Venous thromboembolism (VTE) can have long-term consequences, such as post-thrombotic syndrome (PTS) or chronic thromboembolic pulmonary hypertension (CTPH). Recurrent thrombosis or bleeding can occur during follow-up. These post-VTE complications can have adverse effects on quality of life (QoL). Previous research on QoL after VTE included only middle-aged subjects.1 Although the elderly are more prone to VTE2 and the proportion of aged individuals is increasing worldwide,3 there are no data on QoL in this population. We investigated the QoL of a cohort of patients older than 75 y after VTE and analyzed the determinants 18 mo post-VTE.
This was a prospective observational study of consecutive patients older than 75 y with acute VTE (pulmonary embolism [PE] and/or deep vein thrombosis [DVT]) who presented to Hospital Universitario 12 de Octubre, Spain between 2015 and 2017. Comorbidity was measured using the non-age-adjusted Charlson index,4 and the functional status of the patients in terms of basic activities of daily living was assessed using the Barthel index (BI) (score range: 0-100).5 Depression was established based on a review of the patient's history.
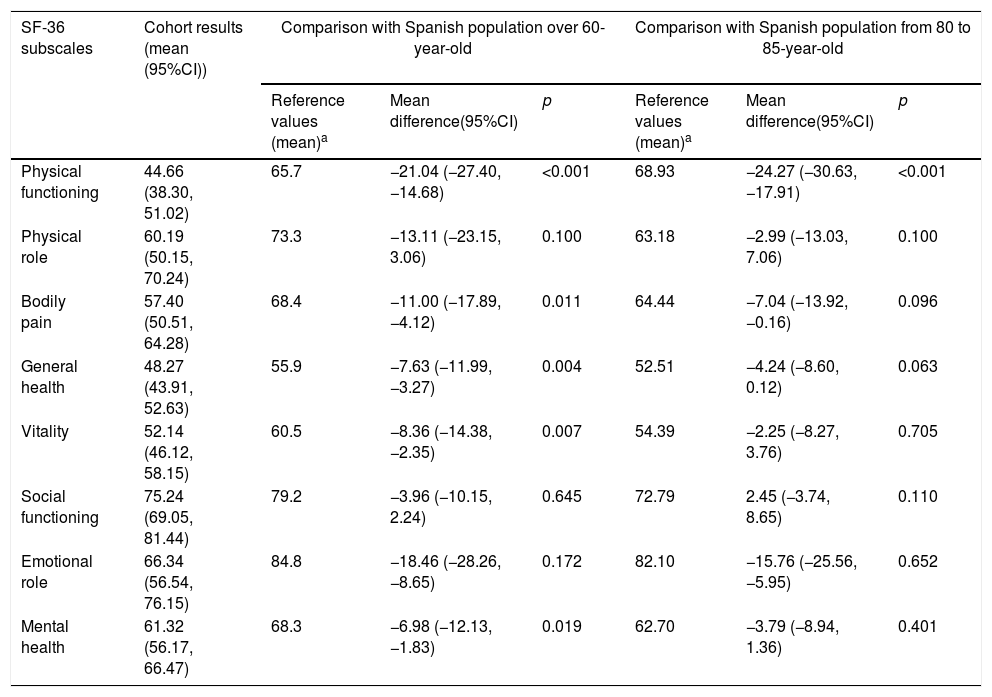
Clinical practitioners registered VTE recurrence and major bleeding. A diagnosis of CTPH required documented pulmonary hypertension (echocardiography or right catheterization) and evidence of chronic thrombosis on ventilation-perfusion scintigraphy or computed tomography at least 3 mo post-PE. The Ginsberg clinical scale was used to diagnose PTS 18 mo after DVT.6 To assess QoL, we administered the Short Form 36 (SF-36) survey 18 mo after VTE and calculated the mean and its 95% confidence interval (95%CI) for each SF-36 subscale and two summary measures (physical summary measure [PSM] and mental summary measure [MSM]).7,8 The subscale values ranged from 0 to 100, with higher scores corresponding to better health status. The summary measures were “norm-based.” Thus, scores above or below 50 were considered above or below the mean of the reference population. We compared the results with those previously published in a Spanish population of the same age.9 A difference of 5 points or more in any subscale was accepted as clinically and socially relevant,7 and a p-value lower than 0.0005 was considered statistically significant, according to a Bonferroni correction for multiple comparisons. Finally, we pre-selected variables related to QoL in older and VTE patients.1,10–12 We analyzed their impact on the summary measures using multivariable linear regression. The variables included in the multivariable models for PSM were age, sex, Charlson index, BI, recurrent VTE, bleeding, CTPH, and PTS. Depression was included in the multivariable models for MSM.
The local ethics committee approved this study. Prior to enrollment, the subjects were informed about the study, and provided written or verbal informed consent.
