Longer life expectancy and the progressive aging of the population are changing the epidemiological pattern of healthcare, with a reduction in the incidence of acute diseases and a marked increase in chronic diseases. This change brings important social, healthcare and economic consequences that call for a reorganization of patient care. In this respect, the Spanish National Health System has developed a Chronicity strategy that proposes a substantial change in focus from traditional rescue medicine to patient- and environment-centered care, with a planned, proactive, participative and multidisciplinary approach. Some of the more common chronic diseases are respiratory. In COPD, this integrated approach has been effective in reducing exacerbations, improving quality of life, and even reducing costs. However, the wide variety of management strategies, not only in COPD but also in asthma and other respiratory diseases, makes it difficult to draw definitive conclusions. Pulmonologists can and must participate in the new chronicity models and contribute their knowledge, experience, innovation, research, and special expertise to the development of these new paradigms.
La mayor expectativa de vida y el progresivo envejecimiento de nuestra población están produciendo un cambio en el patrón epidemiológico asistencial, con una disminución de las enfermedades agudas y un pronunciado aumento de las crónicas. Este importante cambio conlleva notables consecuencias sociales, sanitarias y económicas, lo que plantea la necesidad de una reordenación en la forma de atender a nuestros pacientes. En este contexto, la Estrategia para el abordaje de la cronicidad del Sistema Nacional de Salud propone un cambio de enfoque sustancial para pasar de una medicina de rescate tradicional a una medicina centrada en el paciente y su entorno, una medicina planificada, proactiva, participativa y multidisciplinar. Algunas de las enfermedades crónicas más prevalentes son de origen respiratorio. En la EPOC, esta aproximación integral ha demostrado reducir las exacerbaciones, mejorar la calidad de vida e incluso disminuir el coste. Sin embargo, la heterogeneidad de las intervenciones dificulta las conclusiones definitivas. Algo parecido sucede en asma y en otras enfermedades respiratorias. La neumología puede y debe participar de los nuevos paradigmas de la cronicidad, aportando conocimiento, experiencia, innovación, investigación y valor añadido.
Chronicity is a phenomenon that affects all healthcare workers without exception, and which poses complex challenges. These can only be overcome by changing the way healthcare systems are currently organized, introducing widespread use of information technologies and educational strategies, and involving individuals in their own healthcare. Respiratory medicine is not unaffected by these changes, as some of the chronic diseases with greatest impact are respiratory in origin. This means that respiratory medicine teams can and must participate in these new paradigms, contributing their knowledge, experience, innovation, research, and special expertise.
Throughout the twentieth and early twenty-first century, we have witnessed the development of reactive rescue medicine focused on acute processes, in which health professionals barely interact with patients, except during unstable episodes. This type of episodic care led to the development of the hospital care network, aimed at treating acute conditions, and contributed to a certain fragmentation in continuity of care. However, improvements in social and economic levels, technological development and major breakthroughs in modern medicine have brought with them longer life expectancy and an increasingly aging population, resulting in an epidemiological transition toward chronic diseases. These conditions are generally slowly progressive and long-term. They limit the health-related quality of life (HRQoL) of patients and their caregivers, are a cause of early death and have a major economic impact on families, communities and society.1 Within this context, traditional reactive rescue medicine appears to be inadequate. Care models for chronic disease must be redesigned around a more proactive, patient-centered (patient management) approach, with a greater focus on home ambulatory care and planned, multidisciplinary treatment. This will improve control of these types of diseases, facilitate coordination of care, and reduce costs.
An estimated 70% of the entire healthcare budget in Spain goes toward the care of chronically ill patients.2 This, together with the need to rationalize resources to make the system sustainable, is prompting health authorities to reconfigure the system around a new chronic care management model. In 2012, the Spanish Ministry of Health, Social Services and Equality published their National Health System (NHS) chronicity strategy,2 and almost all Spanish regions are presently rolling out local initiatives. An estimated 45.6% of the Spanish population aged over 16 years suffer from at least one chronic illness, and 22% of the population from two or more, with these figures increasing with age.3 Aging and chronic illness often overlap, and this in many cases undermines the individual's functional capacity, increasing their vulnerability and frailty, and leading to more comorbidities, higher drug use and greater need for care.
