Localization and palpation of pulmonary nodules measuring less than 20mm can be particularly challenging during minimally invasive surgery. Preoperative marking not only facilitates identification but also helps reduce surgical time and the risk of conversion to thoracotomy [1]. The availability of endoscopic equipment with near-infrared imaging enables the detection of nodules after the application of fluorescent contrast agents such as indocyanine green (ICG) [2].
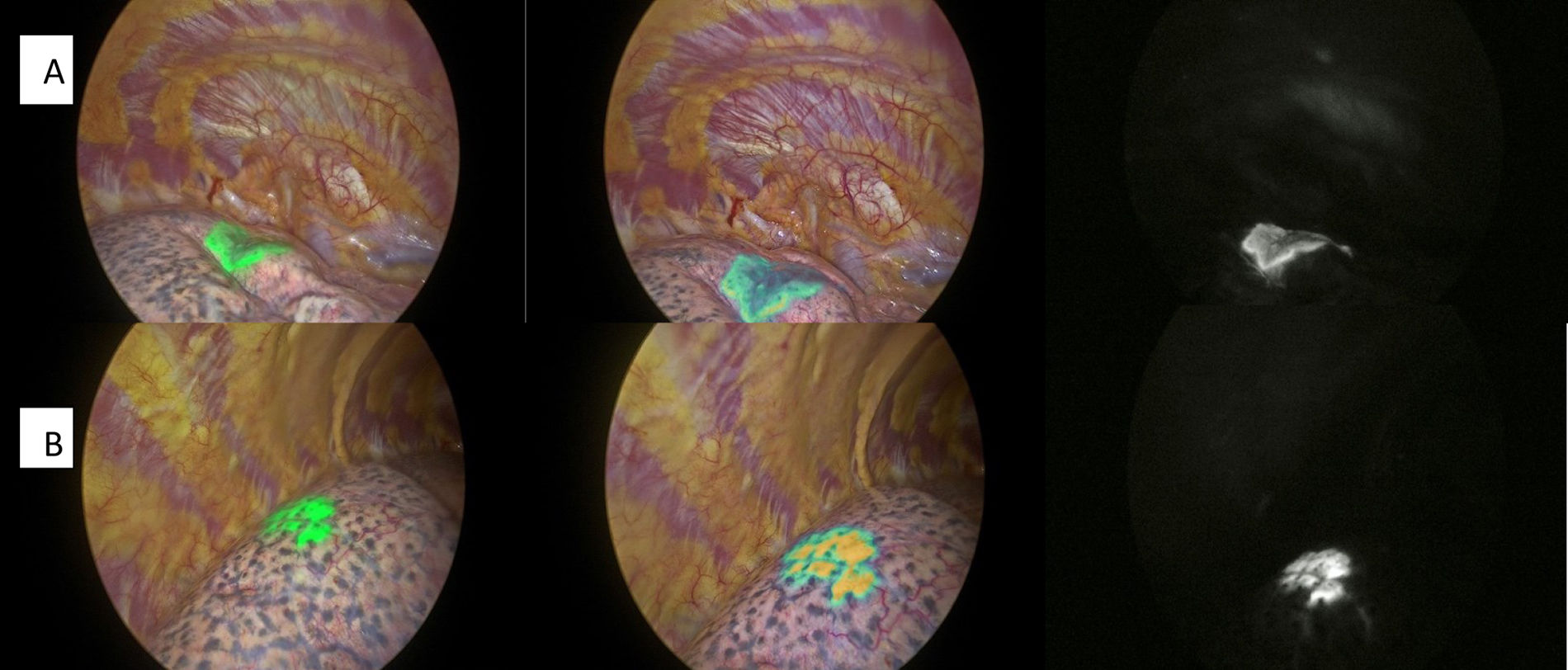
We present the case of a 43-year-old woman with a history of rectal adenocarcinoma. She had been treated with neoadjuvant chemoradiotherapy and surgery one year earlier. Two suspicious right pulmonary nodules, located in the upper and lower lobes, were marked with ICG on the morning before surgery. After anesthetic induction, the anesthesiology team encountered difficulties with selective left bronchial intubation. Several attempts failed, leading to bradycardia and significant desaturation due to airway edema. Urgent orotracheal intubation was required, along with administration of adrenaline and atropine, until respiratory and hemodynamic stability was restored. Given these complications, the procedure was postponed. The patient recovered without incident and was discharged 48h later. One week after the incident, the patient underwent surgery for resection of the known nodules. Selective intubation was performed without complications, as the initial difficulty had been related solely to the first maneuver. Given the complications during the first intervention, we opted not to repeat the marking procedure, as the nodules were peripheral and likely to be palpable during conventional VATS. This also avoided subjecting the patient to an additional double pulmonary puncture. Upon selecting infrared light on the endoscope, persistent ICG fluorescence was still detectable at the original puncture sites (Fig. 1), enabling the successful resection of both nodules. Histology confirmed metastasis from rectal adenocarcinoma, with resection margins larger than the metastatic lesions.
Different ICG-related surgical techniques may be chosen according to the characteristics of the nodule and patient-specific factors, aiming to ensure procedural success while minimizing complications [3]. In our center, ICG is administered using a 2ml syringe with a mixture of 0.4ml ICG (2.5mg/ml) and 0.8ml of saline, as described by Li [4]. The same author reported a similar experience six days after ICG administration [5]. ICG may be a good alternative to other localization techniques for pulmonary nodules, due to its low toxicity and good visualization. Unlike Tc99, it does not involve radioactive materials or require the use of a gamma probe. However, its usefulness is limited for deep lesions [6]. The duration of ICG retention in lung tissue after percutaneous administration remains unknown, but these findings suggest absorption may exceed one week. This feature may prove valuable in planning future surgical procedures involving delayed resections.
Author contributionsM. Arrarás, K. De Aguiar, and M. Barrios contributed to the conception, drafting, and critical revision of the manuscript, approved the final version, and take responsibility for its content.
Artificial intelligence involvementThe authors confirm that no artificial intelligence tools were used in the preparation of this manuscript.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interestAll authors declare no conflicts of interest that could directly or indirectly influence the content of the manuscript.