To describe and compare from a gender perspective the social profile of patients admitted to a respiratory unit for COPD exacerbations (COPDE).
MethodologyA cross-sectional study in patients with serious COPDE in which demographic, clinical, and social data (economic situation, care, dependency for basic and instrumental activities, social risk, caregiver overload, use of social services) were collected using questionnaires and indices such as Barthel, Lawton-Brody, Zarit, Barber, and Gijón. A descriptive analysis was made of patients’ social and healthcare situation, compared on the basis of gender.
ResultsWe included 253 patients, aged 68.9±9.8years, 58 (23%) women, FEV1 42.1±14.2%, and Charlson index 1.8±0.9; 37.9% were active smokers. In total, 55.2% had an income of less than €800/month, 46.2% had some dependency for basic activities, and 89.3% for instrumental activities, 89% presented social fragility, while 64% were in a situation of social problem/risk; 49% had a caregiver, 83% in a non-formal arrangement, 90.9% of whom were women, with some overload reported by 69.2%. A total of 21.4% lived alone, and 22.9% had contacted social services. Women with COPDE are younger, smoke more actively, and have fewer comorbidities. They have more scant economic resources and assistance and are in a poorer socio-familiar situation, but they are less dependent for some activities.
ConclusionsThe social profile of patients with serious COPDE admitted to respiratory units is very unfavorable, especially among women. These inequalities appear to go beyond differences in the expression of COPD, and are associated with gender.
Describir y comparar desde una perspectiva de género el perfil social de los pacientes ingresados por agudizaciones de EPOC (AEPOC) en un servicio de neumología.
MetodologíaEstudio transversal en pacientes con AEPOC graves donde se recogieron variables demográficas, clínicas y de la esfera social (situación económica, cuidados, dependencia en las actividades básicas e instrumentales, riesgo social, sobrecarga de cuidador, uso de servicios sociales) utilizando cuestionarios e índices como Barthel, Lawton-Brody, Zarit, Barber y Gijón. Se realiza un análisis descriptivo de la situación sociosanitaria que se compara en función del género.
ResultadosSe incluyeron 253 pacientes, edad de 68,9±9,8años, 58 (23%) mujeres, FEV1 42,1±14,2% e índice de Charlson 1,8±0,9, 37,9% fumadores activos. El 55,2% cobran menos de 800€/mes, el 46,2% tienen alguna dependencia para actividades básicas y el 89,3% para actividades instrumentales, el 89% presentan fragilidad social y el 64% están en situación de problema/riesgo social. Disponen de cuidador el 49%: el 83% no formales y el 90,9% mujeres, con alguna sobrecarga en el 69,2%. El 21,4% viven solos. El 22,9% han contactado con los servicios sociales. Las mujeres con AEPOC son más jóvenes, fuman más activamente y tienen menos comorbilidades. Disponen de menos recursos económicos y ayuda y peor situación sociofamiliar, pero son menos dependientes para algunas actividades.
ConclusionesEl perfil social de los pacientes con AEPOC graves que ingresan en neumología es muy desfavorable, especialmente en las mujeres. Estas desigualdades parecen ir más allá de las diferencias de la expresión de la EPOC en función del género.
The World Health Organization (WHO) predicts that within a few years chronic obstructive pulmonary disease (COPD) will become the third leading cause of death worldwide.1 Its prevalence will increase in coming decades due to the persistently high numbers of smokers and population aging, both situations being particularly relevant in women.1 COPD exacerbations are common events in the natural history of the disease, and many patients require admission to hospital, generating a heavy burden on both patients and the system.2–4 A careful characterization of patients admitted for COPD exacerbation is essential when planning comprehensive care of the disease and the provision of more individualized and efficient management.2,5
The demographic and clinical characteristics of these patients have been determined, but there is less evidence on their social characteristics, a dimension that includes available resources, dependency, disability, risk of social exclusion, frailty, and autonomy.6–8 COPD causes progressive physical and mental limitations that hinder the performance of basic and instrumental activities of daily living and determine the need for assistance in these tasks, which can damage social relationships.8–11 The benefit that might be obtained by balancing this dimension could be as important for the patient as improvement in lung function.8,9 The available health and social welfare data are heterogeneous, and are derived mainly from elderly outpatients with a significant comorbidity burden admitted to internal medicine departments, and data obtained more than a decade ago.12,13 Information on social frailty could help predict events such as readmission and mortality that cannot currently be reliably anticipated on the basis of available demographic and clinical factors.13–16 In fact, some integrated care proposals recommend the systematic assessment of social frailty using specific questionnaires and scales.16,17
There has been growing interest in the impact of gender on COPD in recent years, particularly susceptibility, prevalence, diagnosis, comorbidities, and prognosis, but rarely social aspects.19,20 However, this type of assessment is considered a key element in health planning in the era of chronicity.21,22
Analyzing the social characteristics of patients with severe COPD exacerbations, in addition to their demographic and clinical characteristics, will provide much needed information for designing more personalized and efficient care programs.