Some respiratory diseases, such as asthma or chronic obstructive pulmonary disease (COPD) in particular, are among the chronic diseases that have aroused most interest due to their huge prevalence, elevated morbidity and mortality and high costs. However, there are other chronic respiratory diseases that can be managed in the same way, such as sleep apnea–hypopnea syndrome, bronchiectasis or idiopathic pulmonary fibrosis. In this article, we will attempt to explain why the chronic care model should be changed, assess general proposals for this change, and review the evidence with respect to new care models for the most prevalent chronic respiratory diseases. Finally, we will attempt to express our opinion on the role that respiratory medicine should play in this new scenario.
Reference Models for Chronic CareDue to demographic, epidemiological and economic demands, chronic care has become a challenge for healthcare systems. The chronic care model (CCM) proposed by Wagner4 was the first integrated chronic care initiative. The model was later expanded, modified and adapted in several countries. A review of the literature yields a variety of terms that capture the essence of the CCM to a greater or lesser extent. These include integrated care, case management, home-based care and disease-management.
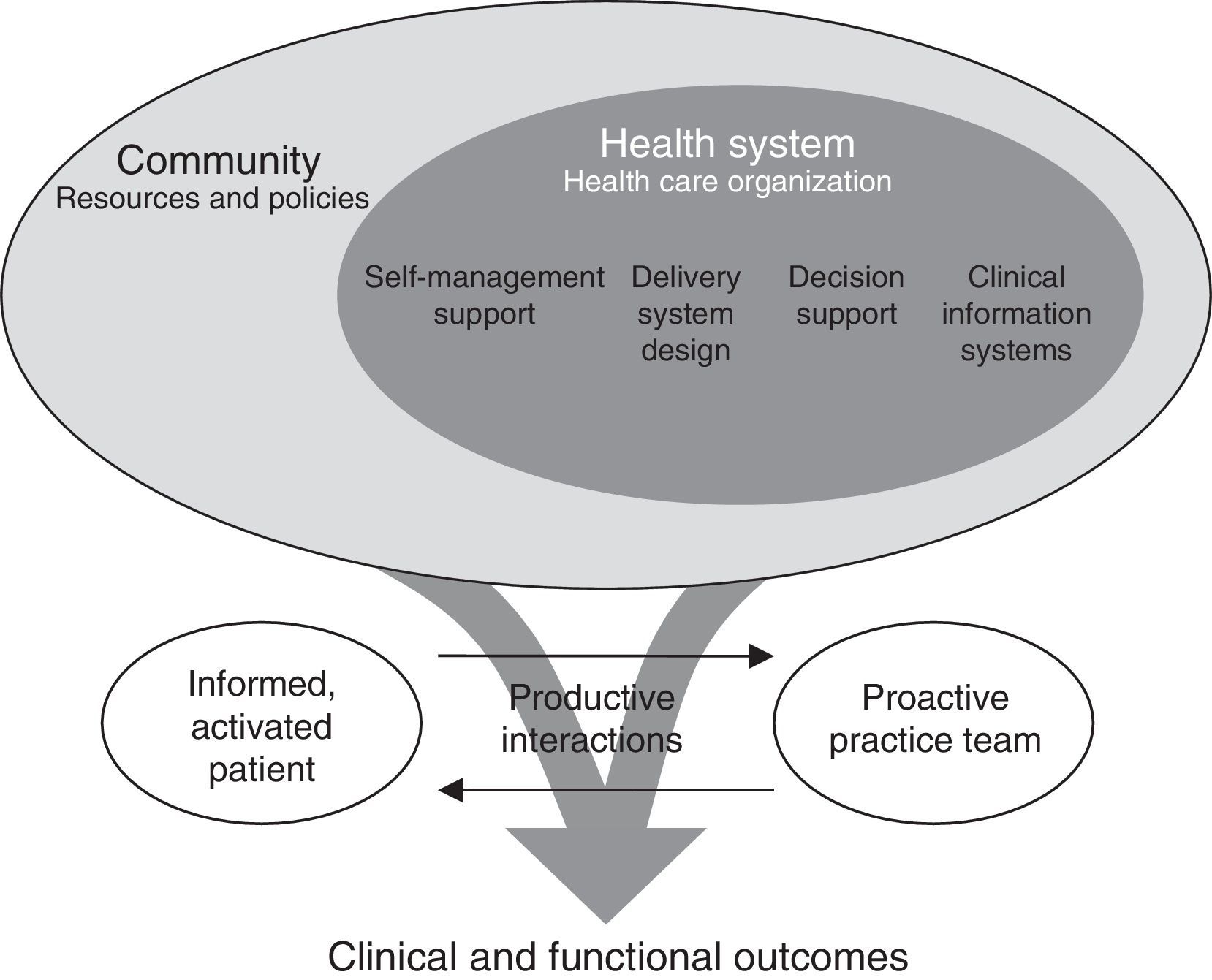
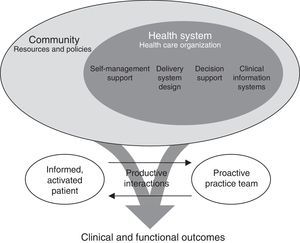
Chronic Care ModelIn 1998, Edward Wagner, then Director of the MacColl Institute for Healthcare Innovation, developed a model for patients with chronic diseases4 (Fig. 1). Broadly speaking, the model suggested the need to transform the health system to focus on improving the health of the population through a shared vision. This called for the health system and community resources, organizations and institutions to work together to prevent and manage chronic diseases. From a care point of view, it established the need to move toward proactive care models centered on a holistic view of the patient, with an integrated, coordinated and multidisciplinary approach. The CCM also proposed involving both patient and caregiver in disease management and care strategies as a means of strengthening their motivation, knowledge and self-care skills through structured healthcare education and psychosocial activities. The use of decision aids and professional training is encouraged in order to improve health outcomes. Finally, CCM considers the use of information systems as a support for clinical and population management.
Conceptual model for the care of patients with chronic diseases (chronic care model) proposed by Wagner.4
