The two-view chest radiograph (CR) is one of the most (if not the most) frequently performed radiological examinations in any hospital worldwide.1 Unlike other imaging techniques that also use X-rays (such as mammography or computed tomography [CT]), CRs are not always reported by radiologists (whether thoracic or non-thoracic radiologists). In addition, over the last decades, CT has displaced CRs as the gold standard modality for imaging the lungs and the mediastinum.2,3 This has led many radiologists (mainly young ones) to become less familiar with the details and intricacies of both the posteroanterior projection (PAP) and, particularly, the lateral projection (LP) of CRs.4,5 Although some authors have demonstrated limited value of the LP of CRs in certain scenarios, the lateral view can be particularly useful in assessing the retrosternal and retrocardiac airspaces.6 In recent years, several commercially available artificial intelligence (AI)-based CR (AIBCR) software have been developed that assist radiologists as a decision support tool for the detection of common findings such as airspace disease, pleural effusion, or cardiomegaly (just to name a few).7–10 Many of these AIBCR tools ignore the LP and exclusively assess the PAP; the reasons for this are not entirely clear, but it is possible that (in part) this is due to the fact that these algorithms are not trained by experienced thoracic radiologists familiar with the added value and potential of the LP. By neglecting the LP, these tools are not taking full advantage of all the information provided by a two-view CR.
But how did we get to this situation where such an essential radiological view as the LP (in fact, 50% of the information contained in a 2-view CR) is being ignored by AIBCR tools? Can you ever imagine developing AI applications that would ignore a whole brain hemisphere on a head CT scan in a patient with suspected stroke or disregard one of the 2 projections of a mammogram in a woman undergoing breast cancer screening? Since the classic and detailed anatomical description of CRs more than 45 years ago by Benjamin Felson, Anthony Proto, and John Speckman, the LP has been losing some of its clinical and educational interest.11–13 The reasons are manifold: from the irruption of CT as the gold standard for the assessment of lung diseases to the progressive abandonment of CR reports in many hospitals, through the fact that in multiple clinical scenarios (e.g., emergency departments, intensive care units) only PAPs (or anteroposterior projections) are performed and interpreted (albeit clinically in most cases, without an associated written report). The current wide availability of CT technology means that a questionable finding on posteroanterior (or anteroposterior) projections almost automatically leads to a request for a chest CT scan, without considering whether an additional projection (e.g., LP) can help to better characterize that equivocal finding. We should not forget that chest CT, despite its enormous diagnostic potential, entails an excess of radiation as well as the detection of false-positive findings (which can trigger a spiraling of additional complementary tests).4,5 Young radiologists (and radiology residents) probably no longer feel as comfortable as more senior radiologists assessing the LP; this is demonstrated (in the experience of the two authors of this manuscript who are thoracic radiologists with more than 20 years of experience in academic hospitals) when we observe that medical students and radiology residents only ask doubts on PAPs (and not on LPs) when confronted with two-view CRs. Moreover, since the radiation dose from a LP is substantially higher than that of a PAP (the LP accounts approximately for 75% of the effective radiation dose of a two-view CR), we should ask ourselves whether it is ethical to unnecessarily radiate a patient if an AIBCR model only analyzes “50%” of the information provided by a CR.