MethodologyThis was a cross-sectional study describing the initial stages of follow-up of a cohort of patients (the SocioEPOC cohort) admitted for COPD exacerbations. Patients were recruited prospectively and consecutively in a third-level hospital which has a reference population of 375000 inhabitants in both urban and rural areas.
STROBE guidelines23 were followed for the study methodology and reporting of results.
Inclusion CriteriaAll patients with an index admission to the respiratory medicine department (first admission in the study period) and a primary diagnosis of COPD exacerbation during a 1-year period (2 January–31 December 2017) were considered for inclusion.
Exclusion CriteriaPatients were excluded if they refused to participate, if a diagnosis of COPD was ruled out during their follow-up, or if an alternative diagnosis to COPD exacerbation was made (pulmonary embolism, pneumonia, or other pathologies).
The recommendations of the GesEPOC guidelines2 were followed to diagnose or rule out COPD exacerbation.
After patient had been stabilized, 72–96h after admission, they were given the study information sheet and were asked to consent to participate in the study.
Data CollectionA review of the clinical history and a personal interview with the patient and their caregiver were used to record sociodemographic variables, history of smoking or active smoking habit, and in non-smokers, the possible etiology of COPD (significant biomass exposure, workplace exposure, or alpha-1 antitrypsin deficiency), chronic alcoholism (average daily intake >70g of alcohol in men or >50g in women), consumption of other drugs, influenza and pneumococcal vaccination, hospital admissions for COPD exacerbation and culture of pathogens in respiratory samples in the previous year, impact of COPD using the COPD Assessment Test (CAT) questionnaire,24 degree of dyspnea prior to this exacerbation according to the modified Medical Research Council (mMRC) scale,25 FEV1 in the last spirometry, eosinophils values in the clinical laboratory test on admission, the presence of anemia (hemoglobin <13g/dl in men and <12g/dl in women), comorbidities using the Charlson index,26 the Goldberg Scale of anxiety and depression,27 and the presence of sleep apnea syndrome or atrial fibrillation.
With regard to the social domain, an expert social worker recorded:
- •
Monthly income (< or >€800) and type of social security benefit (contributory or not), if received, and employee status.
- •
Type of dwelling (apartment, house, care home, hostel) and status as resident.
- •
Living situation (living or sleeping alone), if they had a caregiver, and if the caregiver was paid or not. If the caregiver was not paid, whether they were a family member (spouse, son/daughter, other).
- •
Previous use of municipal social work services or others.
- •
Patient's ability to perform basic activities of daily living (ADL) according to the Barthel index.28
- •
Patient's ability to carry out instrumental activities according to the Lawton-Brody index.29
- •
Social frailty and dependence according to the Barber questionnaire.30
- •
Social and family situation assessed using the Valoración Sociofamiliar de Gijón (Gijón Social-Family Scale).31
- •
Caregiver burden using the Zarit scale.32
See supplementary material (Appendix A Annex) for a brief description of the last 5 indices and scales mentioned and their interpretation.
Other variables, such as body mass index and BODEX, were calculated using the study data. All cardiovascular diseases included in the Charlson index were pooled and atrial fibrillation was added. FEV1 was used to classify patients according to GOLD guidelines.33 Data from indices and questionnaires (mMRC, CAT, Charlson, Goldberg) were used to create other dichotomous variables indicated in the results section. The same was done for social indices and scales, depending on the recommended cut-off point28–32 (see supplementary material [Appendix A Annex]).
