IgG4-related disease is a newly described clinical-pathological entity that has a wide spectrum of clinical manifestations with a common histopathology: dense lymphoplasmacytic infiltrate, obliterative phlebitis and storiform fibrosis.1 The pancreas, salivary glands, and lymph nodes are the organs most frequently affected, although almost any part of the anatomy may be involved.1 The most common thoracic manifestation is the presence of mediastinal lymphadenopathies and pulmonary involvement that range widely from localized lesions to diffuse lesions.2 Pleural effusion has been described in 4% of patients and pericardial effusion in 2% of cases,3 but these manifestations usually occur along with other systemic presentations, and it is unusual to find them occurring in isolation.4,5 We have recently had the opportunity to treat a patient with a pleural and pericardial effusion who was diagnosed with IgG4-related disease, and we believe that it would be interesting to report the case.
Our patient was a 76-year-old woman who consulted with general malaise lasting several months, and a 7 kg weight loss, compounded in the last month with continuous non-radiating epigastric discomfort and generalized weakness. She reported no fever, cough or dyspnea at any time. She had been diagnosed with breast cancer 22 years earlier, treated with simple mastectomy. A recurrence 12 years later was treated with mastectomy and lymphadenectomy, chemotherapy and hormone therapy, and subsequent controls were normal.
On admission, the patient was afebrile, with blood pressure 135/70 mmHg and basal oxygen saturation 97%. Jugular venous pressure and cardiac auscultation were normal and left hemitorax hypoventilation was noted. No adenopathies, hepatomegaly or edema were detected. Chest X-ray showed massive left pleural effusion and transthoracic echocardiography showed a light pericardial effusion with abundant fibrin, and no signs of cardiac tamponade.
Laboratory tests, including blood count, biochemistry with renal function, liver enzymes, proteins, albumin, calcium, TSH, ACE, coagulation, urinalysis with urinary sediment and proteinuria (45 mg/24 h) were normal. The only remarkable values were ESR 68 mm and CRP 16 mg/dl.
Given the presence of pleural effusion of unknown etiology,6 a thoracentesis was performed that yielded serofibrinous pleural fluid with 4.8 g/dl proteins, LDH 317 U/l and normal ADA. Gram stain and pleural fluid culture were negative and cytology revealed 50% lymphocytes, with no malignant cells.
Chest-abdominal-pelvic computed tomography (CT) showed a massive left pleural effusion with complete atelectasis of the corresponding hemitorax and mediastinal shift to the contralateral side, minor right pleural effusion, and pericardial effusion. No pleural thickening, lymphadenopathies, or lung lesions were observed, although a radiologically nonspecific hypodense left renal cortical lesion measuring 3 × 2 cm was detected. Positron emission tomography was performed that showed only diffuse uptake in the inflamed pleura and pericardium. Mycoplasma pneumoniae, Coxiella burnetii, Legionella pneumophila, and HIV serologies and QuantiferonTB® were negative. Antinuclear antibodies (ANA), anti-neutrophil cytoplasmic antibodies (ANCAs), rheumatoid factor and complement were normal. The proteinogram showed a double monoclonal band in the beta-IgA lambda region of 0.8 g/dl, although bone marrow biopsy ruled out myeloma and amyloid staining in bone marrow and pleura was negative. Plasma levels in peripheral blood (954 cells/mL) were slightly raised, normal IgG4 levels were normal (90 mg/dl).
