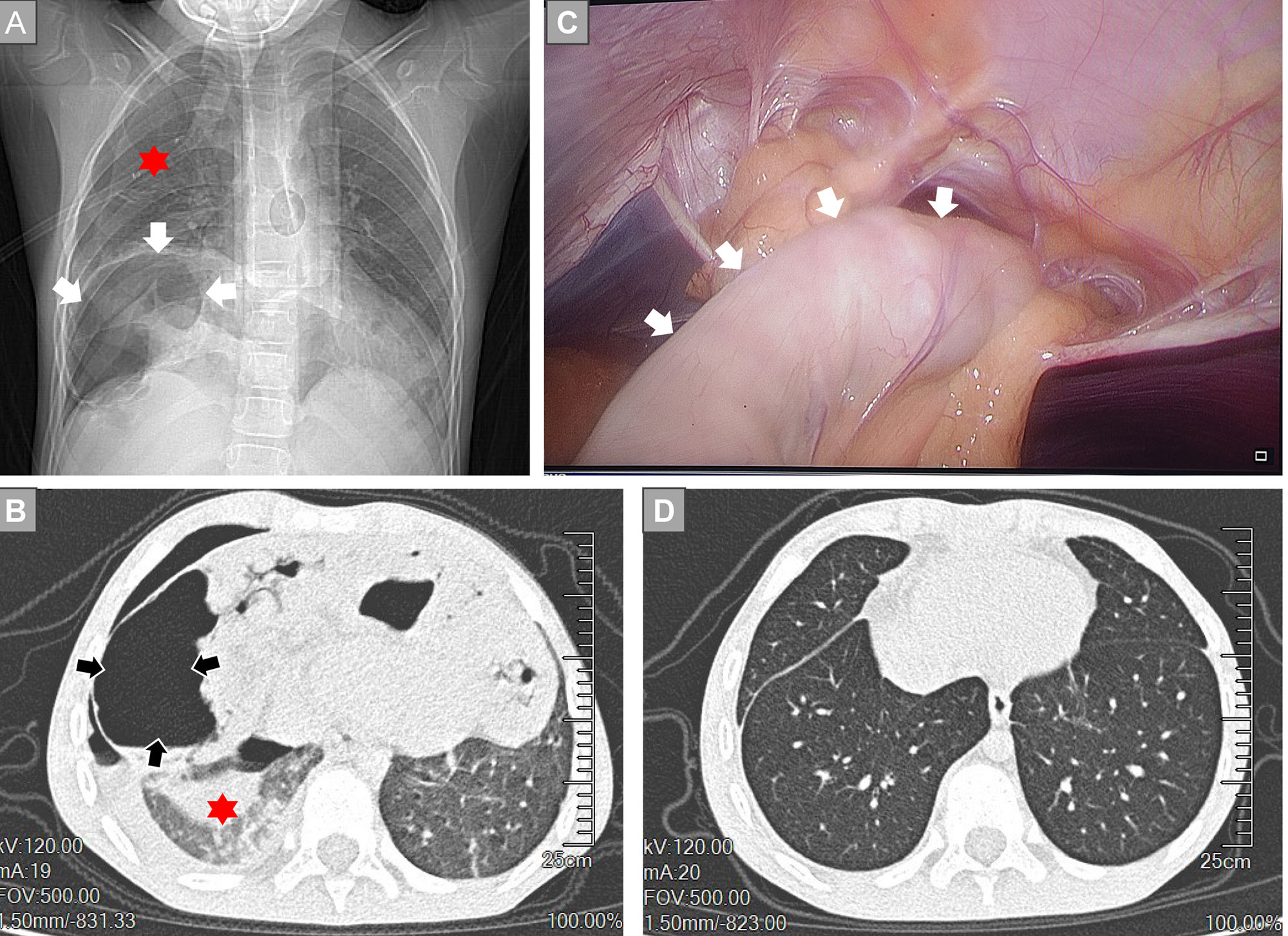
An 8-year-old boy presented after 16h of abrupt chest pain, dyspnea, and profuse vomiting. He had no prior cardiopulmonary or gastrointestinal disease. On arrival he was pale and distressed; heart rate 134beats/min, blood pressure 94/55mm Hg, respiratory rate 28breaths/min, and oxygen saturation 88% despite FiO2 0.6 via nasal cannulae. Breath sounds were diminished over the right lung, and the abdomen was diffusely tender with reduced bowel sounds. Chest radiography and computed tomography (CT) showed focal bronchial compression with right-sided atelectasis and a parasternal (Morgagni) hernia containing transverse colon, omentum, and a portion of liver (Fig. 1 A and B). Emergency thoracoscopic-assisted repair was undertaken (Fig. 1C). Approximately 5cm of gangrenous transverse colon were resected, followed by primary end-to-end anastomosis. Postoperatively, mechanical ventilation with repeated recruitment maneuvers was required; hypoxemia persisted for 2 days, and CT confirmed right-sided atelectasis. By postoperative day 5, oxygenation improved (SpO2>97%) and the endotracheal tube was removed. Two months later, CT showed normal aeration of both lungs (Fig. 1D). Morgagni hernia, a rare form of congenital diaphragmatic defect with an estimated prevalence of one in 2000–5000 live births, may occasionally present with ischemic bowel complications, including obstruction or incarceration, though such manifestations are infrequent [1]; CT is the diagnostic standard, laparoscopic repair is preferred, and complicated presentations with ischemic bowel and respiratory failure mandate care at tertiary centers. This case highlights the relevance of late diagnosis in Morgagni hernias, which are typically recognized and treated at birth or in early childhood, with late presentations reported in 0.17–6% of cases [2].
Morgagni hernia with subtle onset in an 8-year-old boy presenting with acute chest pain, dyspnea, and severe vomiting. (A) Chest radiograph illustrating a parasternal hernia. The arrow marks abdominal bowel loops that have entered the thoracic cavity through a focal diaphragmatic defect. The red asterisk highlights compressed lung parenchyma; (B) Chest computed tomography demonstrating a parasternal hernia. The arrow indicates herniated abdominal bowel within the thorax. The red asterisk denotes compressed pulmonary tissue; (C) Thoracoscopic view of the parasternal hernia. The arrow points to intrathoracic herniated bowel; (D) Follow-up chest CT obtained two months after discharge shows normally re-expanded lung tissue.
Yu Shan: Conceptualization, Clinical Management, Writing – Original Draft, Supervision. Jian Feng: Radiological Analysis, Figure Preparation, Writing – Review & Editing. Cheng Xu: Literature Review, Writing – Review & Editing.
Informed consentInformed consent has been obtained from the patient.
Declaration of generative AI and AI-assisted technologies in the writing processDuring the preparation of this work the author(s) used ChatGPT in order to enhance language quality and readability. After using this tool/service, the author(s) reviewed and edited the content as needed and take(s) full responsibility for the content of the published article.
FundingNone.
Conflicts of interestThe authors state that they have no conflict of interests.