Patients with cerebral infarction often present impaired consciousness and unsatisfactory extubation. We aimed to assess the respiratory mechanics components that might be associated with the success of extubation in stroke patients.
MethodsTwenty consecutive patients with stroke who needed mechanical ventilation support were enrolled. The maximal inspiratory pressure, gastric and the esophageal pressure (Pdi/Pdimax), minute volume, respiratory rate, static compliance, airway resistance, rapid shallow breathing index (RSBI), inspiratory time/total respiratory cycle (Ti/Ttot), and PaO2/FiO2 were measured.
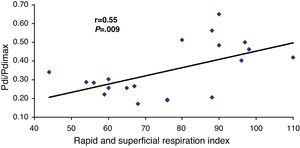
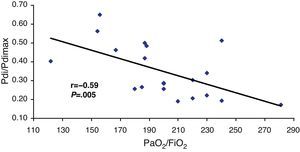
ResultsThe group who presented success to the extubation process presented 12.5±2.2=days in mechanical ventilation and the group who failed presented 13.1±2=days. The mean Ti/Ttot and Pdi/Pdimax for the failure group were 0.4±0.08 (0.36–0.44) and 0.5±0.7 (0.43–0.56), respectively. The Ti/Ttot ratio was 0.37±0.05 (0.34–0.41; P=.0008) and the Pdi/Pdimax was 0.25±0.05 for the success group (0.21–0.28; P<.0001). A correlation was found between Pdi/Pdimax ratio and the RSBI (r=0.55; P=.009) and PaO2/FiO2 (r=−0.59; P=.005). Patients who presented a high RSBI (OR, 3.66; P=.004) and Pdi (OR, 7.3; P=.002), and low PaO2/FIO2 (OR, 4.09; P=.007), Pdi/Pdimax (OR, 4.12; P=.002) and Raw (OR, 3.0; P=.02) developed mechanical ventilation extubation failure.
ConclusionMuscular fatigue index is an important predicting variable to the extubation process in prolonged mechanical ventilation of stroke patients.
Los pacientes con infarto cerebral presentan a menudo un deterioro del nivel de conciencia que hace que la extubación no sea satisfactoria. El objetivo de este estudio fue evaluar los componentes de la mecánica respiratoria que pudieran estar relacionados con el éxito de la extubación en pacientes con ictus.
MétodosSe incluyó en el estudio a 20 pacientes consecutivos con ictus que necesitaron apoyo de ventilación mecánica. Se efectuaron determinaciones de la presión inspiratoria máxima, la presión gástrica y esofágica (Pdi/Pdimáx), el volumen-minuto, la frecuencia respiratoria, la elasticidad estática, la resistencia de las vías aéreas (RAW), el índice de respiración rápida y superficial (RSRI), la relación tiempo inspiratorio/tiempo de ciclo respiratorio total (Ti/Ttot) y la PaO2/FiO2.
ResultadosEl grupo de pacientes que pudieron ser extubados con éxito tenía un tiempo de permanencia en ventilación mecánica de 12,5±2,2días, en comparación con 13,1±2días en el grupo en el que fracasó el proceso de extubación. La media Ti/Ttot y de Pdi/Pdimáx en el grupo de fracaso de la extubación fue de 0,4±0,08 (0,36 a 0,44) y de 0,5±0,7 (0,43 a 0,56), respectivamente. La relación Ti/Ttot fue de 0,37±0,05 (0,34 a 0,41; p=0,0008) y la relación Pdi/Pdimáx fue de 0,25±0,05 en el grupo de extubación satisfactoria (0,21 a 0,28; p<0,0001). Se observó una correlación entre la relación Pdi/Pdimáx y el RSRI (r=0,55; p=0,009) y la PaO2/FiO2 (r=−0,59; p=0,005). Los pacientes que tenían valores altos de RSRI (OR, 3,66; p=0,004) y Pdi (OR, 7,3; p=0,002) o valores bajos de PaO2/FiO2 (OR, 4,09; p=0,007), Pdi/Pdimáx (OR, 4,12; p=0,002) y RAW (OR, 3,0; p=0,02) presentaron un fracaso de la extubación de la ventilación mecánica.
