We present the case of a 51-year-old woman, with no relevant medical history, non-smoker. Her occupational history was limited to domestic cleaning. A significant family history included her mother, who had died of an undetermined pulmonary disease in our institution at the age of 58, more than 15 years earlier.
Ten years prior to the current evaluation, the patient was admitted to the emergency department with episodic fever, polyarthralgia, muscle weakness, and a pruritic macular rash. Laboratory studies revealed only mild leukocytosis and slight transaminase elevation, with negative autoimmune serology. Chest radiography showed bilateral apical thickening. High-resolution computed tomography (HRCT) demonstrated bilateral pleural thickening with subpleural fibrosis and mild basal reticulation. Bronchoscopy yielded negative microbiological studies; lymphocytic predominance (20%) was noted. Based on a rheumatologic evaluation, after discarding other causes and using the Yamaguchi criteria [1], Still's disease was diagnosed. Initial treatment with 60mg prednisone was later transitioned to steroid-sparing agents, including azathioprine, mycophenolate and cyclophosphamide. The patient was ultimately maintained on tocilizumab due better systemic disease control with this drug.
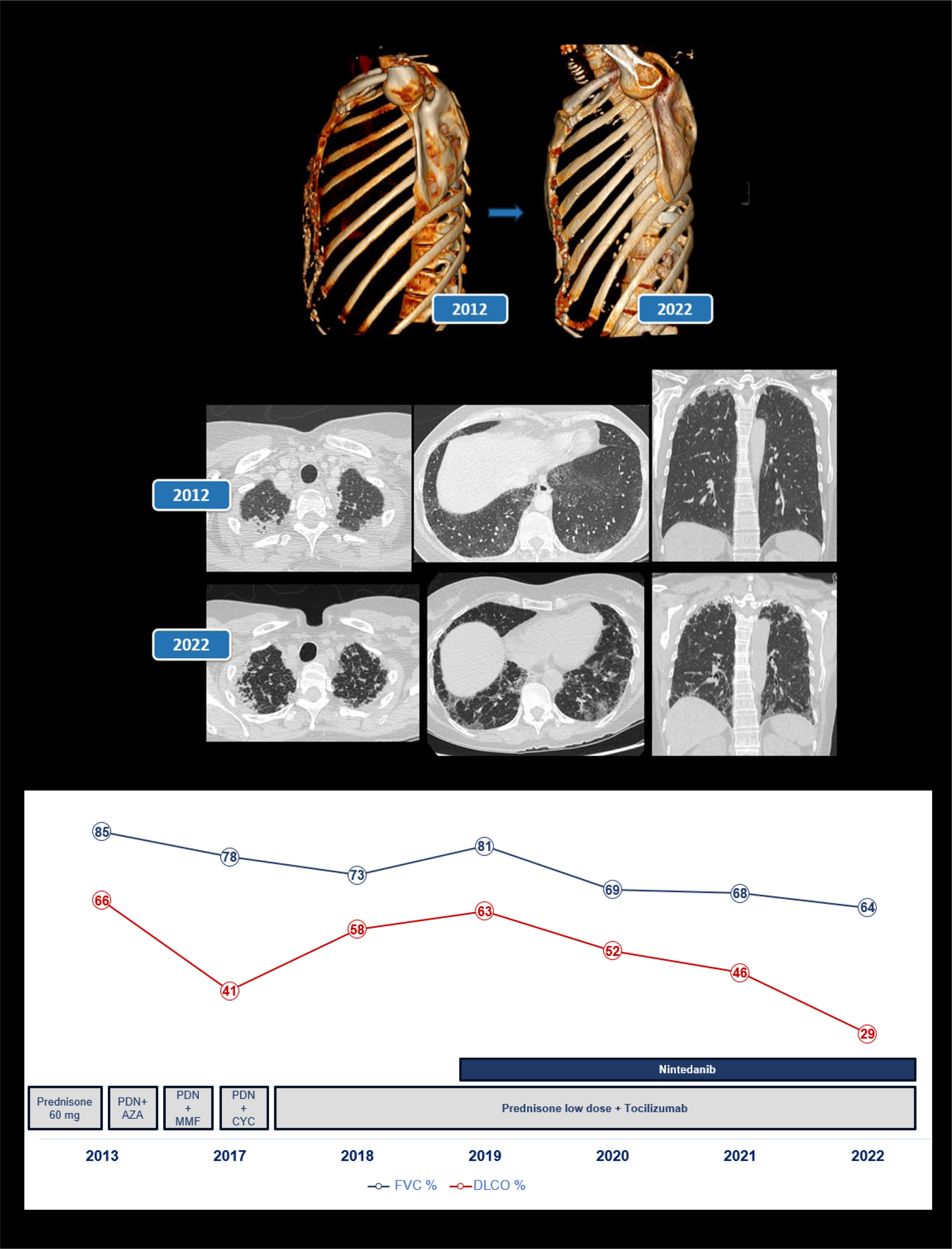
Despite relative stability of her systemic disease, pulmonary involvement progressed insidiously. HRCT demonstrated progressive upper lobe pleuroparenchymal thickening and lower lobe fibrotic consistent with a fibrotic nonspecific interstitial pneumonia (NSIP) pattern and there was a progressive deterioration of pulmonary function (Fig. 1).