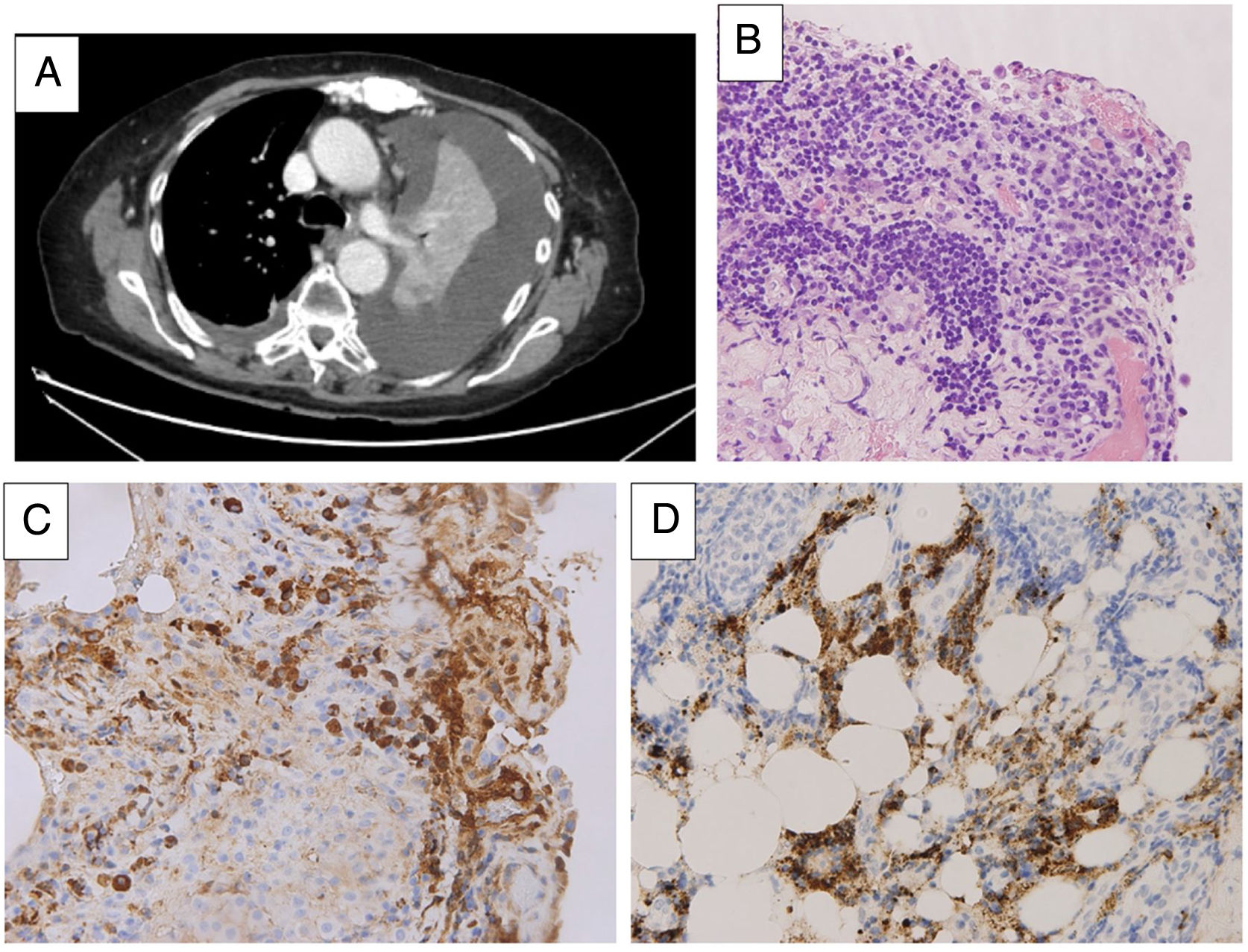
Video-assisted thoracoscopy was performed, revealing no nodularity, hyperemic pleura, and no other significant lesions. No clonal lymphoid population was observed in pleural fluid cytometry, and histological study showed fibrohemorrhagic pleuritis with severe mesothelial hyperplasia and dense plasmocellular infiltrate, with marked increase in IgG4-producing plasma cells (more than 50 cells per high-power field) and an IgG/IgG4 ratio of 49%. No neoplastic infiltration or granulomas were observed (Fig. 1).
A. Chest CT image showing left pleural effusion with pulmonary atelectasis. B. Pleural biopsy (hematoxylin-eosin) showing fibrohemorrhagic pleuritis with severe mesothelial hyperplasia and dense plasmocellular infiltrate. C. Pleural biopsy (immunohistochemical staining for IgG) showing abundant IgG-type plasmocellular infiltrate. D. Pleural biopsy (immunohistochemical staining for IgG4) showing marked increase in IgG4-producing plasma cells with areas of > 50 cells per high-power field and an IgG4/IgG ratio of 49%.
Treatment started with prednisone (40 mg daily), and pleural effusion diminished, the patient's general condition improved, and laboratory alterations (ESR and CRP) normalized.
Several weeks later, the patient was asymptomatic. A tapering corticosteroid regimen was initiated and rituximab was added to the regimen.7 An abdominal ultrasound performed 3 months after the start of treatment showed the persistence of the renal mass. IgG4-related disease may be associated with both cancerous8 and pseudotumor lesions9 (such as inflammatory renal pseudotumors10), so conservative management and close monitoring were undertaken before invasive testing.
Thoracic involvement in IgG4-related disease may affect the lung parenchyma, airways, mediastinum, and pleura. Histologically, storiform fibrosis and obliterative phlebitis may be absent,2 although the presence of >50 plasma cells per high-power field and a proportion of IgG4-producing plasma cells/IgG-producing plasma cells > 40% in pleural biopsy is highly suggestive of IgG4 pleuritis.1,2 Moreover, although serum IgG4 concentration is usually elevated in this disease (>135 mg/dl), up to 30% of patients have normal concentrations of this immunoglobulin,11 as in our case.
Patients who present rare manifestations of IgG4-related disease in isolation might not fulfil the criteria for the classification of the disease,12 so it is important to evaluate the available clinical data and complementary tests. Treatment is guided mainly by symptoms, although glucocorticoids are a mainstay. It has recently been reported that adding rituximab to the regimen helps reduce disease recurrence.7
Therefore, in spite of the low prevalence of pleural involvement in IgG4-related disease,13 given the good response to treatment with corticosteroids, it is advisable to rule out this entity in patients with predominantly lymphocytic exudative pleural effusion of unknown cause, even in the absence of other suggestive systemic manifestations. Multidisciplinary management of these cases is essential.14
Conflict of interestsThe authors declare that they have no direct or indirect conflict of interests related with the contents of this manuscript.
Please cite this article as: Tello-Sánchez M, Rodríguez-Duque MS, Loidi-López C, Martín-Arroyo J, González-Gay MÁ, Novo MF-A. Derrame pleural y pericárdico como única manifestación de enfermedad relacionada con IgG4. Arch Bronconeumol. 2020;56:597–599.