The study was approved by the Research Ethics Committee of Galicia (file 2016/524).
Statistical AnalysisThe arithmetic mean and standard deviation were calculated for quantitative variables, and qualitative variables (number and percentage of cases) were used to construct contingency tables and were compared using the Chi-squared (χ2) or Fisher's exact test. Quantitative variables were compared using the Student's t-test.
The approach in all cases was 2-tailed and the significance level was 5%.
The analysis was carried out using the IBM SPSS Statistics 21 package (IBM Corporation, Armonk, New York),
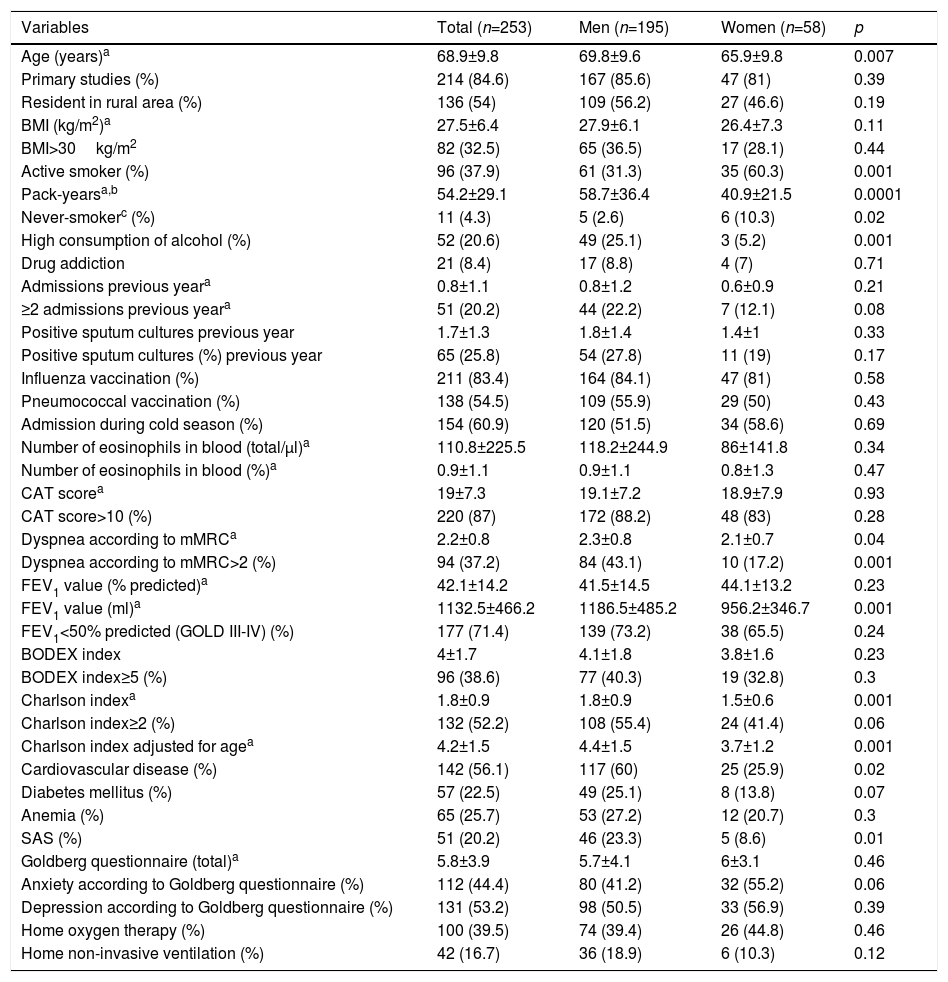
ResultsA total of 253 patients were included in the study, of which 58 (23%) were women. Five patients (2 women) were excluded: 2 because of the severity of their situation, and another 3 who refused to participate. Demographic and clinical characteristics, overall and by sex, are shown in Table 1.