Radiological progression of the patient over a 10-year follow-up period. Serial high-resolution computed tomography (HRCT) scans demonstrate progressive upper lobe pleuroparenchymal fibroelastosis and development of fibrotic nonspecific interstitial pneumonia (NSIP) changes in the lower lobes, characterized by subpleural fibrosis, reticulation, and traction bronchiolectasis. In addition, flattening of the anterior thoracic cage with deep depression of the suprasternal notch is clearly evident. The lower graph shows the evolution of respiratory function expressed in terms of forced vital capacity (FVC) and diffusing capacity for carbon monoxide (DLCO) as percentages. In addition, a legend is included indicating the treatments the patient received at each point in time. PRD: prednisone. AZA: azathioprine. MMF: mycofenolate. CYC: cyclophosphamide.
During her follow-up, her mother's medical record and chest HRCT were reviewed. Also, archived lung biopsy specimens from her late mother's autopsy were re-examined. Histopathology revealed markedly thickened visceral pleura with dense subpleural fibrosis extending into the lung parenchyma, associated with alveolar septal elastosis. These findings were diagnostic of pleuroparenchymal fibroelastosis (PPFE). Both cases were very similar, so, as the patient did not desire a lung biopsy and taking everything into account, she was diagnosed with PPFE associated with fibrotic NSIP in the lower lobes, in the setting of adult-onset Still's disease.
Given fulfillment of NSIP with progressive pulmonary fibrosis criteria, antifibrotic therapy was initiated during follow-up. It was well tolerated but her condition continued to deteriorate. The patient was evaluated for lung transplantation but recently died due to an acute exacerbation of her interstitial lung disease.
To our knowledge, this represents the first reported case of pleuroparenchymal fibroelastosis (PPFE) associated with adult-onset Still's disease, with a clear familial component. PPFE is an exceptionally rare interstitial lung disease, first described in 2004 [2] and formally recognized in international guidelines in 2013 [3]. For this reason, our patient's mother could not have been diagnosed with this entity at the time of her illness.
Since its initial description, reported cases have increased. PPFE is characterized by dyspnea, nonproductive cough, and chest pain. The disease may be idiopathic or secondary to other causes, such as connective tissue disease [4], as in our patient. Median survival is approximately 11 years, though rapidly progressive cases may deteriorate within 3–5 years.
Radiological findings definite PPFE by bilateral pleural thickening with associated subpleural fibrosis in the upper lobes. Typical features also include flattening of the thoracic cage and a deep depression of the suprasternal notch.
Currently, no treatment has demonstrated proven efficacy in isolated PPFE. Limited data suggest that patients may be treated by lung transplantation, although it is associated with high post-operative morbi-mortality rates [5].
We believe this case is of particular importance, as both PPFE and adult-onset Still's disease are rare entities, and to date, no previous report has described their association.
Authors’ contributionAll authors participated in the diagnosis and treatment of the clinical case described, as well as in the writing and preparation of the manuscript.
Generative AIThe authors did not use artificial intelligence in the preparation of this manuscript.
FundingThe authors declare that they have not received any funding.
Conflicts of interestThe authors declare that they have no conflicts of interest to disclose.