The SARS-CoV-2 pandemic has put the Spanish health system to the test, revealing an imbalance between clinical needs and the availability of resources (structures, equipment, and professionals) that has had serious consequences on the outcomes of patients, their families and health professionals themselves. This situation requires complex decision-making based on the classic principles of bioethics,1 distributive justice, patient autonomy, beneficience and non-maleficience, to ensure the appropriate allocation of available resources in a scenario of shortfall. In our view, this distribution of resources must be based on maximizing benefits in the attempt to “save” the greatest number of patients who are more likely to survive.
The document published by the Spanish Society of Intensive Care2 calls for performing triage on admission (a proposal we share) based on giving priority to patients with greater life expectancy (LE), an estimate that is unavoidably probabilistic and difficult to quantify. According to this document, patients older than 80 years of age with comorbidity will preferably receive non-invasive respiratory therapies (NIRTs), and those aged 70–80 years with no significant prior pathology would be candidates for invasive mechanical ventilation (IMV).2
When 2 patients are competing for the same resource, a clinician might decide to base their decision purely on age, as the highest mortality rate occurs in the older age groups (age group 70–79 years = 10.47%, and older than 80 years = 22.31%).3 The older group includes individuals with more comorbidities and fragility; however, we should not make the mistake of considering them, per se, a group with less LE in whom NIRT or IMV would be pointless because of the scant benefit. In clinical practice, making decisions based on the 2 variables of age and comorbidity is not easy, due to the wide variety of comorbidities, many of which are not included in the most commonly used comorbidity indices, and their different impact on the patient’s frailty if they are considered separately.
Joynt et al.4 analyzed reasons for ruling out ICU admission and concluded that age, diagnosis, and disease severity were the main criteria for rejection. While it is true that the mortality of patients >80 years who are admitted to the ICU is high, at around 70% per year, these figures depend, fundamentally, on comorbidity5 and frailty.6–10 These data highlight the need for a more complex assessment based on the Frailty Index (FI) which, in addition to comorbidities, takes into account the patient’s functional status and presence of geriatric syndromes.
In population-based studies, the prevalence of frailty varies between 4.9% and 27.3% and pre-frailty between 34.6% and 50.9%. Prevalence by age group is 7% in >65-year-olds and 20% in >80-year-olds6 and between 23% and 30%8,9 in ICU patients. In these cases, frailty was an age-independent prognostic factor associated with increased mortality during admission and the 6 months after discharge. The studies consulted recommend the use of tools to detect frail patients after admission to the hospital. The FI was the most widely used, as it has a good capacity to distinguish subgroups of patients, and its use could be extrapolated to the Covid-19 pandemic for the selection of frailer patients.
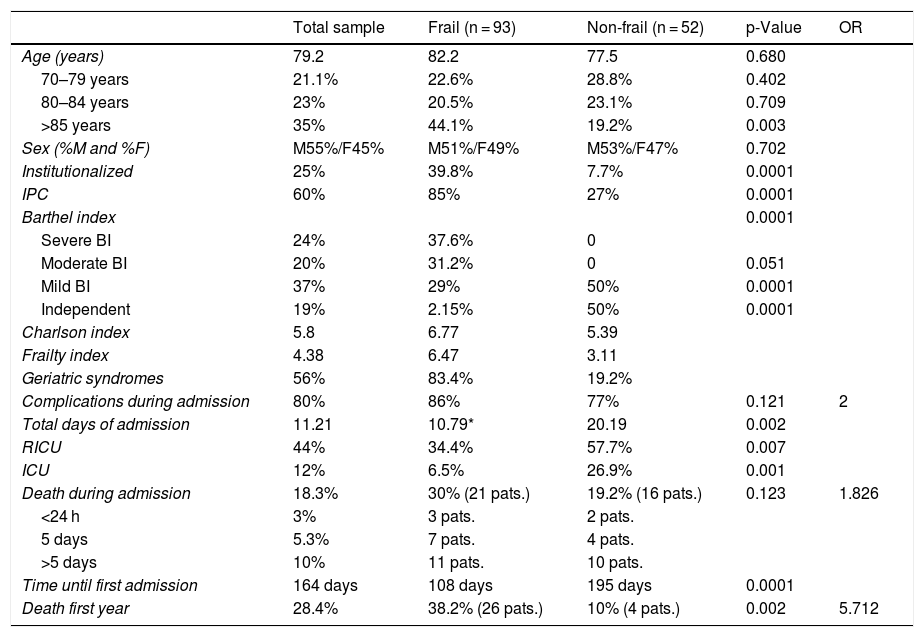
Our group is currently conducting a study that analyzes the impact of frailty on elderly patients admitted for respiratory failure who require non-invasive mechanical ventilation (NIMV): the FRAGRANCIA study (Study on the impact of frailty in older patients requiring NIMV). An intermediate analysis of the results, not yet published, suggests that frailty in the elderly population is associated with higher early mortality (<5 days from admission) and mortality at 1 year of follow-up (26 frail patients vs. 4 patients in the non-frail group, p = 0.002) (Table 1), and that the FI is able to differentiate these risk groups.