Considerable experience has been accumulated in the last decade in the use of the CCM, showing improvements in quality of care and in the primary clinical outcomes of various chronic diseases.5 These findings are consistent in different countries with different healthcare systems and approaches. Although simple interventions may be attractive, most studies show that the best outcomes are obtained when different elements of the CCM are implemented simultaneously. Despite this evidence, further information is required on the efficiency and economic implications of changes in the organization and functioning of ambulatory care. Most studies focus on patients with a single chronic illness, treated by highly motivated professionals. Whether these benefits are maintained in other settings remains to be seen.
World Health Organization Innovative Care for Chronic Conditions FrameworkIn 2002, the World Health Organization (WHO), in an effort to encourage countries to design and develop strategies to address the management of chronic illnesses, published the Innovative Care for Chronic Conditions (ICCC) Framework,6 which added a health policy perspective to the CCM. The contributions of the ICCC framework to the CCM can be explained at 3 levels. At the macro-level, it highlighted the existence of a positive political environment capable of redirecting services to cater for the demands of chronic illness. At the meso-level, the role of the community continues to be essential, and the notion of integration-coordination of services and resources is particularly emphasized. At micro-level, the interaction between the medical professional and patient is extended to the community. In general, the WHO proposal is based on 8 essential elements (Table 1).
Key Elements of the World Health Organization Proposal for Innovative Care for Chronic Conditions.
| - Support a paradigm shift |
| - Manage the political environment |
| - Build integrated health care |
| - Align sectoral policies for health |
| - Use health care personnel more effectively |
| - Center care on the patient and family |
| - Support patients in their communities |
| - Emphasize prevention |
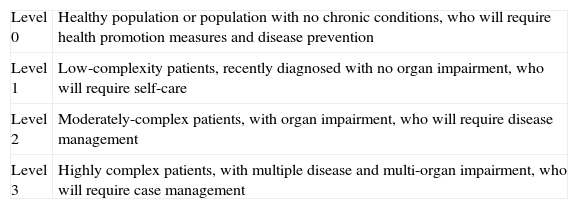
With respect to the reorganization of care, aside from the theoretical models derived from the CCM, it is essential to stratify the population in order to identify individuals at risk of disease, and to predict the needs of patients who already have a chronic illness and so optimize their care. In this regard, the most widely accepted population model is the Kaiser Permanente.7 This consists of a pyramid that stratifies the population into 4 basic levels with respect to the approach to chronic diseases and/or conditions (Table 2).