ConclusiónEl índice de fatiga muscular es una variable predictiva importante del proceso de extubación en pacientes con ictus en los que se ha utilizado una ventilación mecánica prolongada.
Both the delayed withdrawal and the premature interruption of mechanical ventilation have been associated with increased mortality in intensive care units (ICUs).1,2 The decision of whether a patient can tolerate extubation is important as there is failed extubation in 10%–20% of patients, and this is associated with poorer clinical results.3,4 During this process, it is not uncommon to find errors in the prediction of extubation when using regular evaluation methods to measure the ability of the patient to breathe without help, such as blood gas analysis, vital capacity (VC) determination, and minute ventilation (VE). However, airway resistance (Raw) and elasticity (static) of the respiratory system are simple, non-invasive methods that are widely used to predict the success of extubation in patients with respiratory disease.5–7
Patients with cerebral infarction, especially those who present with cerebral edema and an extensive affectation of the encephalic trunk, often present a deteriorated level of consciousness. These patients generally have a poor prognosis due to the affectation of vital centers or respiratory complications.8–10 In ICUs, the question frequently comes up of how to extubate stroke patients with satisfactory parameters when there are concerns about the patient's level of consciousness and capacity to maintain spontaneous breathing. It is well known that there is a high incidence of pneumonia in patients with cranial trauma in whom prolonged intubation becomes necessary.11
The rapid shallow breathing index (RSBI), which is reflected in the relationship of respiratory frequency and tidal volume (f/Vt), is a simple datum to obtain for predicting the result of the extubation more precisely than isolated parameters.12 Chatila et al.13 observed that the f/Vt ratio was more exact than other clinical tools that are frequently used to predict the result of mechanical ventilation extubation. The predictive exactness and the simplicity of the f/Vt parameter justify their use in the management of patients with mechanical ventilation. The maximal transdiaphragmatic pressure ratio (Pdi/Pdimax) could be another important parameter for predicting the success of extubation.14–16 However, little is known about the integrated evaluations of respiratory mechanics, maximal transdiaphragmatic pressure and the PaO2/FiO2 ratio.
Although there are few studies that establish indices for predicting the success of extubation in stroke patients and there are no available guidelines, according to our experience in this disorder, the evolution seems to be good without an artificial airway. Our hypothesis was that Pdi and Pdi/Pdimax are important indirect indicators for predicting the satisfactory extubation of the mechanical respirator in stroke patients. The objective of this study is to identify components of respiratory mechanics that are associated with the success of extubation in stroke patients in whom mechanical ventilation is used.
Materials and MethodsWe carried out an observational, prospective cohort study in 20 consecutive patients with stroke who were hospitalized with mechanical ventilation for more than 10 days in our ICU. The protocol included the periods between July and October 2008. The study was approved by the internal review committee at our university, and the family members of all the patients gave their written informed consent.
InclusionInclusion criteria included stroke (brain stem infarction) that had been confirmed (by imaging techniques) and the patient had been intubated (≥10 days), while hemodynamically stable (without alteration of the circulation values, arterial pressure or ECG) and with a Glasgow coma score (GCS)≥7. Infection was controlled with leukocyte count (12000mm3), temperature (37°C), arterial pressure, and chest radiography without bronchograms. We chose 4 subjective criteria in order to evaluate the level of consciousness of the patients, in the following manner: (a) blinking; (b) holding the researcher's hand; (c) raising at least one of the lower limbs; and (d) confirmation of his/her name.
ExclusionExcluded from the study were those patients who presented arrhythmia, high blood pressure (MAP>150mmHg) or low blood pressure (PAM<60mmHg), recurring stroke of any type or any other disease other than the stroke.
ProtocolWe determined body mass index (BMI) and fluid balance in order to measure the patient's state of hydration. The patients included in our ICU received mechanical ventilation with an endotracheal tube. Before extubation, a gastroesophageal balloon was placed as described in another publication.12 It was established that these patients should be extubated 10 days after the start of mechanical ventilation if they met all the inclusion criteria for the study. Afterwards, other devices (non-invasive ventilation, oxygen therapy) and drugs (diuretics, racemic adrenaline) were used as necessary in order to maintain the patient's spontaneous breathing. If this failed, the patient was intubated.
