Pulmonary capillary hemangiomatosis (PCH) is a low-grade pulmonary malignancy due to interstitial proliferation of capillary-like vessels occurring in patients of any age or sex. Prognosis is poor, with an estimated mean survival of 36 months.1
A 53-year old man, former smoker (39 pack-years), presented with worsening dyspnoea upon exertion and fatigue lasting 4 years. On admission, the patient was markedly tachypneic (respiratory rate 35 breaths/min) due to severe hypoxemia (40.5mmHg). Electrocardiographic examination showed a PR interval of 140 milliseconds, with pulmonary P waves, right bundle branch block, and a heart rate of 94 bpm. Findings of llaboratory tests were unremarkable. Complete pulmonary function tests were not performed, as the patient was not compliant. Spirometry showed a mild obstructive ventilatory defect not reversible upon broncho-dilation. Standard chest X-ray showed non-specific hilar congestion (not shown). Echocardiography revealed severe hypokinesia of the right ventricle along with a marked dilation of the right atrium and an estimated systolic pulmonary artery pressure of 70mmHg. Right heart catheterization was refused. Thromboembolic pulmonary disease was ruled out by contrast medium computed tomography (CT) (Fig. 1a). Main imaging findings are shown in Fig. 1b-c. The patient was started on oral therapy with carvedilol (12.5mg/day) and furosemide (125mg/day) along with supportive care, and discharged home. He was re-admitted after 3 months due to clinical worsening and further studies were carried out showing that more than 90% of cells from broncho-alveolar lavage stained positive for iron using Perl's, suggesting iron deposition, while lung biopsy was highly suggestive of PCH (Fig. 1d-e-f). The patient was referred to a lung transplantation center. Now, over 50 months after diagnosis, his clinical condition is still seriously compromised, though stable.
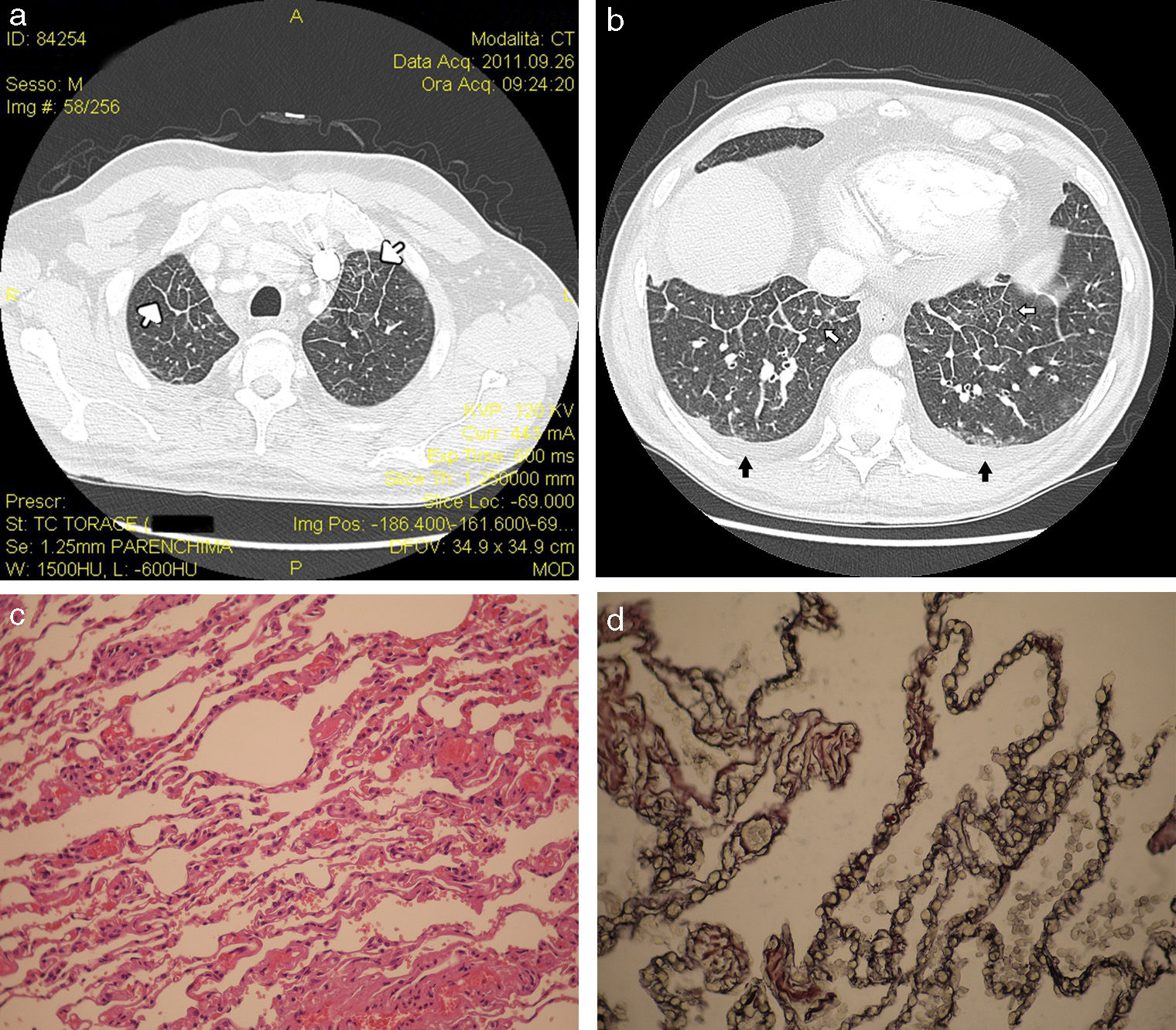
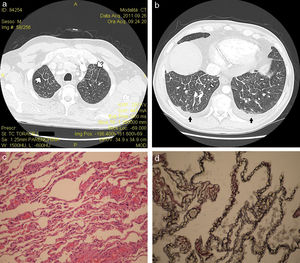