Population Risk Stratification According to Levels of Complexity Proposed by Kaiser Permanente.
| Level 0 | Healthy population or population with no chronic conditions, who will require health promotion measures and disease prevention |
| Level 1 | Low-complexity patients, recently diagnosed with no organ impairment, who will require self-care |
| Level 2 | Moderately-complex patients, with organ impairment, who will require disease management |
| Level 3 | Highly complex patients, with multiple disease and multi-organ impairment, who will require case management |
Stratification goes hand in hand with a comprehensive assessment of the medical, care, functional and social needs of patients, and individualized treatment plans. This model, improved by the King's Fund in the United Kingdom,8 was finally adopted by the Spanish National Health System's (SNHS) Chronicity Strategy.2 It aims to optimize resources by adjusting care interventions to the complexity of the patient, and ensuring a positive cost-effectiveness balance. Healthy people or those with known risk factors should be encouraged to take responsibility for their own health, and should receive education in preventive measures. Those with a low complexity chronic illness should receive self-management support. Disease management is considered for moderately complex patients needing integrated management with multidisciplinary care. Developing integrated, computerized care processes that guarantee adherence to clinical practice guidelines is probably the best approach for disease management. Computerization and decision aids seem to be essential to reduce variability, provide individualized care and monitor outcomes. Finally, case management is based on a process of individualized assessment, planning and coordination. Some new professional profiles, such as the nurse case manager, have arisen in this context. Information and communication technology may also be helpful in monitoring some of these home-care patients.
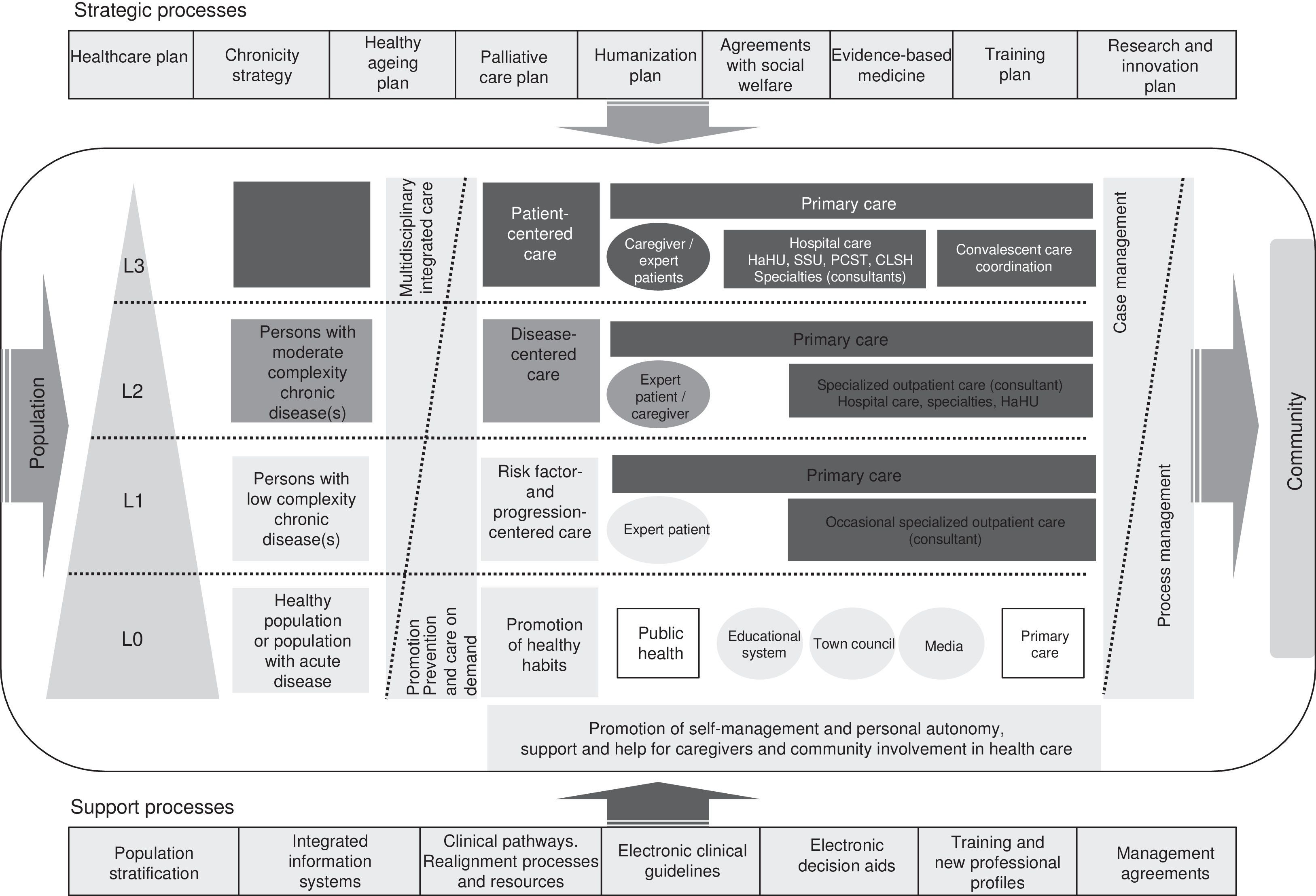
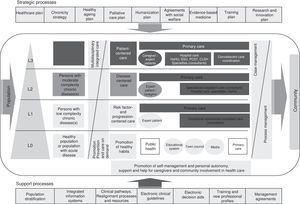
Spanish National Health System Chronicity StrategyIn 2012, the Spanish Ministry of Health published their National Health System Chronicity Strategy,2 a document that represents a change of approach in the SNHS. The new system will be patient-centered instead of disease-centered. It will address the needs of the population as a whole and each individual in particular to give the best and most efficient healthcare, guarantee continuity of care, adapt to disease progression in the patient, and encourage personal autonomy. The Strategy proposes various priority organizational changes to improve the approach to chronic disease (Table 3). Most Spanish regions have already developed their specific programs. Fig. 2 shows, by way of example, the integrated care process for chronically ill patients in the Valencia region of Spain.9
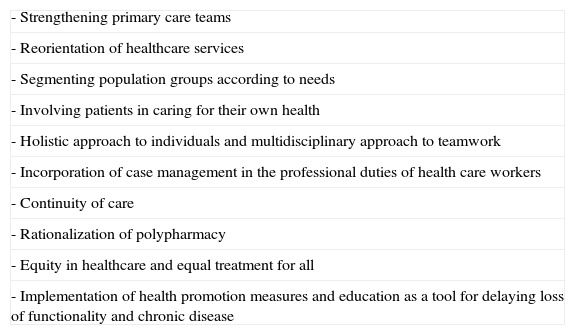
Priority Strategic Interventions for Chronic Care.
| - Strengthening primary care teams |
| - Reorientation of healthcare services |