Patients were sedated with midazolam (Dormonid®) and the gastroesophageal balloon allowed us to determine the gastric and esophageal pressures, representing the abdominal and pleural pressures, respectively. The total of the gastric and esophageal pressures provided us the manner to measure transdiaphragmatic pressure (Pdi=maximal difference between abdominal and pleural pressures).17 Anteroposterior chest X-ray was used to confirm that the gastroesophageal balloon was placed exactly. Once the balloon was placed, we interrupted sedation with the use of flumazenil (Lanexate®). Immediately after the patient had recovered consciousness, we performed the 4 subjective tests in order to verify that the patients were not sedated (blinking, holding the researcher's hand, lifting at least one lower limb, and confirmation of his/her name). If the patient confirmed being awake, we measured the highest value of maximal inspiratory pressure (PImax) using a compound gauge directly connected to the endotracheal tube. To confirm the absence of leaks, a nasal clip was used and the pressure was verified inside the balloon (tube sleeve). The best of three maneuvers with a rest period of 30s was taken as peak effort (PImax).
We also determined the fatigue index of the respiratory muscles, which is defined as Ti/Ttot/Pdi/Pdimax, where Ti is inspiratory time, Ttot is total respiration time, Pdi is the mean diaphragmatic pressure generated by breathing and Pdimax is the maximal transdiaphragmatic pressure. The value of Ti/Ttot/Pdi/Pdimax reflects the function of the intercostal muscles and diaphragm. When breathing is done with an inspiratory load, the threshold of the muscle fatigue index is from 0.35 to 0.40.17,18
Before the use of flumazenil (Lanexate®), we determined the maximal and plateau pressure values of the airway pressure, inspiratory flow, tidal volume (Vt), minute volume, RR and positive end-expiratory pressure (PEEP) while the patient continued to be connected to the mechanical respirator. The parameters for assessment were evaluated breath by breath for 1min. The respirator used was a Rafael® (Hamilton Medical). The parameters registered were the following: static elasticity (ml/cmH2O), airway resistance (cmH2O/l/min), dead space/tidal volume ratio (Vd/Vt), RSBI, Ti/Ttot and PaO2/FiO2 ratio. Total static lung elasticity was determined using: tidal volume/inspiratory plateau pressure−PEEP. Raw was determined by means of: maximal inspiratory pressure−plateau pressure/inspiratory flow. The PaO2/FiO2 ratio was determined by blood gas analysis with a normal concentration of O2 in order to maintain SpO2 above 90%. For the statistical analyses, we took the highest values from all the determinations. When the patient presented a clinical state of spontaneous breathing, the RSBI was determined while the patient was connected to the respirator in spontaneous-function mode. Meanwhile, spontaneous RR was determined by dividing the spontaneous tidal volume by liters. The index was obtained after the first and fifth minutes. The mechanical respiration parameters and oxygen parameters were compared with the normal values.18,19
The patient was extubated if he/she presented a clinical state of spontaneous breathing with PaO2/FiO2>200 and an SpO2>92%. During the extubation procedure and for the following hour, every measure was taken to ensure the safety of the patient (for example, non-invasive ventilation and oxygen, aspiration, use of diuretics and racemic adrenaline). The extubation process was considered to have failed if the patient presented a decrease in the level of consciousness, respiratory discomfort and/or hypoxemia despite the use of non-invasive ventilation and oxygen therapy for a period of up to 30min.
In the event of failed extubation, the patient was intubated again and tracheostomy was later proposed. Patients who were able to remain extubated were included in the protocol. Before extubation, 5min after and 1h after, maximal transdiaphragmatic pressure was determined in patients in whom the protocol was successfully applied. Pdi was determined during calm breathing and also during a maneuver of maximal inspiration performed by the patient. For both determinations, the external part of the gastroesophageal balloon was connected to a pneumotachograph. The determination of the correct position and the exact measurements of the gastroesophageal balloon were done with an occlusion test and the values reached were within reference values. In all patients, a nasal clip was used during both maneuvers. We did not determine Pdi in patients who were re-intubated within 1h after the initial extubation.