In total, 101 of 151 (67%) patients completed the SF-36 questionnaire 18 mo post-VTE. The median age was 81 y (interquartile range [IQR]: 79, 86), 61% were females, and 19% had cancer. The median BI was 100 (IQR: 85, 100), and the Charlson index was 1 (IQR: 0, 2). Eighty-two% of patients had experienced a PE, with or without DVT. VTE recurrence, major bleeding, CPTH, and PTS occurred in 8%, 5%, 3%, and 10% of patients, respectively. The means for the two summary measures were lower than the values for the Spanish population older than 60 y (PSM, 45.51 [95%CI: 43.68, 47.35]; MSM, 47.30 [95%CI: 44.95, 49.65]) (Table 1). After the multivariable analysis, the BI was the only determinant related, clinically and statistically, to PSM at the 18-mo follow-up (B-coefficient: 0.119 [95%CI: 0.043, 0.195], p=0.002). Neither the Charlson index nor VTE-related factors were related to PSM (Charlson B-coefficient: −0.126 [95%CI: −1.238, 0.986], recurrence B-coefficient: −3.650 [95%CI: −11.051, 3.751]; bleeding B-coefficient: 1.846 [95%CI: −2.934, 6.625]; CTPH B-coefficient: 2.182 [95CI%: −6.659, 11.022]; PTS B-coefficient: −5.212 [95%CI: −10.980, 0.557]). No factors were related to MSM after the multivariable analysis.
Results of SF-36 questionnaire: comparison with Spanish population.
| SF-36 subscales | Cohort results (mean (95%CI)) | Comparison with Spanish population over 60-year-old | Comparison with Spanish population from 80 to 85-year-old | ||||
|---|---|---|---|---|---|---|---|
| Reference values (mean)a | Mean difference(95%CI) | p | Reference values (mean)a | Mean difference(95%CI) | p | ||
| Physical functioning | 44.66 (38.30, 51.02) | 65.7 | −21.04 (−27.40, −14.68) | <0.001 | 68.93 | −24.27 (−30.63, −17.91) | <0.001 |
| Physical role | 60.19 (50.15, 70.24) | 73.3 | −13.11 (−23.15, 3.06) | 0.100 | 63.18 | −2.99 (−13.03, 7.06) | 0.100 |
| Bodily pain | 57.40 (50.51, 64.28) | 68.4 | −11.00 (−17.89, −4.12) | 0.011 | 64.44 | −7.04 (−13.92, −0.16) | 0.096 |
| General health | 48.27 (43.91, 52.63) | 55.9 | −7.63 (−11.99, −3.27) | 0.004 | 52.51 | −4.24 (−8.60, 0.12) | 0.063 |
| Vitality | 52.14 (46.12, 58.15) | 60.5 | −8.36 (−14.38, −2.35) | 0.007 | 54.39 | −2.25 (−8.27, 3.76) | 0.705 |
| Social functioning | 75.24 (69.05, 81.44) | 79.2 | −3.96 (−10.15, 2.24) | 0.645 | 72.79 | 2.45 (−3.74, 8.65) | 0.110 |
| Emotional role | 66.34 (56.54, 76.15) | 84.8 | −18.46 (−28.26, −8.65) | 0.172 | 82.10 | −15.76 (−25.56, −5.95) | 0.652 |
| Mental health | 61.32 (56.17, 66.47) | 68.3 | −6.98 (−12.13, −1.83) | 0.019 | 62.70 | −3.79 (−8.94, 1.36) | 0.401 |
This study showed that older VTE patients reported worse QoL than that of older patients in the general Spanish population, with mainly physical function affected. Although several studies concluded that VTE had a negative impact on the QoL of middle-aged people,1 a recent study13 reported that QoL 1 y after VTE improved to a level similar to that of a healthy population. This finding differs from that found in our study, in which both summary measures were below the population norms after 18 mo. We ascribe this disparity to the age difference of the study populations. The disability prevalence increases among the aged,14 and it have been linked to a reduced QoL in several disorders.12,14,15 In the present study, the BI was the only independent determinant of a low PSM score.
Our study had some limitations. First, the small sample size limited the power to detect an association between QoL and long-term complications. Thus, no conclusions can be drawn about the impact of recurrence, bleeding, CTPH or PTS on QoL. In addition, this was a monocentric study, which limits its external validity. Finally, we did not use a disease-specific QoL questionnaire, which could have been more sensitive than the SF-36 survey in detecting differences in QoL. However, previous studies on VTE and QoL employed the SF-36 survey and demonstrated good reliability and validity.1,13
Despite the aforementioned limitations, to our knowledge, this is the first study to examine QoL in aged VTE patients. The response rate in the present study was similar to that of earlier research1 and can be attributed to the challenging nature of follow-ups of elderly populations. Given that VTE-related complications usually occur within the first 2 y,1 we estimate that an average follow-up of 1.5 y should be sufficient to identify the impact of most of these complications on QoL.
In our cohort, older VTE patients reported worse QoL than that of the general population of the same age, and the BI was the only independent determinant of QoL. Although our study cannot lead to firm conclusions, the results may be relevant for future research on the influence of VTE-related complications or treatment on the QoL of patients.