| - Segmenting population groups according to needs |
| - Involving patients in caring for their own health |
| - Holistic approach to individuals and multidisciplinary approach to teamwork |
| - Incorporation of case management in the professional duties of health care workers |
| - Continuity of care |
| - Rationalization of polypharmacy |
| - Equity in healthcare and equal treatment for all |
| - Implementation of health promotion measures and education as a tool for delaying loss of functionality and chronic disease |
Integrated process for chronic patient care in the Valencia region of Spain. Source: Strategy for chronic patient care in the Valencia region of Spain.9
One of the chronic diseases with the greatest social, healthcare and economic impact is COPD. Its huge prevalence (10.2% of the population aged over 40 years), high mortality (fifth cause of death in Spain), frequent association with other chronic conditions, and use of resources (0.2% of the gross domestic product) make COPD a “paradigm of chronicity”.10
Although clinical practice guidelines propose a therapy maintenance approach aimed at improving symptoms and preventing risk, COPD patient care is often based on reactive rescue strategies, generally aimed at controlling exacerbations. As mentioned above, this approach is insufficient for a chronic, progressive disease involving multiple comorbidities, and in which major deficiencies have been detected. These include problems with diagnosis (both under-diagnosis, which affects 73% of COPD patients,11 and over-diagnosis, which occurs in up to 30% of our patients12), significant variability in healthcare practices,13,14 scant adherence to clinical practice guidelines with overuse of some drugs,15 poor implementation of respiratory rehabilitation therapies, the strong influence of comorbidities or the need for integrated, coordinated care. To address these issues, redesigning chronic disease management around proactive, more patient-centered (patient management) clinical practice, with greater focus on home ambulatory care and treatment planning, could potentially improve control of these types of diseases, facilitating coordination of care and reducing costs.
Despite this general approach, and although the partial or full use of the CCM has been beneficial in some settings, the fact remains that there is still little evidence to support the efficiency of these types of interventions in COPD patients. Three systematic reviews have shown clinical benefits, finding a significant reduction in both exacerbations requiring medical attention, and in the frequency of hospitalizations, improvements in exercise tolerance and shorter hospital stays.16–18 In a fourth meta-analysis, Boland et al.19 also showed a reduction in direct costs, with savings of €1060 (95% CI: €80–€2040) per patient and year in hospitalization costs and €898 (95% CI: €231–€1566) in costs derived from the use of healthcare services. However, the heterogeneity of the interventions, with underpowered pilot studies, and the scant methodological use of clinical trials make it difficult to draw definitive conclusions.