Statistical AnalysisThe continuous variables are presented as means, standard deviation, ratios, and percentages. The simple comparisons of the groups were done with the t-test for unpaired data or with the χ2 test. The factors associated with failed extubation were studied with a logistic regression model and the strength of the association is expressed with odds ratios and 95% confidence intervals. The variables evaluated were the following: Ti/Ttot, Pdi/Pdimax ratio, PaO2/FiO2 ratio, PImax, RSBI and respiratory mechanics. The level of statistical significance for each test was established at P<.05. The sample size was calculated depending on the variability of the maximal transdiaphragmatic pressure with the use of the E/S equation, corresponding with the magnitude of the expected effect divided by standard deviation of the result assessment variable. We used an α error of 5% and a β error of 20%, based on the results of previous studies.12 18 patients were necessary in order to meet the statistical power demands established for this research. The statistical analysis was done with a commercial statistical computer program (InStat3®).
ResultsThe 20 patients included in this study had a mean age of 56.4±4.7 (48–67); mean BMI was 20.1±3.4(14.3–27.1)kg/m2, PImax was 43.8±9.1(30–64)cmH2O, transdiaphragmatic pressure (Pdi) was 15.1±5.5 (9–26), maximal transdiaphragmatic pressure (Pdimax) was 45±10(30–64)cmH2O, the transdiaphragmatic pressure/maximal transdiaphragmatic pressure ratio (Pdi/Pdimax) was 0.34±0.1 (0.17–0.65), PaO2/FiO2 was 199.8±35 (122–281) and RSBI – Tobin was 107±12 (104–111). The effective inspiratory time (Ti/Ttot) was 0.38±0.1, the mechanical ventilation time was 302±35, lung elasticity was 43.4±8.8 and Raw was 7.9±2.4 (Table 1).
Clinical Evaluation of the Patients Upon Hospitalization and 10 Days After Remaining in the ICU.
| Variables | At Admittance | After 10 Days | P Value |
| Age, years | 56.4±4.9 | 56.4±4.9 | – |
| Sex, M/F | 12/8 | 12/8 | – |
| BMI, kg/m2 | 20.1±3.5 | 19.6±3.4 | .6 |
| Glasgow scale | 10±1 | 10±2 | .4 |
| Systolic blood pressure, mmHg | 145±15.7 | 145±13.6 | .9 |
| Diastolic blood pressure, mmHg | 93±11.2 | 91±8.8 | .5 |
| Heart rate, beats/min | 91.3±23.6 | 89.1±28.6 | .8 |
| Temperature, °C | 37.7±0.8 | 37.5±0.7 | .3 |
| Inspiratory pressure, cmH2O | 43.8±9.3 | 38.3±6.7 | .03 |
| Transdiaphragmatic pressure, cmH2O | 15.1±5.6 | 17.2±6 | .2 |
| Maximal transdiaphragmatic pressure, cmH2O | 45±10.3 | 41.2±8.3 | .2 |
| Pdi/Pdimax, cmH2O | 0.3±0.1 | 0.43±0.2 | .09 |
| Ti/Ttot | 0.38±0.1 | 0.39±0.1 | .9 |
| PaO2/FiO2 | 199.8±36.1 | 204.7±40.1 | .7 |
| Rapid shallow breathing index (RSBI) (l) | 107±12 | 85±13 | .4 |
| Lung elasticity, ml/cmH2O | 40.7±4.7 | 43.4±8.8 | .2 |
| Airway resistance, l/s/cmH2O | 7.9±2.4 | 8.2±2.6 | .7 |
| Mechanical ventilation time, h | 307±34.5 | 302.8±35.4 | .7 |
BMI: body mass index; Pdi/Pdimax: transdiaphragmatic pressure/maximal transdiaphragmatic pressure ratio; Ti/Ttot: inspiratory time/total respiratory cycle time ratio; PaO2/FiO2: arterial oxygen pressure/inspiratory fraction of oxygen ratio.
