Diffuse interstitial lung disease (DILD) has a varied etiology, although in only 35% of cases is it possible to identify the causal agent.1 The disease can be triggered by a systemic a systemic drug that the patient may take for diverse clinical indications2,3 (chemotherapy agents, anti-arrhythmia medication, antibiotics, anticonvulsants, anti-inflammatories, anti-hypertension medication or illicit drugs) and should be the first etiology to consider when given a patient with DILD. We present the first reported case to date of interstitial pneumonitis secondary to treatment with a recently marketed hypertension drug, eprosartan. It belongs to the family of angiotensin II receptor blockers (ARBs), which are drugs that are widely used in the treatment of high blood pressure. In general, they are very well tolerated and the adverse effects that are most frequently reported are hypotension, deteriorated renal function, hyperkalemia, cough and angioedema. As for pulmonary toxicity secondary to ARBs, this is usually very uncommon, although there are reports of isolated cases of subacute interstitial pneumonia, eosinophilic pneumonia, bronchospasm, isolated cough, pleural effusion or thickening with positive ANA (drug-induced systemic erythematous lupus), laryngeal spasm and edema of the glottis.2 However, until now there were no reported cases of lung toxicity attributable to this new ARB.
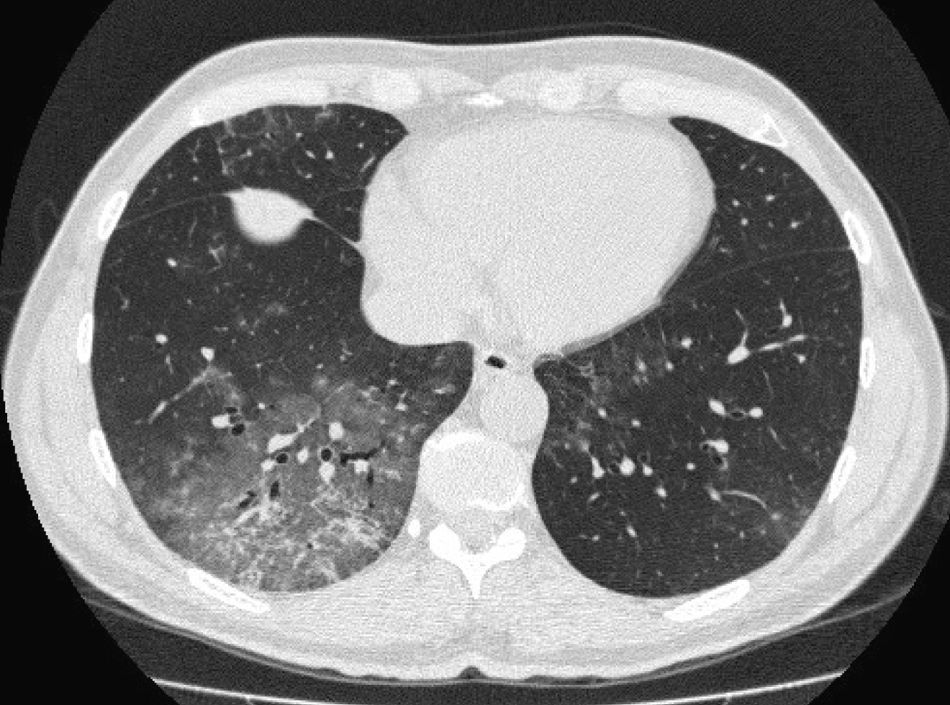
The patient is a 53-year-old man referred to our pulmonology consultation due to symptoms evolving over 5 months of cough with difficult expectoration that is sometimes hemoptoic and progressive moderate-exertion dyspnea. He had quit smoking 9 months before, with an accumulated consumption of 15 pack-years, with no reports of other toxic habits. He presented no previous respiratory pathology or occupational exposure to inhaled irritants (occupation: building engineer). The only pathological history was that 8 months before he had been diagnosed with mild high blood pressure, with no target organ injury, and had initiated treatment with eprosartan at a dosage of 600mg every 12h. Upon physical exploration, the subject was eupneic, with 16 Vf, transcutaneous oxygen saturation 98%, blood pressure 133/82mmHg, normal cardiac auscultation and lung auscultation with crackles in the lower half of the right hemithorax. Chest radiography presented small bilateral densities and chest CT showed a ground-glass pattern in the posterior basal segments of the right lower lobe and patchy areas in the left lower lobe (Fig. 1). Hemogram was normal, while biochemistry showed LDH 515U/l. Autoimmune studies with rheumatoid factor, ANA and ANCA were negative. Bronchoscopy showed no alterations; bacterial and mycobacterial cultures from bronchial suctioning were negative and bronchial cytology was normal. Transbronchial biopsy confirmed the diagnosis of interstitial pneumonitis that was predominantly lymphocytic, in the absence of vasculitis, granulomas, eosinophils and with limited fibrosis of the interstitium. Spirometry was normal, but the lung diffusion with helium (DLCO) was 41%. We considered the possibility that the interstitial lung disease was caused by the blood pressure medication that the patient was taking, so this drug was withdrawn. Twenty days later, the patient had experienced significant clinical improvements: the cough and hemoptoic sputum had stopped and the dyspnea had improved. Two months after the medication had been withdrawn, the patient was asymptomatic, and a follow-up thoracic CT showed a decrease in the interstitial pattern with changes that were limited only to the lingula; DLCO was 70%. A follow-up CT done 6 months later showed complete resolution of the interstitial alteration, and DLCO was normal. Two years after the withdrawal of the drug, the patient continues to have no clinical, functional or radiological alterations.
Due to the time correlation between starting with the medication and the onset of symptoms, the reversibility of the clinical and radiological findings with the withdrawal of the drug without having initiated treatment with systemic corticosteroids, the absence of another causal agent and the biopsy findings,4 we conclude that the interstitial pneumonitis was induced by eprosartan. Although hemoptoic sputum is not a typical symptom of drug-induced pneumonitis, this also resolved itself along with the cough.5 The interest of this communication lies in the fact that there are no other published cases of interstitial pneumonitis specifically associated with eprosartan. We should always keep in mind the possibility of DILD with any drug, especially if it has been recently marketed.
FundingThis study has received no funding.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Pérez-Lluna L, et al. Neumonitis intersticial secundaria a eprosartán. Arch Bronconeumol. 2012;48:485.