When 2 or more components of the CCM are included, the programs provide satisfactory results.16,17 However, the benefit of only including a single element is more equivocal. Educational programs and action plans have been particularly controversial. While some systematic reviews show good results,20 one recent clinical trial has even warned of an increase in mortality.21 Success, however, would appear to depend upon using these action plans within an integrated program that seeks collaborative interaction between a well-informed patient (instructed through a more extensive education program) and healthcare professionals.22
Another problem identified in connection with the CCM in COPD is poor population stratification. Focusing integrated care programs that include education, care coordination and telemonitoring on highly complex patients with frequent hospitalizations gives more consistent outcomes, with a reduction in exacerbations and hospital admissions, together with a notable improvement in HRQoL.23 There are barely any results in less complex populations. The use of telemedicine, despite its great potential, also gives heterogeneous results. A Cochrane systematic review24 showed a significant reduction in visits to the emergency department and in hospital admissions. However, it is not known whether this beneficial effect is attributable to the technology itself, or to the implementation of integrated programs. In a recent randomized trial, Pinnock et al.25 did not find any benefits in telemonitoring between groups following a similar care program.
Most of these studies focus on a single disease, in this case COPD. However, it is very interesting to assess interventions that manage patients with multiple chronic diseases. A randomized trial comparing the use of telemedicine with conventional treatment in 3230 patients with diabetes, heart failure or COPD showed lower mortality (4.6% vs 8.3%; odds ratio: 0.54; 95% CI: 0.39–0.75) and a lower rate of hospital admission (odds ratio: 0.82; 95% CI: 0.70–0.97; P=.017), with lower mortality at 12-month follow-up.26 These findings are very encouraging, although they must be replicated in different settings.
AsthmaAnother chronic respiratory disease with huge social, healthcare and economic impact is asthma, which is also often associated with comorbidities. According to Prosser et al.,27 60% of adult asthmatics have at least one concomitant disease, and 12% have 3 or more. Although chronic illness and aging go hand in hand in many cases, childhood asthma, which affects around 7% of the population, is an example of chronic disease in a young population that shares practically the same challenges as the older population.
Thirty-six percent of asthma patients have “uncontrolled” disease, and an additional 34.1% are “partially controlled”. Uncontrolled patients had poorer HRQoL and greater consumption of healthcare resources, tripling the mean cost per patient.28 According to the AsmaCost study, the annual cost of asthma in Spain is between €1480 and €3022 million.29 The mean cost per patient and year is estimated to be €1726, which varies according to the severity of the asthma, ranging from €959 for mild asthma to €2635 for severe asthma. The direct healthcare costs are mainly derived from hospital admissions and poor disease control.
Global strategies such as those proposed in the CCM can facilitate the objective of achieving and maintaining control in the asthmatic patient. Compared to COPD, fewer experiences have been amassed in asthma and CCM, and there is greater heterogeneity. Mehuys et al.,30 in a randomized trial in which education on medication use was offered and pharmacists were also involved in disease monitoring, found a greater reduction in the need for rescue medication, with fewer night-time awakenings, greater adherence to maintenance medication and better inhaler technique. Armor et al.,31 in a similar study, also found better asthma control. As in COPD, programs that include multiple elements of the CCM give better results, and in this context the benefits of educational programs have been widely reported.32 However, not all results are consistent, and some studies found no significant benefits.
Other Chronic Respiratory DiseasesApart from COPD and asthma, the principles of chronicity can potentially be applied to many other chronic respiratory diseases, such as sleep apnea–hypopnea syndrome, bronchiectasis, chronic diffuse interstitial diseases or chronic respiratory failure. However, cumulative scientific evidence remains limited. Recently, the American Association of Sleep Technologists33 proposed stratifying sleep studies according to patient complexity and applying principles of integrated treatment, including patient education, adherence monitoring and distance follow-up. Some authors are conducting integrated studies on sleep units and primary care to facilitate diagnosis and coordination of care,34 and much is being done to develop the use of telemedicine for a variety of interventions in this setting, ranging from diagnosis to adherence monitoring.35,36
For decades, the treatment of chronic respiratory failure (oxygen therapy and/or non-invasive ventilation), irrespective of the specific underlying disease, has been an example of home-based care that includes a clearly patient- and family-centered care reorganization. Integrated nursing care, health education, and more recently distance monitoring, have also been developed in the context of chronic respiratory failure. Attempts are also being made to decentralize other respiratory therapies such as rehabilitation, to switch the focus to home-based care with a closer, more personalized approach, where information and communication technology may also be of inestimable help.37 However, despite these examples, there is still no integrated approach that includes all the components of the CCM in the management of these diseases.
