Tracheobroncomalacia (TBM) is a chronic condition characterized by weakening of the tracheobronchial cartilage, resulting in excessive dynamic airway collapse, especially during expiration. Tracheobronchoplasty (TBP), is the most common surgical repair for TBM. However, it is technically demanding and carries significant perioperative risks.1 Recently, robotic TBP (R-TBP) has been introduced,2 enhancing the traditional open technique.
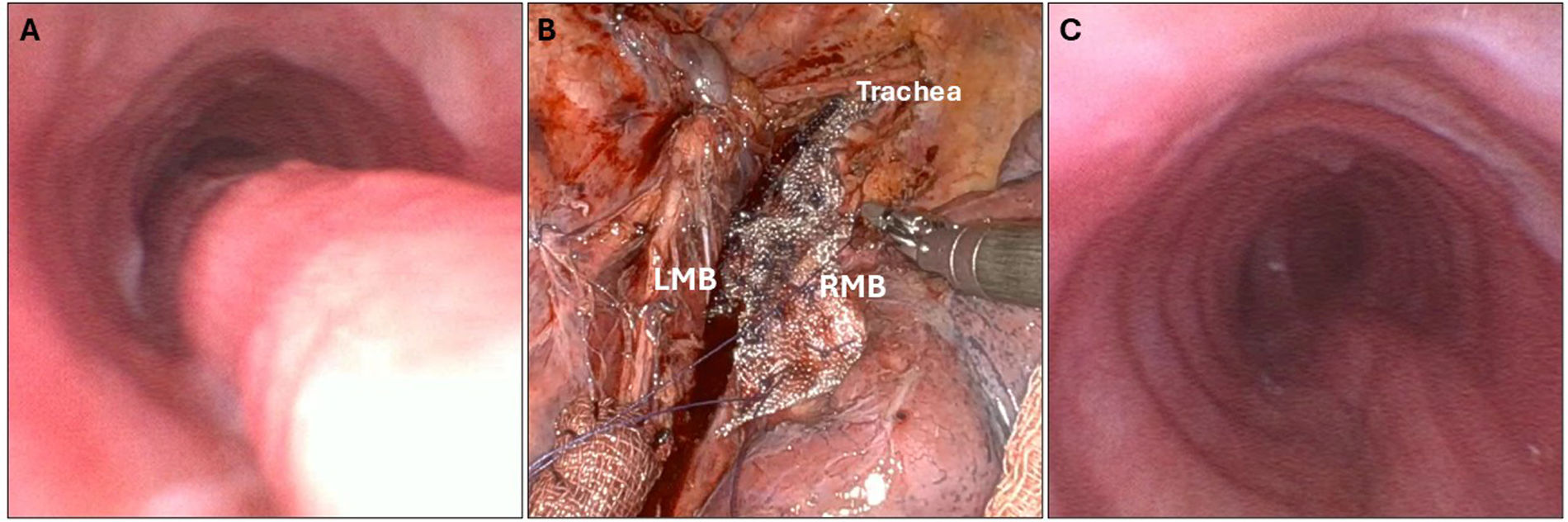
We present the case of a 53-year-old woman with an unremarkable medical history who was diagnosed with COVID-19 pneumonia two years prior, requiring hospital admission but no orotracheal intubation. Following recovery, she developed a persistent cough and dyspnoea. Further evaluation, including awake dynamic bronchoscopy and dynamic computed tomography, revealed a tracheobronchial collapse exceeding 90% (Fig. 1A), leading to a diagnosis of TBM. Pulmonary function tests (PFT) showed a forced expiratory volume in 1 second (FEV1) of 74% and a forced vital capacity (FVC) of 65%. The patient had a poor quality of life, with a St George's Respiratory Questionnaire (SGRQ) score of 86.4 and a 6-minute walk test (6-MWT) distance of 120m (32% of predicted). Initial management included 24-h continuous positive airway pressure therapy, followed by placement of a self-expanding Y-shaped metallic stent for 6 months to assess symptom improvement and/or resolution. Although initially well tolerated, the patient progressively developed mucus plugging and recurrent infections, resulting in limited symptomatic relief. Due to persistent symptoms and severity of TBM, R-TBP was performed. The procedure involved suturing a polypropylene mesh to the posterior cartilaginous rings of the trachea, both mainstem bronchi, and the bronchus intermedius, with plication and fixation of the redundant posterior membranous wall to the mesh (Fig. 1B and C) as previously described by Lazzaro et al.2 The postoperative period was uneventful, and the patient was discharged on day eight. At two months, she reported complete symptom resolution, with improved PFT (FEV1: 89% and FVC: 77%), SGRQ scores (51.3) and a 6-MWT distance of 300m (81% of predicted).
(A) Preoperative awake dynamic bronchoscopy showing >90% expiratory collapse of the trachea, consistent with severe tracheobronchomalacia. (B) Intraoperative view depicting the suturing of the polypropylene mesh to the posterior wall of the trachea and mainstem bronchi during robotic-assisted tracheobronchoplasty. (C) Postoperative awake bronchoscopy demonstrating successful plication and stabilization of the posterior membranous tracheal wall.
Diagnosis and management of TBM remain challenging. A thorough diagnostic evaluation is essential to accurately confirm TBM, differentiate it from excessive dynamic airway collapse (EDAC),3 and assess severity. This evaluation includes dynamic computed tomography with ultralow-dose forced exhalation imaging and cinematic reconstructions, as well as awake dynamic bronchoscopy. TBP is indicated in patients with >90% dynamic airway collapse and persistent symptoms despite optimal medical treatment.4 The primary goal of surgery is to stabilize the posterior membranous wall of the trachea and bronchi. Traditionally, TBP has been performed via right posterolateral thoracotomy. However, the robotic approach has emerged in recent years as a safe and less invasive alternative that reduces the morbidity of open surgery.4 R-TBP offers several technical advantages, including enhanced three-dimensional visualization, precise dissection and suturing with wristed instruments, and improved surgeon ergonomics.
Collectively, these features may underlie the favourable outcomes described in the literature, including substantial improvements in pulmonary function and quality of life.4,5 These results further support the role of R-TBP as a safe and effective surgical option for appropriately selected patients with severe TBM.
CRediT Authorship Contribution StatementDeclaration of substantial contributions to:
- 1.
Study conception and design: All authors.
- 2.
Acquisition of data: All authors.
- 3.
Analysis and interpretation of data: All authors.
- 4.
Drafting of the manuscript or critical revision for relevant intellectual content: MTGH, MFJ.
- 5.
Final approval of the version to be submitted: All authors.
All authors have read and agreed to the published version of the manuscript.
Declaration of Generative AI and AI-assisted Technologies in the Writing ProcessThe authors declare that any of the material has been produced with the help of any artificial intelligence software or tool.
FundingNone declared.
Conflicts of InterestThe authors declare no conflicts of interest.