Demographic and Clinical Characteristics of the Overall Cohort, and By Sex.
| Variables | Total (n=253) | Men (n=195) | Women (n=58) | p |
|---|---|---|---|---|
| Age (years)a | 68.9±9.8 | 69.8±9.6 | 65.9±9.8 | 0.007 |
| Primary studies (%) | 214 (84.6) | 167 (85.6) | 47 (81) | 0.39 |
| Resident in rural area (%) | 136 (54) | 109 (56.2) | 27 (46.6) | 0.19 |
| BMI (kg/m2)a | 27.5±6.4 | 27.9±6.1 | 26.4±7.3 | 0.11 |
| BMI>30kg/m2 | 82 (32.5) | 65 (36.5) | 17 (28.1) | 0.44 |
| Active smoker (%) | 96 (37.9) | 61 (31.3) | 35 (60.3) | 0.001 |
| Pack-yearsa,b | 54.2±29.1 | 58.7±36.4 | 40.9±21.5 | 0.0001 |
| Never-smokerc (%) | 11 (4.3) | 5 (2.6) | 6 (10.3) | 0.02 |
| High consumption of alcohol (%) | 52 (20.6) | 49 (25.1) | 3 (5.2) | 0.001 |
| Drug addiction | 21 (8.4) | 17 (8.8) | 4 (7) | 0.71 |
| Admissions previous yeara | 0.8±1.1 | 0.8±1.2 | 0.6±0.9 | 0.21 |
| ≥2 admissions previous yeara | 51 (20.2) | 44 (22.2) | 7 (12.1) | 0.08 |
| Positive sputum cultures previous year | 1.7±1.3 | 1.8±1.4 | 1.4±1 | 0.33 |
| Positive sputum cultures (%) previous year | 65 (25.8) | 54 (27.8) | 11 (19) | 0.17 |
| Influenza vaccination (%) | 211 (83.4) | 164 (84.1) | 47 (81) | 0.58 |
| Pneumococcal vaccination (%) | 138 (54.5) | 109 (55.9) | 29 (50) | 0.43 |
| Admission during cold season (%) | 154 (60.9) | 120 (51.5) | 34 (58.6) | 0.69 |
| Number of eosinophils in blood (total/μl)a | 110.8±225.5 | 118.2±244.9 | 86±141.8 | 0.34 |
| Number of eosinophils in blood (%)a | 0.9±1.1 | 0.9±1.1 | 0.8±1.3 | 0.47 |
| CAT scorea | 19±7.3 | 19.1±7.2 | 18.9±7.9 | 0.93 |
| CAT score>10 (%) | 220 (87) | 172 (88.2) | 48 (83) | 0.28 |
| Dyspnea according to mMRCa | 2.2±0.8 | 2.3±0.8 | 2.1±0.7 | 0.04 |
| Dyspnea according to mMRC>2 (%) | 94 (37.2) | 84 (43.1) | 10 (17.2) | 0.001 |
| FEV1 value (% predicted)a | 42.1±14.2 | 41.5±14.5 | 44.1±13.2 | 0.23 |
| FEV1 value (ml)a | 1132.5±466.2 | 1186.5±485.2 | 956.2±346.7 | 0.001 |
| FEV1<50% predicted (GOLD III-IV) (%) | 177 (71.4) | 139 (73.2) | 38 (65.5) | 0.24 |
| BODEX index | 4±1.7 | 4.1±1.8 | 3.8±1.6 | 0.23 |
| BODEX index≥5 (%) | 96 (38.6) | 77 (40.3) | 19 (32.8) | 0.3 |
| Charlson indexa | 1.8±0.9 | 1.8±0.9 | 1.5±0.6 | 0.001 |
| Charlson index≥2 (%) | 132 (52.2) | 108 (55.4) | 24 (41.4) | 0.06 |
| Charlson index adjusted for agea | 4.2±1.5 | 4.4±1.5 | 3.7±1.2 | 0.001 |
| Cardiovascular disease (%) | 142 (56.1) | 117 (60) | 25 (25.9) | 0.02 |
| Diabetes mellitus (%) | 57 (22.5) | 49 (25.1) | 8 (13.8) | 0.07 |
| Anemia (%) | 65 (25.7) | 53 (27.2) | 12 (20.7) | 0.3 |
| SAS (%) | 51 (20.2) | 46 (23.3) | 5 (8.6) | 0.01 |
| Goldberg questionnaire (total)a | 5.8±3.9 | 5.7±4.1 | 6±3.1 | 0.46 |
| Anxiety according to Goldberg questionnaire (%) | 112 (44.4) | 80 (41.2) | 32 (55.2) | 0.06 |
| Depression according to Goldberg questionnaire (%) | 131 (53.2) | 98 (50.5) | 33 (56.9) | 0.39 |
| Home oxygen therapy (%) | 100 (39.5) | 74 (39.4) | 26 (44.8) | 0.46 |
| Home non-invasive ventilation (%) | 42 (16.7) | 36 (18.9) | 6 (10.3) | 0.12 |
Patients had a mean age of almost 70 years, the majority had completed only primary education, and half lived in a rural environment. Four resided in hostels (1.6%) and 2 (0.8%) in care homes. Most were overweight or obese, and had functionally severe COPD and stable dyspnea (mMRC grade 2–3). In the vast majority of patients, COPD was mainly caused by smoking; nearly 40% continued to smoke actively, and 20% drank alcohol excessively. Less than 10% were drug users, most of whom were on methadone programs, and only 6 frequently consumed other toxic substances, such as heroin or cocaine. Although the Charlson index is low, slightly more than half of the cohort had cardiovascular comorbidities, half had anxiety or depression, and between 20% and 25% had diabetes, sleep apnea, or mild anemia. A total of 40% were receiving domiciliary oxygen and 15% noninvasive ventilation.
