Identifying high-risk patients is fundamental to slowing disease progression in mild-to-moderate COPD. Over one-fifth of these patients have impaired ventilatory efficiency, strongly associated with advanced disease severity, while its unclear prognostic value for high-risk case identification persists.
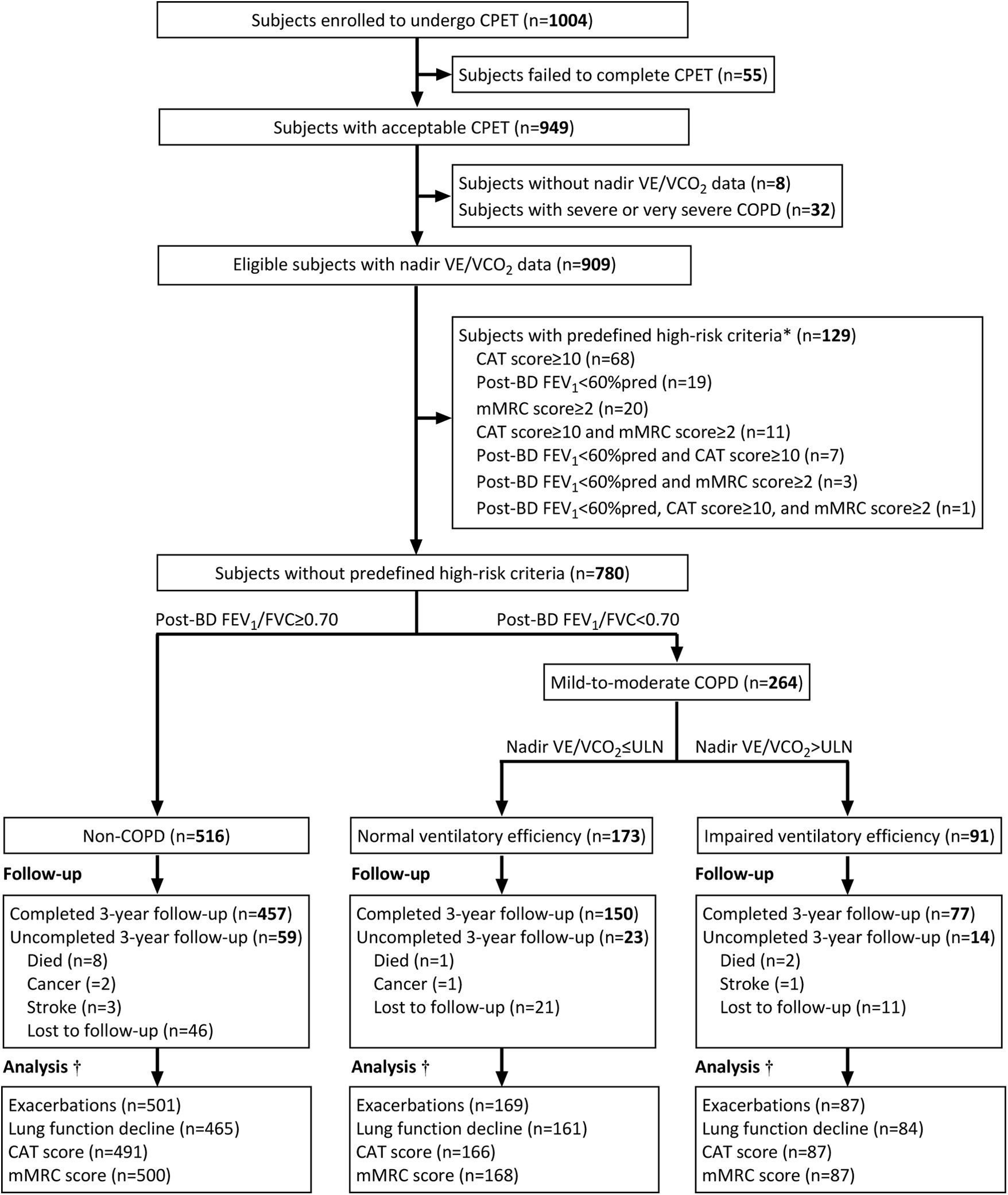
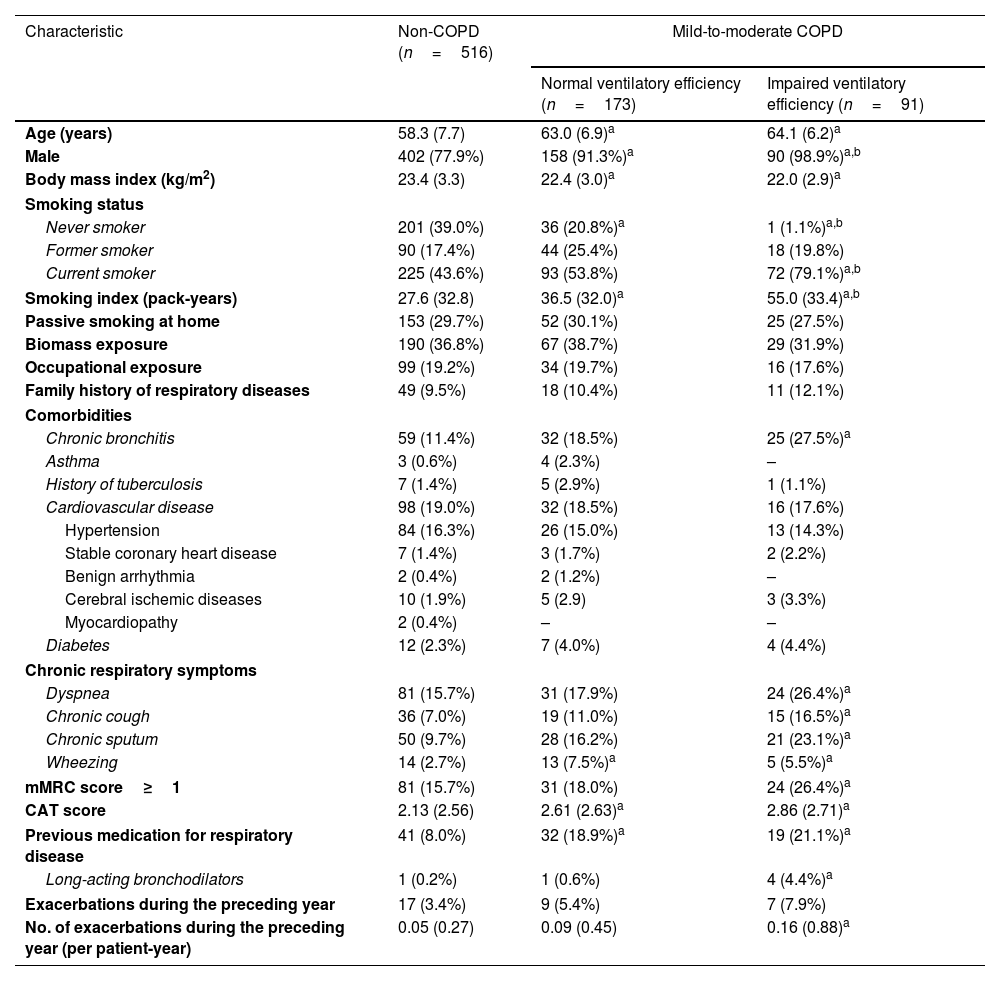
MethodsThis was a prospective cohort study conducted from July 2019 to September 2024 (encompassing the COVID-19 pandemic period) in China. Non-COPD subjects and mild-to-moderate COPD patients who completed questionnaires, lung function tests and cardiopulmonary exercise tests at baseline were annually followed up over 3 years. Subjects with predefined high-risk criteria, including CAT score≥10, mMRC score≥2, postbronchodilator FEV1<60% predicted, and frequent exacerbations, were further excluded. Impaired ventilatory efficiency was defined as a nadir minute ventilation/CO2 output≥the upper limit of normal. Outcomes included annual lung function decline, exacerbation risks, and symptom scores.