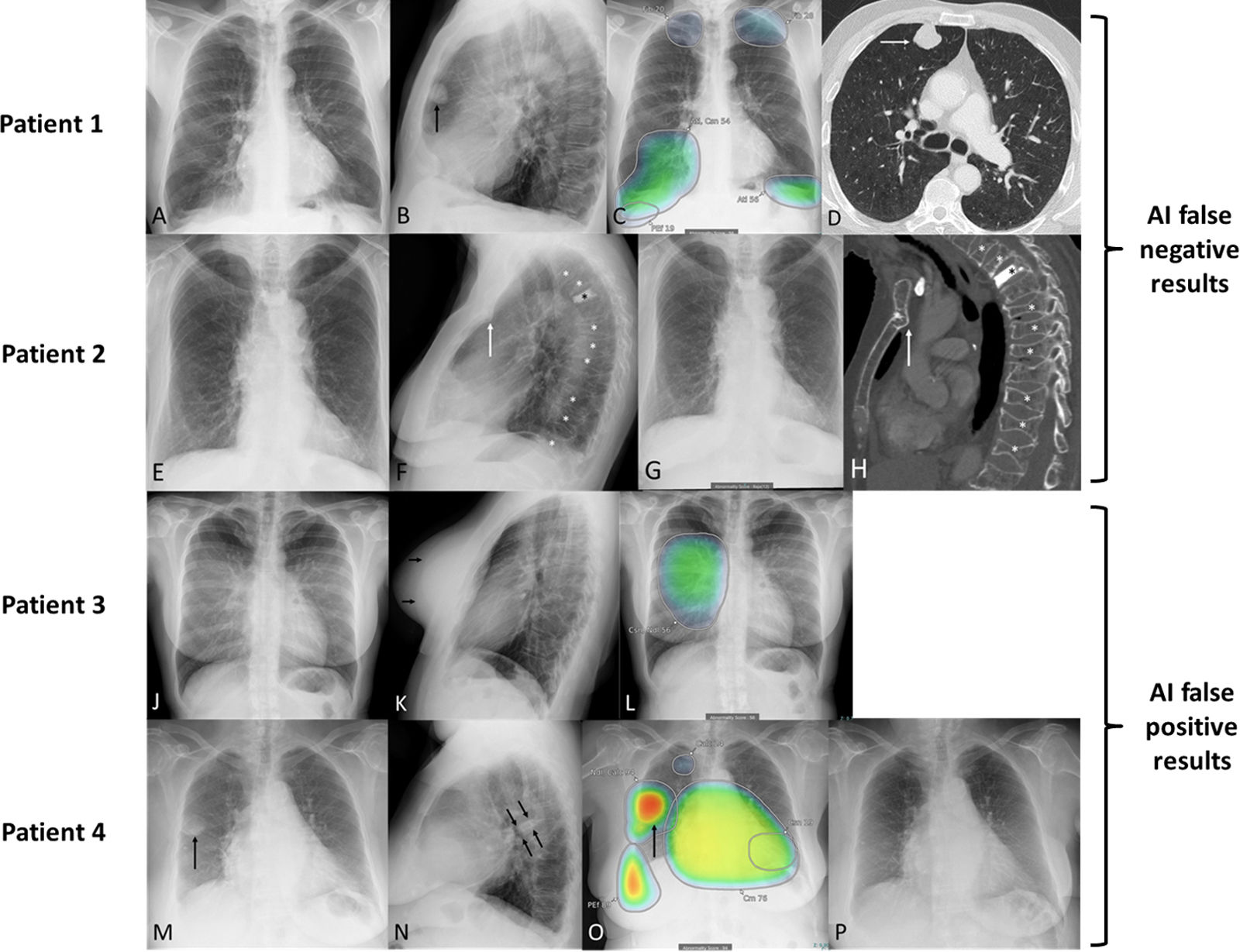
As mentioned above, the LP can be particularly useful in assessing the retrosternal and retrocardiac airspaces as well as the spine, sternum, and the posterior costophrenic angles. For instance, some retrosternal pulmonary nodules and anterior mediastinal lesions may only be visible on LPs; other conditions, such as small pleural effusions or some vertebral and sternal fractures are only detected on the LP (Fig. 1A–H). Finally, and perhaps more importantly, many equivocal findings on the PAP are confirmed or ruled out much more reliably with the LP (Fig. 1J–P). If AIBCR tools do not take into account the data provided by LPs (apart from ethical issues related to “unnecessary” exposure to ionizing radiation), they are likely to generate not only false-negative cases (failure to detect lesions that are only visible on LPs), but also an excess of false-positive cases (equivocal findings on PAPs whose diagnoses can be confirmed or ruled out by LPs).7,14
Examples in which the lack of assessment of the lateral projection (LP) by an artificial intelligence-based chest radiograph (AIBCR) algorithm (Lunit INSIGHT CXR, version 3.1.5.3) may have clinical implications (patients 1 [A–D] and 2 [E–H] are AIBCR false negative examples, whereas patients 3 [J–L] and 4 [M–P] are AIBCR false positive examples). Patient 1 (A–D). (A) A posteroanterior projection (PAP) of a chest radiograph (CR) in an active smoker with shortness of breath shows no abnormal findings. (B) LP of the same patient shows a suspicious retrosternal nodule (arrow). (C) Image caption (heatmap) from an AIBCR algorithm that only assesses the PAP (a deep-learning based algorithm that can detect up to 10 imaging findings) shows several findings with varying degrees of confidence (fibrosis [“Fib”], atelectasis [“Atl”], “consolidation” [“Csn”], “pleural effusion” [“PEf”]) unrelated to the lung nodule (a thoracic radiologist with 20 years of experience didn’t give importance, in the clinical context of the patient, to any of these findings). (D) Axial CT image (lung window) performed 6 days later confirms a suspicious retrosternal lung nodule (arrow) in the right upper lobe. Patient 2 (E–H). (E) A PAP of a CR in an elderly patient with chest pain shows no abnormal acute lung or pleural findings. (F) LP of the same patient shows multiple fractures involving the sternum (arrow) and most of the thoracic vertebrae (white asterisks); note the presence of a vertebroplasty of T4 (black asterisk). (G) Image caption (heatmap) from an AIBCR algorithm that only assesses the PAP does not detect any abnormality. (H) Sagittal CT image (bone window) performed 4 weeks later confirms multiple fractures involving the sternum (arrow) and the majority of thoracic vertebral bodies (white asterisks); note the vertebroplasty of T4 (black asterisk). Patient 3 (J–L). (J) PAP of a CR in a young female patient with cough shows no abnormal findings, except for the presence of breast implants (increased attenuation of the breast shadows). (K) LP of the same patient shows the anterior contour of both breast implants (arrows) but does not demonstrate any pulmonary, mediastinal, pleural or bone abnormalities. (L) Image caption (heatmap) from an AIBCR algorithm that only assesses the PAP suggests a right parahilar “consolidation/nodule” with a 56% confidence (circular area projected over the right lung). Patient 4 (M–P). (M) PAP of a CR in an elderly patient with chronic heart failure and shortness of breath shows a round-like in the right lung (arrow). (N) LP of the same patient demonstrates a fusiform opacity along the right major fissure (arrows), consistent with an interlobar loculated pleural effusion. (O) Image caption (heatmap) from an AIBCR algorithm that only assesses the PAP suggests multiple findings, the most alarming of which (arrow) is a “nodule” with a 94% confidence (red circular area). (P) PAP of a CR of the same patient performed 4 weeks later confirms resolution of the right round-like opacity after treatment for the patient's decompensated heart failure.