When compared on the basis of sex, women were younger, their COPD was more often due to causes other than smoking, they had a lower pack-year index, more were active smokers, and they drank less excessively. Despite a similar FEV1, they had a lower degree of dyspnea, cardiovascular comorbidities, and sleep apnea. They showed a greater degree of anxiety and less diabetes, but these differences did not reach statistical significance.
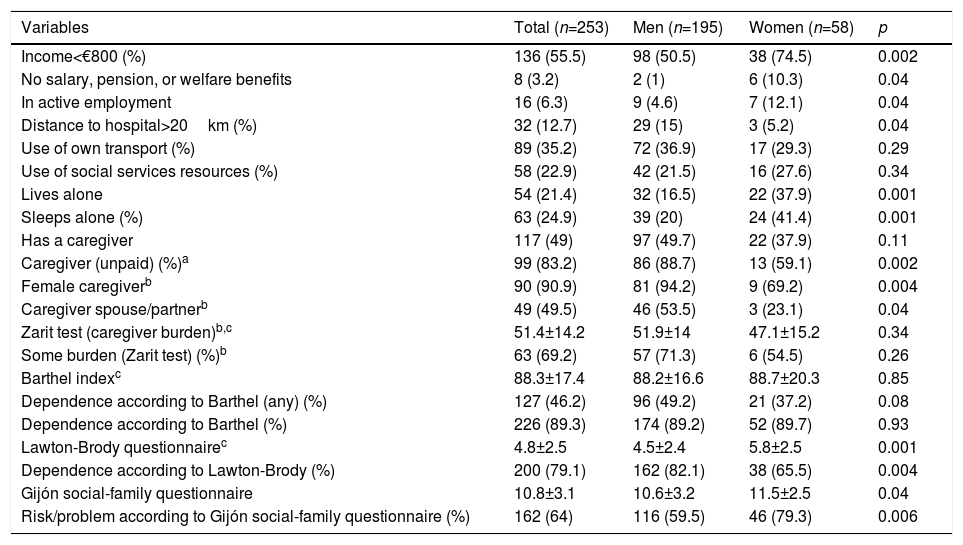
With respect to overall social characteristics (Table 2 and supplementary Tables 1–4), most patients were pensioners and more than half had a monthly income of less than €800, 25% lived or slept alone, almost half had some dependency for performing some basic ADLs (52.5% moderate and 18.6% severe), 90% for instrumental ADLs, and 60% had some social or family risk/problem. However, only half had a caregiver, of which 80% were informal, mostly women, and 60% of these caregivers reported some degree of burden. Half of the caregivers were the patients’ own spouses or partners and the other half were mainly daughters or relatives. However, barely 20% of patients had used the social services. Most patients resided less than 20km from the hospital, and one third had their own transportation.