In the group in which the extubation process was satisfactory, the mean number of days of mechanical ventilation was 12.5±2.2 versus 13.1±2 in the group with failed extubation. In 12 patients (60%), tracheostomy was not used (extubation success). The characteristics of the 2 groups of patients are presented in Table 2.
Clinical Characteristics of the Satisfactory Extubation Group and the Failed Extubation Group.
| Variables | Success (n=12) | Failure (n=8) | P Value |
| Age, years | 56±5 | 58±5 | .32 |
| Sex, M/F | 8/4 | 5/3 | – |
| BMI, kg/m2 | 22±2.8 | 18±3.1 | .01 |
| Glasgow scale | 10±2 | 9±1 | .2 |
| Systolic blood pressure, mmHg | 147.5±13 | 141.3±15.9 | .4 |
| Diastolic blood pressure, mmHg | 90.8±8 | 96.3±12.4 | .3 |
| Heart rate, beats/min | 89.2±24.6 | 94.5±16.9 | .6 |
| Temperature, °C | 37.6±0.7 | 38±0.7 | .2 |
| Maximal inspiratory pressure (PImax), cmH2O | 45.3±10.3 | 41.6±7.5 | .39 |
| Transdiaphragmatic pressure, cmH2O | 12.1±1.4 | 20.8±3.8 | <.0001 |
| Maximal transdiaphragmatic pressure, cmH2O | 46.8±10.8 | 42.5±9.4 | .37 |
| Pdi/Pdimax, cmH2O | 0.2±0.05 | 0.5±0.07 | <.0001 |
| Ti/Ttot | 0.4±0.05 | 0.4±0.04 | .1 |
| PaO2/FiO2 | 216±27 | 175±34 | .008 |
| Rapid shallow breathing index, l | 96±12 | 149±28 | <.0001 |
| Lung elasticity, ml/cmH2O | 42±5 | 39±2 | .34 |
| Airway resistance, l/s/cmH2O | 6.6±1.0 | 10±2.4 | .0004 |
| Mechanical ventilation time, h | 301±34 | 317±35 | .31 |
BMI: body mass index; Pdi/Pdimax: transdiaphragmatic pressure/maximal transdiaphragmatic pressure ratio; Ti/Ttot: inspiratory time/total respiratory cycle time ratio; PaO2/FiO2: arterial oxygen pressure/inspiratory fraction of oxygen ratio.
We considered the extubation to be successful if the patient remained extubated 48h later. The first 4h following the extubation were the worst for these patients, given that half of the group that failed in the process needed invasive mechanical ventilation support within this time period. The other patients were re-intubated over the course of the first 24h (P=.0001).
The muscle fatigue index was determined with the Ti/Ttot and Pdi/Pdimax ratios. It was considered within the area of respiratory muscle fatigue if any of these values were higher than 0.4. The mean Ti/Ttot and Pdi/Pdimax for the extubation failure group were 0.4±0.08 (95% CI, 0.36–0.44) and 0.5±0.7 (95% CI, 0.43–0.56), respectively. In the extubation failure group, there were only 2 patients with a Pdi/Pdimax ratio lower than 0.4, and 2 presented a Ti/Ttot ratio equal to 0.4. Thus, 6 patients were in the fatigue zone and 2 in the risk zone for developing respiratory muscle fatigue. The Raw was significantly higher in this group (P=.0004). Static lung elasticity did not present significant differences between the two groups (P=.34) (Table 2).
None of the patients in the satisfactory extubation group were within the respiratory muscle fatigue zone: 6 were in the zone at risk of developing fatigue and 3 were in the lack of fatigue zone. The Ti/Ttot ratio was 0.37±0.05 (95% CI, 0.34–0.41) and the Pdi/Pdimax ratio was 0.25±0.05 (95% CI, 0.21–0.28). The groups with failed extubation presented values of the Ti/Ttot ratio and the Pdi/Pdimax ratio higher than those of the satisfactory extubation group (P<.0001 and P=.0008, respectively) (Table 2).
We observed a significant correlation between the Pdi/Pdimax ratio and the RSBI (r=0.55; P=.009) and the PaO2/FiO2 (r=−0.59; P=.005) (Figs. 1 and 2, respectively).