Preliminary data from FRAGANCIA study.
| Total sample | Frail (n = 93) | Non-frail (n = 52) | p-Value | OR | |
|---|---|---|---|---|---|
| Age (years) | 79.2 | 82.2 | 77.5 | 0.680 | |
| 70–79 years | 21.1% | 22.6% | 28.8% | 0.402 | |
| 80–84 years | 23% | 20.5% | 23.1% | 0.709 | |
| >85 years | 35% | 44.1% | 19.2% | 0.003 | |
| Sex (%M and %F) | M55%/F45% | M51%/F49% | M53%/F47% | 0.702 | |
| Institutionalized | 25% | 39.8% | 7.7% | 0.0001 | |
| IPC | 60% | 85% | 27% | 0.0001 | |
| Barthel index | 0.0001 | ||||
| Severe BI | 24% | 37.6% | 0 | ||
| Moderate BI | 20% | 31.2% | 0 | 0.051 | |
| Mild BI | 37% | 29% | 50% | 0.0001 | |
| Independent | 19% | 2.15% | 50% | 0.0001 | |
| Charlson index | 5.8 | 6.77 | 5.39 | ||
| Frailty index | 4.38 | 6.47 | 3.11 | ||
| Geriatric syndromes | 56% | 83.4% | 19.2% | ||
| Complications during admission | 80% | 86% | 77% | 0.121 | 2 |
| Total days of admission | 11.21 | 10.79* | 20.19 | 0.002 | |
| RICU | 44% | 34.4% | 57.7% | 0.007 | |
| ICU | 12% | 6.5% | 26.9% | 0.001 | |
| Death during admission | 18.3% | 30% (21 pats.) | 19.2% (16 pats.) | 0.123 | 1.826 |
| <24 h | 3% | 3 pats. | 2 pats. | ||
| 5 days | 5.3% | 7 pats. | 4 pats. | ||
| >5 days | 10% | 11 pats. | 10 pats. | ||
| Time until first admission | 164 days | 108 days | 195 days | 0.0001 | |
| Death first year | 28.4% | 38.2% (26 pats.) | 10% (4 pats.) | 0.002 | 5.712 |
F: female; IB: Barthel index; ICU: intensive care unit; IPC: informal primary caregiver; M: male; pats.: patients; RICU: intermediate respiratory care unit.
We are aware that the FI is not the only answer to the prioritization problems we have experienced during the Covid-19 pandemic, when resources were sometimes unavailable for even the youngest and healthiest of patients. In a recent editorial, published in The New England Journal of Medicine, the authors address the problem of having to choose between 2 or more patients for the assignment of resources, such as ICU admission.11 The need to weigh up multiple ethical values in order to prescribe different interventions and allocate limited resources can generate different benchmarks for the weight assigned to each value in a particular case. This real situation that arose during the Covid-19 pandemic underlines the need to develop fair resource allocation procedures that include all the stakeholders involved in patient care, and the patient and family themselves, in order to develop prioritization criteria for decision-making in times of adversity, without transferring this burden to a single healthcare professional in a specific situation. At the present time, there are no valid criteria to deny ICU admission to people with good life expectancy. The lessons learned from this pandemic underline the need for the health system to increase its resources to adapt to emergency situations.
In adversity, respiratory medicine experts have demonstrated the value of our knowledge of NIRT in critical and semi-critical patients and the importance of the development of respiratory intensive care units (RICU). The RICU plays a role not only in the treatment of the acute patient, but also in the weaning of ICU patients, and helps free up beds. The RICU has eliminated any argument for the need to reserve ICU beds “just in case”. Refusing a patient access to the ICU in order to assign the place to another patient more likely to survive is justifiable in a pandemic,11 but even more so when the initial patient can be transferred to a RICU, where IMV can be withdrawn and replaced by NIRT under a level of monitoring and care that is superior to a conventional hospital ward.
The development of joint care protocols with the collaboration of intensive care units, internal medicine, and emergency departments, together with respiratory medicine, is essential to maximize the management of available resources. Pre-selecting patients with easy, intuitive tools, such as the FI, is indispensable for improving decision-making.
Among the many changes that will emerge after the Covid-19 pandemic, we believe that one of the most relevant will surely be the expansion of RICUs and the leadership of respiratory medicine in decision-making on borderline patients, such as the elderly, unifying selection criteria, clarifying the concept of frailty, and integrating its use into our clinical practice.
Please cite this article as: Segrelles-Calvo G, de Granda-Orive JI, López-Padilla D, Zamora García E. Limitación terapéutica en pacientes ancianos: reflexiones a propósito del COVID-19. Arch Bronconeumol. 2020;56:677–679.