Volumetric reconstruction bone filter HRCT of the upper (a) and lower lung lobes (b) showing multifocal smooth interlobular septal tickening (white arrows) and bilateral mild pleural effusion (black arrows). Histopathological features (c) included thickening of interlobular septa and alveolar walls, filled by a growing proliferation of thin-wall blood vessels with little areas of lymphocytic interstitial inflammation (hematoxylin and eosin staining; magnification 30×). Endothelial cells stain positive with the CD31 monoclonal antibody (d). Magnification 40×.
We reported a case of PCH with an atypically long clinical course (6 years from clinical onset) along with a non-specific radiologic pattern. PCH may clinically masquerade as idiopathic pulmonary arterial hypertension (IPAH), or pulmonary veno-occlusive disease (PVOD). In PAH, differential diagnosis is crucial because pulmonary vasodilators may cause massive pulmonary edema in patients with PCH or PVOD.2 Radiological characterization with chest HRCT is useful, but lung biopsy is mandatory for confirmation.3 In our patient, chest HRCT was not typical for PCH due to the absence of centrilobular lung nodules,4 and final diagnosis was based on pathology data. PCH is characterized by alveolar wall thickening due to capillary proliferation. Infiltration and compression of pulmonary veins by new capillaries can result in secondary PVOD. PCH can be differentiated from IPAH or PVOD on the basis of the diameter of new pulmonary capillaries (larger in PVOD > PCH > IPAH) and the size of centrilobular nodules (wider in PCH>PVOD; absent in IPAH).5 Interstitial fibrosis, hemosiderosis and changes due to pulmonary arterial hypertension may also be found.
Clinicians and radiologists should bear PCH in mind, as early identification may improve patient management. PCH behaves like a low-grade non-metastatic vascular neoplasm, with a slow progressive clinical course. Prognosis is poor and lung transplantation is the best option.
Conflict of interestThe authors declare that they have no conflict of interests.
Please cite this article as: Rea G, Valente T, de Rosa N, Muto M, Berritto D, Bocchino M. Hemangiomatosis capilar pulmonar: un reto diagnóstico. Arch Bronconeumol. 2015;51:98–99.