Role of Respiratory Medicine in Chronic IllnessAccording to the SNHS Strategy, chronic care requires encouraging the formation of interdisciplinary teams made up of different medical and social services professionals, to guarantee continuity of care with the full participation of the patient and their family.2 Naturally, primary care teams, which are central to the care strategy, have always played a major and relatively well-defined role. However, the role reserved for other specialties is less clear, suggesting that all SNHS professionals must become involved in improving the integrated approach to chronic illness. In this respect, the SNHS Strategy for COPD9 is already collaborating with the Chronicity Strategy in major tasks such as constructing a common electronic health history, and the need to update existing contents, with a shift toward chronic illness, is currently being debated.
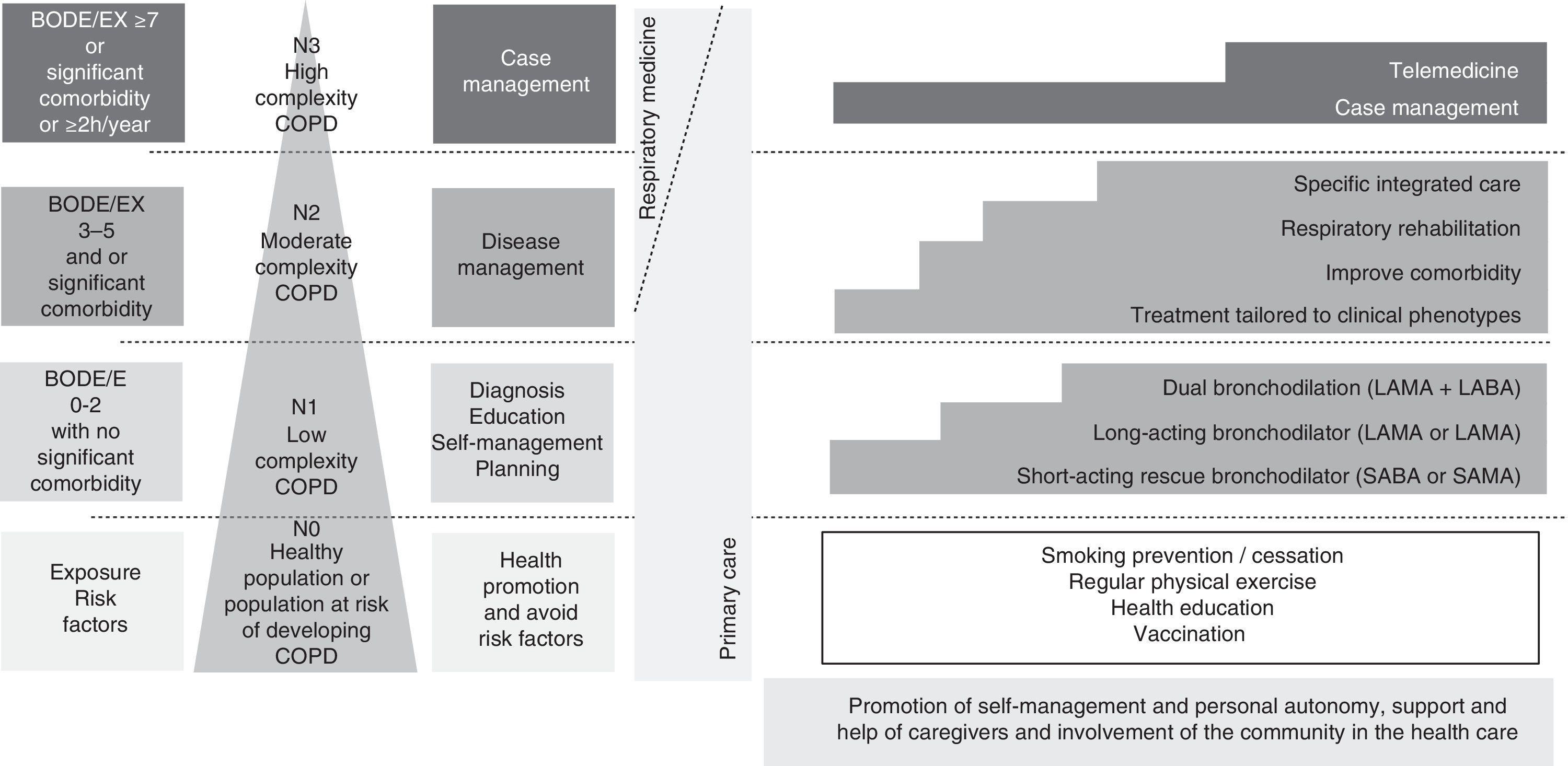
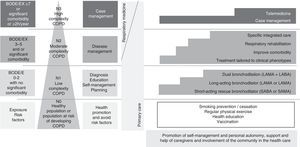
In our opinion, respiratory medicine must adapt itself to this new care context, contributing knowledge, experience, innovation and expertise. Integrated care requires collaboration and teamwork, and in this respect it is essential to overcome corporatist barriers and work closely with primary care, internal medicine and all disciplines that treat these patients. Respiratory medicine professionals undoubtedly have skills and abilities that make them natural leaders in respiratory diseases. This scientific and technical knowledge should be used to participate actively in the design of all related care programs, which should be based on the best scientific evidence available, and to apply efficiency criteria. In this respect, clinical practice guidelines for the main chronic respiratory diseases should be adapted to the chronic care management model, stratifying the actions according to the level of complexity. Fig. 3 shows a proposed adaptation to a chronic care model for the Spanish COPD society (GesEPOC).38 From an organizational point of view, respiratory medicine services must acquire a more cross-disciplinary approach that includes specific areas dedicated to chronic care, where the concepts of stratification, health promotion, self-care, health education, planned activity, disease management and case management can be implemented. As regards care, the main focus should be on severe, complex patients who require specialized integrated care, and also on many who require disease management. The use of new information and communication technology could be an advantage, provided it is used within specific integrated programs. Establishing integrated and computerized care processes aimed at standardizing care will be essential for the cross-management of these patients. In terms of prevention, the fight against smoking is paramount. Again, primary care must take center stage. Nevertheless, our extensive experience should enable