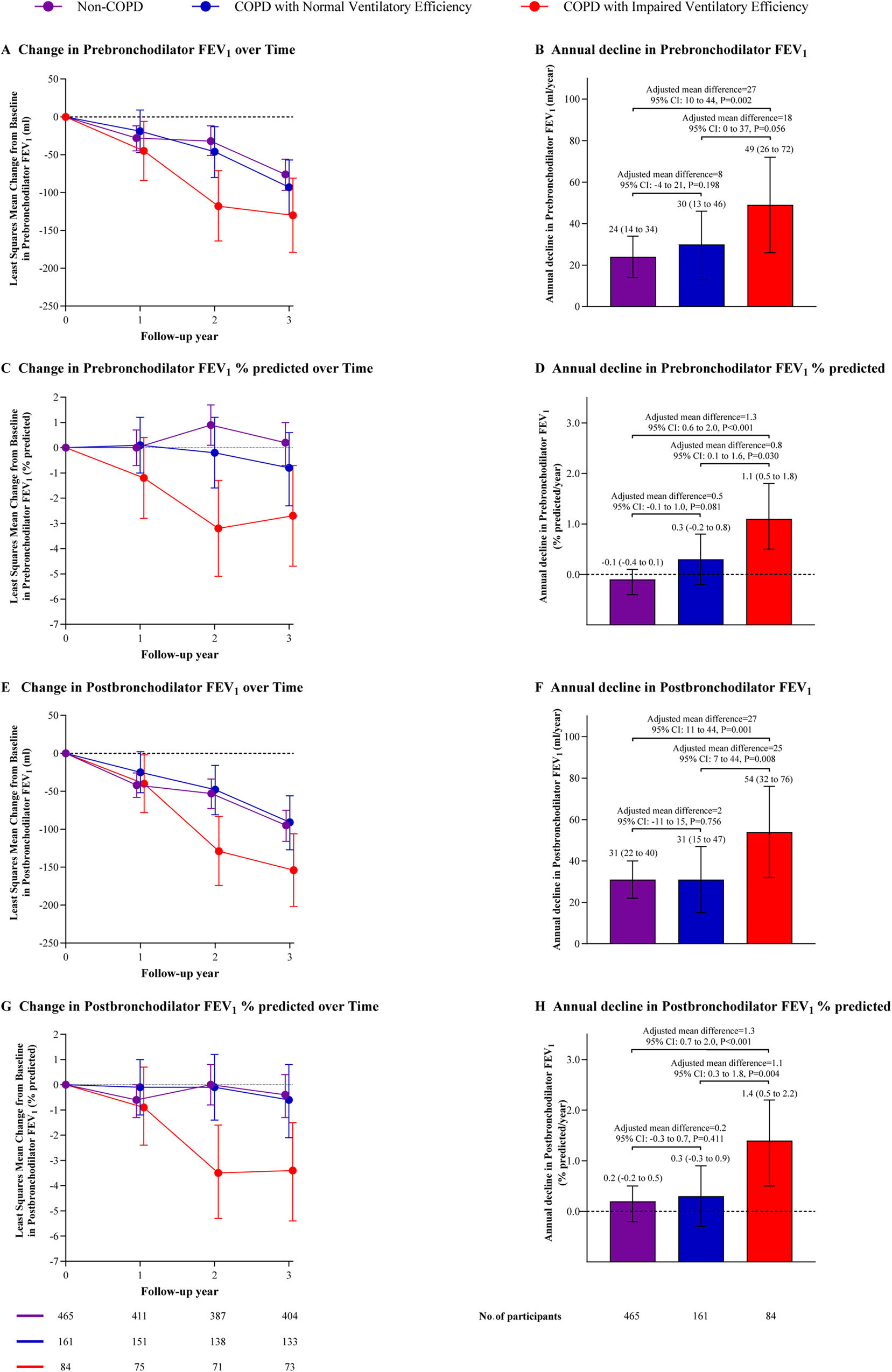
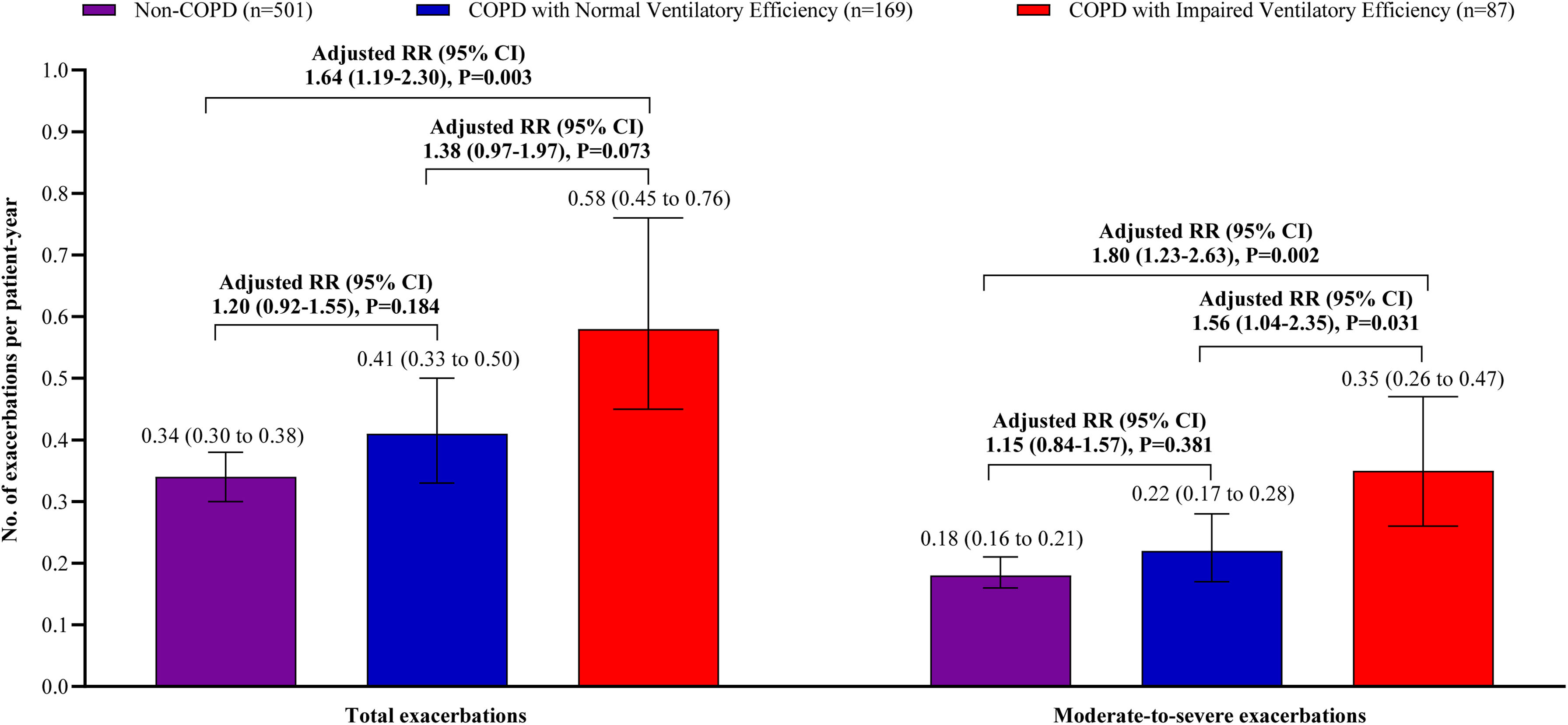
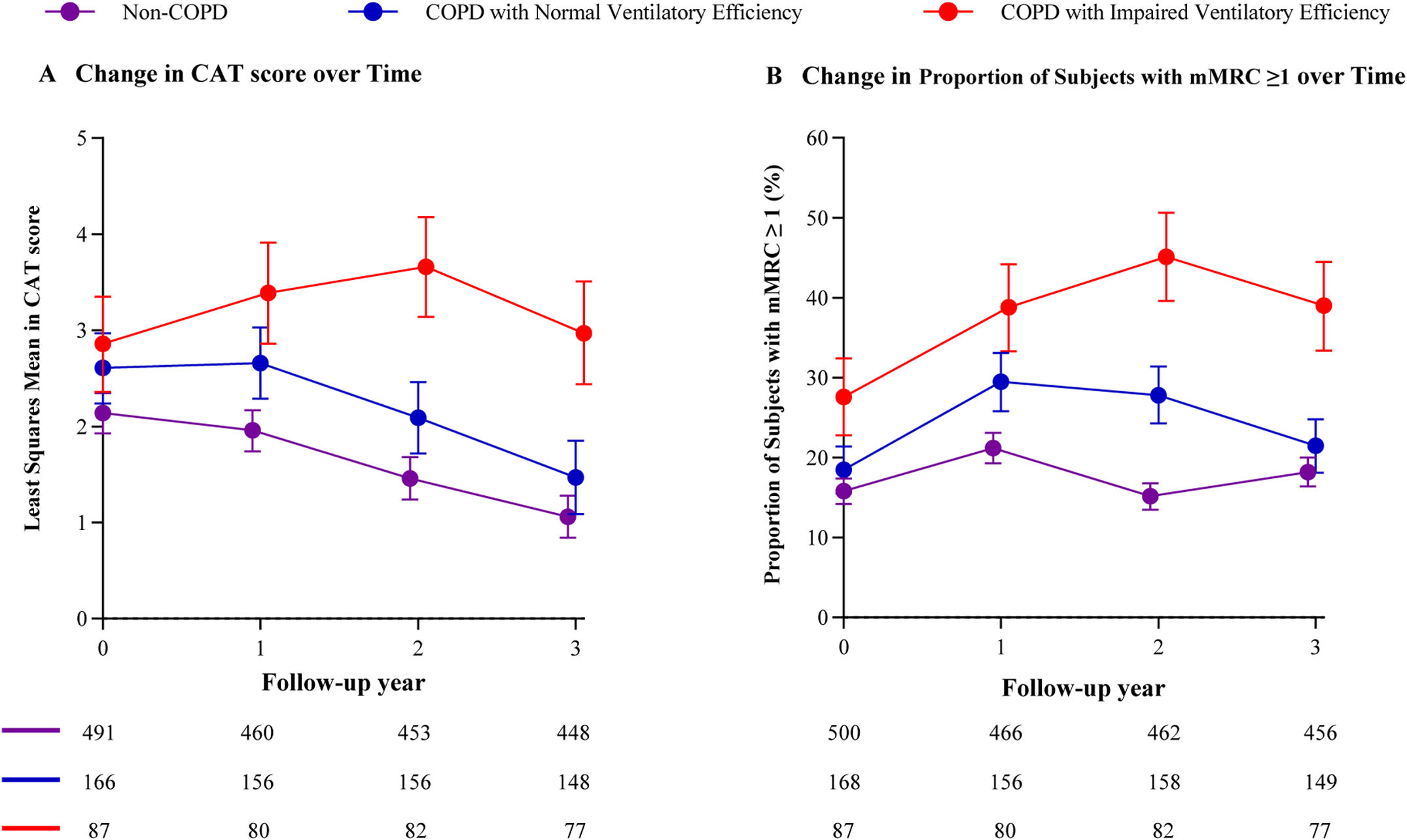
ResultsA total of 780 subjects were included, with 684 (88%) completing follow-up. Patients with impaired ventilatory efficiency displayed a greater annual decline in postbronchodilator FEV1 (54 [95% CI: 32–76]mL/year) than patients with normal ventilatory efficiency (31 [15–47] mL/year, adjusted P=0.008) and non-COPD subjects (31 [22–40]mL/year, adjusted P=0.001). However, no significant difference existed between patients with normal ventilatory efficiency and non-COPD subjects (adjusted P=0.756). Similar results were observed for exacerbation risks and symptom scores.
ConclusionsImpaired ventilatory efficiency can identify high-risk mild-to-moderate COPD patients with poor prognosis independently of established risk factors. Further studies are needed to explore effective interventions for patients with impaired ventilatory efficiency.