We believe that the lack of assessment of LPs by many AIBCR models prevents the correct assessment of the information supplied by “50% of the data provided by two-view CRs”, precludes the diagnosis of some conditions that are only visible (or more conspicuous) on LPs, and decreases the specificity of some findings that may be equivocal on PAPs. We also believe that if AIBCR tools that currently only evaluate the PAP were designed and trained to consider both the PAP view and the LP view, their false positive rate (a recognized drawback of most of these software) would decrease significantly, while allowing the diagnosis of conditions that are more evident on the LP. And last, but not least, developers of AIBCR tools must understand that if a patient is exposed to X-rays for imaging purposes, we physicians should be able (as professionals committed to an ethical and responsible use of ionizing radiation) to extract as much information as possible from every acquired image (in the present topic, from the two projections of two-view CRs). This editorial emphasizes the need for AIBCR algorithms to place patients (the real beneficiaries of AI tools) at the center of the imaging diagnostic process by taking into account the information provided by the LP of CRs.
Declaration of Generative AI and AI-Assisted Technologies in the Writing ProcessNone of the material has been partially or totally produced with the help of any artificial intelligence software or tool.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of InterestThe authors declare not to have any conflicts of interest that may be considered to influence directly or indirectly the content of the manuscript.


![Examples in which the lack of assessment of the lateral projection (LP) by an artificial intelligence-based chest radiograph (AIBCR) algorithm (Lunit INSIGHT CXR, version 3.1.5.3) may have clinical implications (patients 1 [A–D] and 2 [E–H] are AIBCR false negative examples, whereas patients 3 [J–L] and 4 [M–P] are AIBCR false positive examples). Patient 1 (A–D). (A) A posteroanterior projection (PAP) of a chest radiograph (CR) in an active smoker with shortness of breath shows no abnormal findings. (B) LP of the same patient shows a suspicious retrosternal nodule (arrow). (C) Image caption (heatmap) from an AIBCR algorithm that only assesses the PAP (a deep-learning based algorithm that can detect up to 10 imaging findings) shows several findings with varying degrees of confidence (fibrosis [“Fib”], atelectasis [“Atl”], “consolidation” [“Csn”], “pleural effusion” [“PEf”]) unrelated to the lung nodule (a thoracic radiologist with 20 years of experience didn’t give importance, in the clinical context of the patient, to any of these findings). (D) Axial CT image (lung window) performed 6 days later confirms a suspicious retrosternal lung nodule (arrow) in the right upper lobe. Patient 2 (E–H). (E) A PAP of a CR in an elderly patient with chest pain shows no abnormal acute lung or pleural findings. (F) LP of the same patient shows multiple fractures involving the sternum (arrow) and most of the thoracic vertebrae (white asterisks); note the presence of a vertebroplasty of T4 (black asterisk). (G) Image caption (heatmap) from an AIBCR algorithm that only assesses the PAP does not detect any abnormality. (H) Sagittal CT image (bone window) performed 4 weeks later confirms multiple fractures involving the sternum (arrow) and the majority of thoracic vertebral bodies (white asterisks); note the vertebroplasty of T4 (black asterisk). Patient 3 (J–L). (J) PAP of a CR in a young female patient with cough shows no abnormal findings, except for the presence of breast implants (increased attenuation of the breast shadows). (K) LP of the same patient shows the anterior contour of both breast implants (arrows) but does not demonstrate any pulmonary, mediastinal, pleural or bone abnormalities. (L) Image caption (heatmap) from an AIBCR algorithm that