We would like to present the case of a 52-year-old woman, with a personal history of grade I obesity, occasional smoker of 2–3 cigarettes, who was diagnosed with deep vein thrombosis (DVT) of the right lower limb 6 months before hospitalization. She presented neither respiratory history of interest nor any known allergies to medication, nor diabetes mellitus nor arterial hypertension. She had neither toxic habits nor any type of occupational exposure. She worked as a homemaker and had no family history of interest either. She was taking a standard treatment with warfarin due to the recent DVT episode. The patient came to the emergency department due to symptoms of a cold which had been evolving over the previous 2 weeks, including cough but no expectoration, nighttime sweating, the sensation of dysthermia with fever that had not been measured and, recently, cough with purulent-hemoptoic expectoration and moderate-effort dyspnea. There was no cardiac asthma, nor any other associated symptom.
Physical examination revealed a normal general state, tachypnea at 28breaths/min, normal cardiopulmonary auscultation, oxygen saturation 85% (inspiratory oxygen fraction 21%), perimalleolar pitting edema, signs of chronic venous insufficiency, no signs of deep vein thrombosis, and symmetrical distal arterial pulse.
The lab work-up showed normal biochemistry and blood count, a D-dimer of 4 and partial respiratory insufficiency in the arterial blood gas analysis. Electrocardiogram demonstrated sinus tachycardia at 120beats/min. Chest radiography showed cardiomegaly with a loss of volume in both hemithoraces. Venous Doppler ultrasound of the lower limbs showed evidence of chronic left iliofemoral thrombosis and later ventilation-perfusion gammagraphy showed a low probability of thromboembolism.
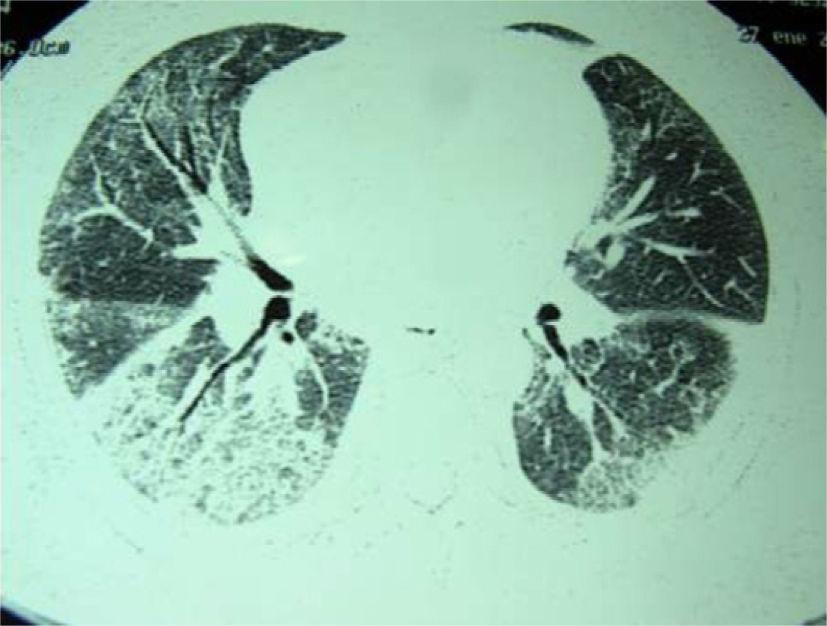
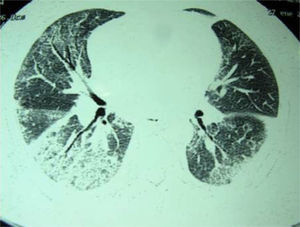
The respiratory function tests quantified a forced expiratory volume in one second (FEV1) of 1570ml (82%), forced vital capacity (FVC) 1880ml (72%), FEV1/FVC ratio 83% and carbon monoxide diffusing capacity 51%. Thoracic high-resolution computed tomography revealed mediastinal lymphadenopathies in the retrocaval-peritoneal, subcarinal and prevascular spaces and a diffuse ground-glass pattern distributed in both lung bases, as well as small bronchiectasis (Fig. 1).
Given the said findings, the patient was sent for lung biopsy using mini-thoracotomy, which gave the result of metastatic embolism due to carcinoma (without specifying the origin of the primary). Afterwards, the patient experienced a progressive deterioration and developed severe renal failure and hypoxemia as well as cardiorespiratory failure, therefore requiring immediate mechanical ventilation and support with vasoactive agents. In spite of the support measures used, severe hypotension led to cardiorespiratory arrest and finally the death of the patient. The anatomopathological examination of the autopsy revealed a neoplastic proliferation in glandular pattern in the endocervical canal, with abundant images of vascular and lymphatic invasion. These findings were also located in both lungs and in the cerebellum. In the end, the report determined papillary adenocarcinoma of the uterine cervix with metastasis in the retroperitoneal, paraaortic and mesenteric lymph nodes, vascular permeation (hematic and lymphatic) in the meningeal vessels of the cerebellum and in both lungs, causing pulmonary carcinomatous lymphangitis and diffuse alveolar damage, a finding which was related with the immediate cause of death of the patient.
Pulmonary tumor embolism is one of the most difficult causes of dyspnea to diagnose clinically. Most publications report isolated cases that are generally diagnosed in post-mortem studies.1 There are patients in whom the carcinoma has already been located when the dyspnea begins, but in others it is not possible to know about the location of the carcinoma.2 In all cases, the prognosis is very poor, often resulting in death due to either respiratory failure or secondary lung hypertension. Autopsy demonstrates the presence of tumor emboli in 26% of patients who die from cancer. The risk seems higher in patients with mucin-secreting adenocarcinomas, originating in the breasts, lungs, stomach or colon, but it has also been demonstrated in patients with hidden neoplasms, as in our case. As for the symptoms, dyspnea is present in most cases, and it is subacute and progressive.3 Pleuritic pain is also frequent. On physical examination, tachypnea and tachycardia are seen.4 The main findings on the chest radiography and computed tomography are cardiomegaly, the presence of prominent pulmonary arteries and interstitial infiltrates, if there is carcinomatous lymphangitis, as in the case that we present. Ventilation-perfusion gammagraphy may be normal or show multiple small, peripheral repletion defects. The diagnosis of pulmonary tumor embolism requires finding tumor cells in the lung vasculature. Cervical cancer is the second most frequent cause of morbidity and mortality related with cancer among women in developing countries: 371,200 new cases each year, with a 50% mortality rate. The incidence of invasive cervical cancer is related with age, with a mean age at the time of diagnosis of 47 in the United States. As for the histopathology, squamous carcinoma represents 80% of cervical cancers, adenocarcinoma 15% and adenosquamous carcinoma between 3% and 5%. The lesion may present as a superficial ulceration, an exophytic tumor of the external cervix or infiltration of the cervix. 15% of patients show no visible lesion because the carcinoma is inside the endocervical canal. Cervical cancer may propagate by direct extension in the uterus, vagina, parametrium, peritoneal cavity, bladder or rectum, and by lymphatic or hematogenous dissemination.5
Please cite this article as: Caballero Vázquez A, et al. Embolia pulmonar metastásica de un adenocarcinoma papilar de endocérvix. Arch Bronconeumol. 2012; 48:216-7.