so the bronchoscopy was repeated, showing cranial displacement of the valve at the entrance of the right basal segment. In this position, it was ineffective (Fig. 1B), so it was removed. Fibrinoid and purulent material, observed distal to the valve, was removed. The pleural cavity was accessed, giving a view of the parietal and diaphragmatic pleura, both of which were thickened and had an infiltrative appearance, and of the correctly positioned chest tube (Appendix B video). Bronchopleural fistula has a poor prognosis (mortality 0.05%–27%).1 The most important risk factors are age, diabetes mellitus, necrotizing lung infection, COPD, chronic corticosteroid treatment, or chemoradiotherapy.2 Although the treatment of choice is surgery, carefully selected patients who are not candidates for surgery may benefit from endoscopic treatment. In our case, the patient presented acute concomitant infection in addition to the fistula, creating controversy with regard to the placement of an endobronchial valve. However, surgery was ruled out due to the patient's comorbidities, so this was the only therapeutic possibility available to control the air leak. Chemoradiotherapy could subsequently be reinitiated.
The Impact Factor measures the average number of citations received in a particular year by papers published in the journal during the two preceding years.
© Clarivate Analytics, Journal Citation Reports 2025
SRJ is a prestige metric based on the idea that not all citations are the same. SJR uses a similar algorithm as the Google page rank; it provides a quantitative and qualitative measure of the journal's impact.
See moreSNIP measures contextual citation impact by wighting citations based on the total number of citations in a subject field.
See more