Social Characteristics of the Total Cohort, and by Sex.
| Variables | Total (n=253) | Men (n=195) | Women (n=58) | p |
|---|---|---|---|---|
| Income<€800 (%) | 136 (55.5) | 98 (50.5) | 38 (74.5) | 0.002 |
| No salary, pension, or welfare benefits | 8 (3.2) | 2 (1) | 6 (10.3) | 0.04 |
| In active employment | 16 (6.3) | 9 (4.6) | 7 (12.1) | 0.04 |
| Distance to hospital>20km (%) | 32 (12.7) | 29 (15) | 3 (5.2) | 0.04 |
| Use of own transport (%) | 89 (35.2) | 72 (36.9) | 17 (29.3) | 0.29 |
| Use of social services resources (%) | 58 (22.9) | 42 (21.5) | 16 (27.6) | 0.34 |
| Lives alone | 54 (21.4) | 32 (16.5) | 22 (37.9) | 0.001 |
| Sleeps alone (%) | 63 (24.9) | 39 (20) | 24 (41.4) | 0.001 |
| Has a caregiver | 117 (49) | 97 (49.7) | 22 (37.9) | 0.11 |
| Caregiver (unpaid) (%)a | 99 (83.2) | 86 (88.7) | 13 (59.1) | 0.002 |
| Female caregiverb | 90 (90.9) | 81 (94.2) | 9 (69.2) | 0.004 |
| Caregiver spouse/partnerb | 49 (49.5) | 46 (53.5) | 3 (23.1) | 0.04 |
| Zarit test (caregiver burden)b,c | 51.4±14.2 | 51.9±14 | 47.1±15.2 | 0.34 |
| Some burden (Zarit test) (%)b | 63 (69.2) | 57 (71.3) | 6 (54.5) | 0.26 |
| Barthel indexc | 88.3±17.4 | 88.2±16.6 | 88.7±20.3 | 0.85 |
| Dependence according to Barthel (any) (%) | 127 (46.2) | 96 (49.2) | 21 (37.2) | 0.08 |
| Dependence according to Barthel (%) | 226 (89.3) | 174 (89.2) | 52 (89.7) | 0.93 |
| Lawton-Brody questionnairec | 4.8±2.5 | 4.5±2.4 | 5.8±2.5 | 0.001 |
| Dependence according to Lawton-Brody (%) | 200 (79.1) | 162 (82.1) | 38 (65.5) | 0.004 |
| Gijón social-family questionnaire | 10.8±3.1 | 10.6±3.2 | 11.5±2.5 | 0.04 |
| Risk/problem according to Gijón social-family questionnaire (%) | 162 (64) | 116 (59.5) | 46 (79.3) | 0.006 |
When comparing these characteristics on the basis of sex, women had a lower income, they were more often still in active employment, although a greater percentage did not receive any type of pension, salary or welfare benefits. They slept or lived alone more often and had fewer informal caregivers than men; caregivers were less frequently women, and fewer were their own partners/spouses. Women were less dependent for instrumental domestic tasks, controlling their medication, shopping and financial affairs, and for basic activities related to mobility. They presented a higher social problem/risk in the social and family domains of the Gijón questionnaire.
DiscussionThis study offers a comprehensive description and gender-based comparison of the social, demographic and clinical profiles of patients with severe COPD exacerbations admitted to the respiratory medicine department of a third-level hospital. This is the first study conducted in Spain that addresses the social situation from a gender perspective, using numerous social assessment indices and scales administered by expert personnel.
From a clinical point of view, the main clinical characteristics of the patients included in this study are very similar to those described in the AUDIPOC audits and the Spanish cohort of the pan-European COPD audit, consisting of 3493 and 4650 cases, respectively.34 We believe, therefore, that our study population is a good reflection of patients admitted to other respiratory departments in Spain.