All the significant variables are included in a logistic regression model with the aim to determine the factors that predisposed patients for reintubation. The patients in whom there was an RSBI<80, a PaO2/FiO2 ratio<200, a Pdi/Pdimax ratio<40cmH2O, a Pdi>15 and a Raw<8 presented mechanical ventilation extubation failure (Table 3).
Predisposing Variables that Lead to Failure of the Extubation Process in ICU Patients.
| Variables | OR | CI | P |
| RSBI>80, l | 3.66 | 1.39–9.62 | .0045 |
| Pdi/Pdimax>0.4, cmH2O | 4.12 | 1.20–14.17 | .0022 |
| IMC>17, kg/m2 | 1.53 | 0.72–3.27 | .42 |
| Ti/Ttot>40 | 1.66 | 0.88–3.14 | .37 |
| Raw>8, l/s/cmH2O | 3.0 | 1.13–7.90 | .022 |
| Pdi≤15, cmH2O | 7.3 | 1.16–46.25 | .0021 |
| PaO2/FiO2>199 | 4.091 | 1.18–14.09 | .0078 |
RSBI: rapid shallow breathing index; Pdi/Pdimax: transdiaphragmatic pressure/maximal transdiaphragmatic pressure ratio; BMI: body mass index; Ti/Ttot: inspiratory time/total respiratory cycle time ratio; Raw: airway resistance; Pdi: transdiaphragmatic pressure; PaO2/FiO2: arterial oxygen pressure/inspiratory fraction of oxygen ratio.
Our study has obtained two main results:
- •
The values of the muscle fatigue index (Ti/Ttot/Pdi/Pdimax and the Pdi/Pdimax ratio) higher than 40% play a decisive role as predictive factors of a failed extubation process in stroke patients.
- •
The first 4h after extubation is decisive in terms of the success or failure of the extubation process.
Some data of respiratory mechanics and oxygenation are frequently evaluated in the extubation process of patients in whom prolonged mechanical ventilation has been used.2,13 Factors such as age, sex (mainly women), heart dysfunction, and low cardiac output could also require mechanical ventilation in excess.14,15 Despite there being few studies20,21 about the evaluation of this extubation process with the use of data on respiratory mechanics, none of them have been centered on the evaluation of respiratory muscle strength as a predictive factor for the success of extubation in these patients in order to withdraw mechanical ventilation. However, in our study we have observed the importance of measuring respiratory mechanics as well as the strength of the respiratory muscles (Table 3). It could be supposed that our patients did not have enough muscle strength because their BMIs were at the lower limit of normal (Table 1).7 Nevertheless, this situation is predictable in ICU patients who have been kept on mechanical ventilation for long periods of time.16
Several studies have recommended the use of static lung elasticity as a reliable variable for the prediction of successful extubation in patients with lung disease (e.g. COPD, pneumonia, ARDS).2,16 Furthermore, these data are easy to obtain with non-invasive methods. Nonetheless, as other studies have indicated, we observed that static lung elasticity presents lower-than-normal values,22 and this datum was not sensitive enough to differentiate the prognosis in the extubation process (P=.77). One probable explanation of this observation would be related with the time spent by patients in the ICU and the effect of the positive pressure during mechanical ventilation.
We have also observed that Raw was greater in the failed extubation group than in the satisfactory extubation group (P=.003). The high Raw in this group of patients could be related with edema, the presence of liquids or secretions in the airway walls that reduce functional residual capacity, and bronchial spasms.23 Oddo et al.24 demonstrated that high Raw is one of the most important factors that predict the need for mechanical ventilation, as well as the difficulty of satisfactory extubation, and that these alterations increase the effort required for respiration and could lead to respiratory muscle fatigue and a high risk of mortality. Failed extubation is frequently the result of a lack of protection of the airway and, therefore, it depends on the combination of cough, secretions and mental state.
