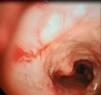
We report the case of a 46-year-old man with no known toxic habits, hospitalized with a diagnosis of pneumonia in the left lower lobe. He had a medical history of recurrent pneumonia during the past 2 years in different sites, with habitual symptoms of cough, expectoration with purulent mucus, and febrile episodes. In the episode reported here, the chest CT scan revealed a pulmonary infiltrate in the left lower lobe and an irregular image of calcified appearance in the tracheal wall and both main bronchi. Fiberoptic bronchoscopy (full procedure shown in the attached video), and endobronchial imaging (Fig. 1) showed nodular involvement of the tracheal cartilage wall and both bronchial trees up to the subsegmentary level, where the bronchial mucosa became normal. Bronchial biopsy of a nodule confirmed the diagnosis of tracheobroncopathia osteochondroplastica.
Tracheobroncopathia osteochondroplastica is a benign disease of the lower region of the trachea and upper region of the main bronchi, with the presence of submucosal calcified cartilaginous nodules protruding into the tracheobronchial lumen.1 No etiology has been defined for this entity, and diagnosis is made with direct vision, and when endobronchial biopsy is performed, description of nodules as above. There is no specific treatment, and resection of the nodules is only required in serious cases, to resolve bronchial obstruction and avoid accumulation of secretions and respiratory infections.1,2
Please cite this article as: Juanola Pla J, et al. Traqueobroncopatía osteocondroplástica. Arch Bronconeumol. 2020;56:172.