only assesses the PAP suggests a right parahilar “consolidation/nodule” with a 56% confidence (circular area projected over the right lung). Patient 4 (M–P). (M) PAP of a CR in an elderly patient with chronic heart failure and shortness of breath shows a round-like in the right lung (arrow). (N) LP of the same patient demonstrates a fusiform opacity along the right major fissure (arrows), consistent with an interlobar loculated pleural effusion. (O) Image caption (heatmap) from an AIBCR algorithm that only assesses the PAP suggests multiple findings, the most alarming of which (arrow) is a “nodule” with a 94% confidence (red circular area). (P) PAP of a CR of the same patient performed 4 weeks later confirms resolution of the right round-like opacity after treatment for the patient Examples in which the lack of assessment of the lateral projection (LP) by an artificial intelligence-based chest radiograph (AIBCR) algorithm (Lunit INSIGHT CXR, version 3.1.5.3) may have clinical implications (patients 1 [A–D] and 2 [E–H] are AIBCR false negative examples, whereas patients 3 [J–L] and 4 [M–P] are AIBCR false positive examples). Patient 1 (A–D). (A) A posteroanterior projection (PAP) of a chest radiograph (CR) in an active smoker with shortness of breath shows no abnormal findings. (B) LP of the same patient shows a suspicious retrosternal nodule (arrow). (C) Image caption (heatmap) from an AIBCR algorithm that only assesses the PAP (a deep-learning based algorithm that can detect up to 10 imaging findings) shows several findings with varying degrees of confidence (fibrosis [“Fib”], atelectasis [“Atl”], “consolidation” [“Csn”], “pleural effusion” [“PEf”]) unrelated to the lung nodule (a thoracic radiologist with 20 years of experience didn’t give importance, in the clinical context of the patient, to any of these findings). (D) Axial CT image (lung window) performed 6 days later confirms a suspicious retrosternal lung nodule (arrow) in the right upper lobe. Patient 2 (E–H). (E) A PAP of a CR in an elderly patient with chest pain shows no abnormal acute lung or pleural findings. (F) LP of the same patient shows multiple fractures involving the sternum (arrow) and most of the thoracic vertebrae (white asterisks); note the presence of a vertebroplasty of T4 (black asterisk). (G) Image caption (heatmap) from an AIBCR algorithm that only assesses the PAP does not detect any abnormality. (H) Sagittal CT image (bone window) performed 4 weeks later confirms multiple fractures involving the sternum (arrow) and the majority of thoracic vertebral bodies (white asterisks); note the vertebroplasty of T4 (black asterisk). Patient 3 (J–L). (J) PAP of a CR in a young female patient with cough shows no abnormal findings, except for the presence of breast implants (increased attenuation of the breast shadows). (K) LP of the same patient shows the anterior contour of both breast implants (arrows) but does not demonstrate any pulmonary, mediastinal, pleural or bone abnormalities. (L) Image caption (heatmap) from an AIBCR algorithm that only assesses the PAP suggests a right parahilar “consolidation/nodule” with a 56% confidence (circular area projected over the right lung). Patient 4 (M–P). (M) PAP of a CR in an elderly patient with chronic heart failure and shortness of breath shows a round-like in the right lung (arrow). (N) LP of the same patient demonstrates a fusiform opacity along the right major fissure (arrows), consistent with an interlobar loculated pleural effusion. (O) Image caption (heatmap) from an AIBCR algorithm that only assesses the PAP suggests multiple findings, the most alarming of which (arrow) is a “nodule” with a 94% confidence (red circular area). (P) PAP of a CR of the same patient performed 4 weeks later confirms resolution of the right round-like opacity after treatment for the patient](https://static.elsevier.es/multimedia/03002896/unassign/S0300289625001802/v1_202505290419/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w98FxLWLw1xoW2PaQDYY7RZU=)