We have demonstrated that the increased muscle fatigue index Ti/Ttot/Pdi/Pdimax (3.1 [2.13–5.5]) and the Pdi/Pdimax ratio were the main driving factors for extubation failure (OR, 4.7 [2.5–5.8]). This would occur mainly in the presence of a high Raw. Not even with the use of non-invasive ventilation was muscle fatigue avoided in the 8 patients in whom mechanical ventilation was re-instated.
PImax continues to be widely used for the prediction of extubation failure and the early detection of muscle fatigue, especially when this value is less than 20cmH2O. However, Meade et al.25 revealed that PImax is extremely inexact and should not be used for predicting the results of respirator disconnection or extubation. Nonetheless, our results indicate that the muscle fatigue index and the Pdi/Pdimax ratio, as an isolated measurement of diaphragm effectiveness, have a predictive value higher than that of PImax, especially in patients with values higher than 20cmH2O.
It has been reported that respiratory skeletal muscle fatigue occurs when the muscles generate more than 15% of their maximal effort during a sustained contraction. It is well-known that fatigue is produced only when the pressure–time level generated surpasses that threshold level. In addition, the fatigue threshold is higher during the intermittent contractions and depends on the relative duration of the contraction and relaxation, especially if the inspiratory muscles of the individuals examined are subjected to an external inspiratory load. For this reason, we measured the respiratory muscle fatigue index, which is defined as Ti/Ttot/Pdi/Pdimax, where Ti is the inspiratory time, Ttot is the total respiration time, Pdi is the mean transdiaphragmatic pressure generated by breathing and Pdimax is the maximal transdiaphragmatic pressure. The value of Ti/Ttot/Pdi/Pdimax reflects the function of generating contractions by the intercostal muscles and diaphragm. When breathing is produced with an inspiratory load, the threshold of the muscle fatigue index is from 0.35 to 0.40. Under this threshold, breathing can be maintained for more than 1h without evidence of fatigue. Above this threshold, there is a failure in the task after a time limit that is inversely related with muscle fatigue index.17,18
Our data demonstrated that in 60% of our patients from the failed extubation group, mechanical ventilation was reinstated in the first 4h after extubation. Yang et al.12 demonstrated that the first 4h following extubation are crucial for determining either the success or failure of said process. This is related with the difficult adaptation of the patient to spontaneous breathing, the variability of the levels of consciousness and the high resistance of the airways. Several authors12,17,21 have indicated that the work of respiration is the sum of the resistive and elastic work, and that the higher values during a long period of time leads to fatigue of the respiratory musculature. The authors also suggest that the muscle fatigue index (Ti/Ttot/Pdi/Pdimax) test the energy output of the respiratory muscles during mechanical work, constituting a predictive muscle fatigue variable.25 As we have shown, the high values of Pdi and the Pdi/Pdimax ratio were the reason why some patients presented failed extubation during the first 4h before spontaneous breathing (Table 2).
Our study has certain limitations. We did not determine the intracranial pressure, although we constantly verified the maximal respiratory pressures of our patients in order to avoid all undesirable vascular hypertension.26 Another limitation is that we did not have a control group available, based on the supposition that our patients were their own controls.
ConclusionThe muscle fatigue index is an important parameter for predicting the success of the extubation process in patients with stroke who have used prolonged mechanical ventilation. The success of extubation in stroke patients is related with a careful evaluation of respiratory musculature indices, such as the Pdi and Pdi/Pdimax.
Ethical ResponsibilitiesThe protocol was presented to the ethics committee of our university and approved by said committee, and all patients gave their written informed consent.
FundingNo fund was received, for this study, from any tobacco company or from other companies.
AuthorshipThis material has not previously been published, either completely or partially, nor is it being considered for publication elsewhere. Any unexpected adverse effects or change in protocol have been declared. All the authors have made important contributions to the study and have read and approved of the manuscript. All the authors agree with the declarations indicated and cede the editorial rights to this article.
Conflict of InterestsThe authors declare having no conflict of interest.
Please cite this article as: Castro AAM, et al. Evaluación de la musculatura respiratoria en la predicción del resultado de la extubación de pacientes con ictus. Arch Bronconeumol. 2012;48:274–9.
This study was carried out at the Universidad Adventista de São Paulo and the Hospital Itamaraty.