In Spain, less than 20% of patients present COPD as their only chronic disease,35 as shown in this study. Although the average age was less than 70 years and the Charlson index less than 2, most patients presented multiple pathologies that met the criteria of comorbidity defined by the national strategy for care of chronicity of the Ministry of Health, Social Services and Equality.23,35 This document emphasizes the importance of coordinating between health and social services and addressing the problem from a gender perspective.18,23
Almost a quarter of our cohort are women. This percentage is higher than in other Spanish series,7,10,14,33 and may be explained by the period of time covered and by the fact that smoking among women began to rise in our health area earlier than in other regions, as previously described.36 From a demographic and clinical point of view, women in this study are slightly younger, with a lower pack-year index, and more frequently have a etiology other than smoking than men, as has already been described in other studies.19–21 Sixty percent are active smokers, similar to the data published by Mayoralas et al.11 in a large outpatient study of women with COPD. It is likely that other social or psychological determinants found in our study may come into play, in addition to a greater degree of addiction among women. This should compel us to raise awareness about COPD, as other authors suggest, and to implement more successful strategies in the prevention and treatment of COPD in women.12,19–21 In contrast to the findings of other studies,19–21 women with a similar lung function to men had a lower degree of dyspnea. This could be partly explained by the greater frequency of cardiovascular comorbidity among men (data not shown).
With respect to social profiles, our study shows the overall prevalence of disability and dependence for both basic and instrumental activities, loneliness, and social frailty and risk, some of which are noticeably worse in women. The low economic and educational level and major limitations in basic ADLs of COPD outpatients observed in the Spanish EIME study over 10 years ago10 has still prevails today.10 Only 7.5% of the patients included in the EIME study10 lived alone, a finding which contrasts with the 21.4% reported in our cohort. This figure is similar to that described in more recent studies in other countries37 and reflects societal changes in developed countries.23,34 Women have fewer economic resources and help, and more often work actively. They also have less dependence for basic instrumental activities related to household chores and shopping. This could be a result of the above, but may owe more to the roles and stereotypes of our society,22,38 a consideration that has led some authors to recommend evaluating questionnaires on the basis of sex.29
Only 16.3% of women with COPD in the Mayoralas study11 lived alone, compared to 40% of our series, a difference that might be explained by differences in the scope of the study, and that may possibly reflect a poorer social situation among patients with serious COPD exacerbations.35
With respect to non-formal care, women are cared for less frequently by their partners and spouses, so the caregiver burden tended to be lower, perhaps also because of the different social roles and inequalities already described.38
All these factors suggest that women with serious COPD exacerbations are found to be at greater risk of social exclusion when specific questionnaires addressing family and social domains are used – a risk that is generally higher than that described in an older, dependent population of COPD patients with multiple comorbidities.13
Our study has some limitations. Firstly, its single center design may not reflect the social and healthcare reality of other regions of Spain. However, the clinical characteristics of the patients included are similar to those described in extensive audits,34 although the mean age in our study was slightly lower. In addition, our sample size could be too small to adequately compare some variables. Finally, the social aspects (dependence, social frailty and risk of exclusion, caregiver burden) were assessed using scales and questionnaires that have not been widely validated in patients with COPD. The same could be said for the assessment of anxiety and depression. However, as these tools are recommended for use in integrated healthcare processes in COPD and patients with multiple pathologies,17,18 they were used to facilitate future comparisons with other studies and evaluate their usefulness. Finally, we did not evaluate specific factors, such as quality of life, which might be of interest.
The most important advantages of this study include the novel use of social scales administered by expert personnel, consecutive case sampling, which reduces the possibility of selection bias, and the fact that we focus on patients with COPD exacerbations, adding to the relative homogeneity of the study population.
In conclusion, patients with severe COPD exacerbations admitted to respiratory departments are highly dependent, at risk of social exclusion, need the help of caregivers who are often overburdened, and a significant number of them live alone. There are notable gender differences, and women have more limited economic resources and assistance and a worse family and social situation, although they are less dependent for some activities. These inequalities, which seem to go beyond gender differences in COPD manifestation, should be taken into account in the design of comprehensive COPD care programs. The potential weight of social factors in COPD exacerbations opens the door for future studies to determine the involvement of these factors in other events, such as readmissions or mortality, compared to purely clinical variables.
FundingThis study was funded by grants obtained from SEPAR (grant 456/2017), FIS-ISCII PI18/01317 (FEDER) and the unconditional collaboration of the company Menarini.
Conflict of InterestsThe authors state that they have no conflict of interests.
Please cite this article as: Fernández-García S, Represas-Represas C, Ruano-Raviña A, Mosteiro-Añón M, Mouronte-Roibas C, Fernández-Villar A. Perfil social de los pacientes que ingresan por una agudización de EPOC. Un análisis desde una perspectiva de género. Arch Bronconeumol. 2020;56:84–89.