us to train professionals in this and in the care of highly complex cases. The same might be said of health education and self-care, which should be promoted particularly at the primary care level, but which should inevitably extend to respiratory medicine teams. Throughout this entire preventive, educational and care context, respiratory medicine nursing is hugely important. Advanced nursing practice and case management must also be developed. Finally, we believe it is our obligation to evaluate and investigate, not only the different components of the CCM, but also the use of programs that integrate all actions. Many questions remain unanswered, and this is fertile ground for innovation and investigation. Spanish respiratory medicine has become a widely respected force in international research in recent decades. These qualities should be brought to bear in an area such as this, where accumulated evidence and experience is essential.
Adaptation of the chronic care model to Spanish COPD guidelines (GesEPOC).32 Four levels of complexity are proposed. L0: healthy population or population at risk of developing COPD. In addition to encouraging regular exercise and healthy lifestyle habits, it is essential to develop primary and secondary smoking prevention policies. L1: patients with low-complexity COPD will be identified by a BODE or BODEx index score of 0–2 points, with no significant comorbidities. It is essential to ensure a definitive diagnosis in these patients, and to encourage self-care. In addition to the measures listed in L0, these patients should be treated with bronchodilators (particularly long-acting), either as monotherapy or dual bronchodilation, according to the intensity of the symptoms. L2: Patients with moderately complex COPD will be identified by a BODE or BODEx index score of 3–6 points or by the presence of a significant comorbidity. Disease-management criteria should be used in this group. In addition to bronchodilator treatment, the patient's clinical phenotype should be characterized and treatment adjusted according to GesEPOC, to improve the comorbidity and assess respiratory rehabilitation. Assessment of specific integrated care is also recommended in this patient group. L3: high complexity patients. These patients will be identified by a BODE or BODEx index score ≥7, by various concomitant chronic diseases, or by 2 or more hospital admissions (h) in the previous year. Individualized case management should be proposed in this group, incorporating all the previous therapeutic measures and an integrated and multidisciplinary approach. Telemedicine may also be considered as a support tool in some cases.
The authors declare that they have no conflict of interests.
Please cite this article as: Soler-Cataluña JJ, Sánchez Toril F, Aguar Benito MC. El papel de la neumología ante la Estrategia de cronicidad del Sistema Nacional de Salud. Arch Bronconeumol. 2015;51:396–402.