From the moment the COVID-19 pandemic was declared in March 2020, there was palpable fear of the potential impact on the cystic fibrosis (CF) population. Not only were there reports of worse outcomes in more vulnerable persons (e.g., the elderly and those with comorbidities), but CF has a long history of adverse outcomes tied to viruses. Respiratory viral infections are often implicated as a cause of pulmonary exacerbations1,2 and persons with CF (pwCF) had suffered during the 2009 H1N1 Influenza A pandemic.3 Yet the early COVID-19 pandemic experience reported was much better than anticipated. Regional and pooled datasets revealed two important observations: first, remarkably few pwCF were identified with COVID-19 (Fig. 1), perhaps because they were not infected or not identified (e.g., asymptomatic or had mild illness) and second, those who were infected rarely suffered severe outcomes.4–11 Hypotheses arose to account for these better-than-expected outcomes including (1) fewer associated comorbidities (e.g., pwCF are younger and have a lower prevalence of obesity), (2) pwCF are accustomed to infection preventive measures, (3) protective effects of CF cellular processes (e.g., dysregulated autophagy may counteract viral infection), and (4) protective effects of CF therapies (e.g., CFTR modulators or azithromycin).12–15
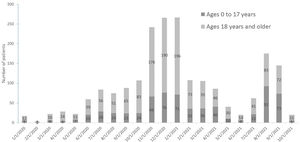
COVID-19 cases among people with CF over time: The chart shows the number of people with CF in the Cystic Fibrosis Patient Registry who tested positive for, or were otherwise diagnosed with, COVID-19 monthly since Jan. 2020. As with the general U.S. population, cases have increased during surges. Note the last bar to the right (10/31/2021) reflects incomplete data.
During times of great apprehension, it is understandable that we express conjecture even with limited supporting data. However, as the COVID-19 pandemic has continued, we have gained additional knowledge about the epidemiology and impact of SARS-CoV-2 in the CF population.16 The general findings of our accumulated data reveal that pwCF are as vulnerable to infection with SARS-CoV-2 as the general population; a surge in cases in pwCF mirrored that of the overall U.S. population (Figure). Also, there are some who are at risk for severe adverse outcomes of COVID-19, especially those who have undergone lung transplantation and on immunosuppressant drugs.17 There do not appear to be any protective benefits from having CF nor from CF therapies. However, those pwCF able to enjoy the benefits of CFTR modulators are in better overall health, and there were fewer children on CFTR modulators were hospitalized.11 There had been a reduction in hospitalizations for CF pulmonary exacerbations associated with the approval of elexacaftor-tezacaftor-ivacaftor (ETI) in the U.S. that preceded the onset of the pandemic with a further reduction in events after its onset18; although this could be attributed to the ETI therapy, there was also a reduction in hospitalizations in children under 12 years of age, who were not eligible for ETI, after the onset of the pandemic. Therefore, it seems most likely that the lower numbers of infected pwCF in the early part of the pandemic were related to better infection control measures and school closures. This is similar to what has been seen in other respiratory conditions, where there was a substantial reduction in COPD exacerbations during 202019 likely because of infection control measures and less exposure to other respiratory viruses.20 The best protection available to us all are preventive measures such as distancing and wearing of masks, and highly-effective COVID vaccines, and so we must strongly encourage our patients and their families to adhere to these measures.
Yet even if not infected with SARS-CoV-2, pwCF were still adversely affected by the pandemic. The economy suffered considerable disruption with furloughs and closures of businesses. The effect on employment affected some pwCF directly because of loss of jobs21 or indirectly due to loss of CF team members.22,23 In addition, there were high rates of concern for food security among pwCF.21
The pandemic has also impacted on how care for pwCF is delivered. When most of the world implemented extreme measures to reduce the spread of infection, this included the closure of medical clinics, and, in some cases, a redeployment of staff to areas in need such as intensive care units. Fortunately, the technology had improved sufficiently to allow for a conversion of CF clinics into a telemedicine model of care. Early experience in CF clinics has demonstrated that multidisciplinary clinics could be conducted in this manner24; clinical encounters have since evolved into hybrid models in which patients may be seen either in person or virtually.25 Clinics implemented typical aspects of CF care remotely (e.g., spirometry and obtaining respiratory cultures26), and found ways to incorporate diabetes management,27 mental health assessment,28,29 physiotherapy including exercise programs,30 and other aspects of CF care. To date, success has been defined by the ability to deliver, to varying degrees, these parts of CF care, and there is expressed desire by pwCF, their families, and the CF multidisciplinary team, in part related to the convenience that telemedicine offers.26
Remote care is expected to remain an important component of CF care31; however, it does not allow for some critical aspects of care (e.g., physical examination and observation of interactions between parent and child with CF) and may adversely compromise the important relationship the multidisciplinary team has with the pwCF and family. It may also result in greater disparities as there are families who do not have the internet access necessary for telehealth.32,33 The hard work must now begin to establish how remote care can best contribute to optimal care for pwCF without losing the clear value of the pre-pandemic care model that has contributed to marked improvement in medical outcomes over the last several decades.34