We describe the early detection of lung cancer during the follow-up of two emphysematous patients undergoing endobronchial treatment with one-way valves for severe dyspnea. In both cases, the lung function improvement achieved after the valves placement allowed their surgical treatment. In additional to standard follow-up for evaluating the progression of emphysema, such patients should be enrolled in a screening program. It may allow the early detection of lung cancer with the possibility for surgery in accordance with respiratory function of patient.
Describimos la detección precoz de cáncer de pulmón durante la revisión de 2 pacientes enfisematosos con tratamiento endobronquial mediante válvulas unidireccionales para la disnea grave. En ambos casos el tratamiento quirúrgico fue posible gracias a la mejora de la actividad pulmonar conseguida tras la colocación de las válvulas. Además del seguimiento convencional para evaluar la evolución del enfisema, dichos pacientes deberían incluirse en un programa de detección sistemática. Podría conseguirse la detección precoz del cáncer de pulmón y, por lo tanto, la posibilidad de operar al paciente en función de su capacidad respiratoria.
We describe the early detection of lung cancer during the follow-up of two emphysematous patients undergoing endobronchial treatment with one-way valves (Zephyr TM; Pulmonx Inc., Redwood, CA, USA) for severe dyspnea. The functional improvement obtained after EBV (endobronchial valve) procedure meant that patients could undergo surgery.
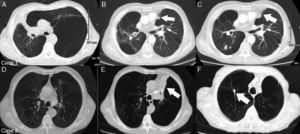
Case 1A 71-year-old male smoker was admitted for giant emphysematous bulla (GEB) that occupied the entire upper left lobe (Fig. 1A). He had had a previous right upper lobectomy for tuberculosis 25 years ago. The patient's respiratory condition was so poor that bullectomy was contraindicated (Table 1). Under moderate sedation, 3 valves were sequentially placed to occlude the left upper lobe communicating with the bulla. One-way flutter EBVs enabled bulla deflation with re-expansion of adjacent compressed lung (Fig. 1B). At 6 months of follow-up, high resolution computed tomography (HRCT) scan revealed a single nodule in the lower right lobe not previously seen (Fig. 1C). This was confirmed as cancer by CT-guided needle biopsy (clinical stage: T1N0M0). Functional improvement obtained after EBV treatment allowed the performance of a wedge resection via muscle-sparing thoracotomy. Thoracoscopy was avoided due to possible post-operative adhesions stemming from the patient's previous lobectomy. After resection, respiratory function was similar to post-EBV values. No other treatments were given. After 10 months of follow-up, the patient was alive without recurrence.
Case 1: A 71-year-old male smoker with giant emphysematous bulla that entirely occupied the left upper lobe (Part A). After endobronchial valve placement in the left bronchus (thin arrow), complete atelectasis of bulla was obtained (thick arrow) with re-expansion of adjacent lung parenchyma (Part B). After 6 months of follow-up, a nodule (*) diagnosed to be a bronchioloalveolar carcinoma was seen in the lower right lobe (Part C). Case 2: A 69-year-old male smoker with emphysema that mostly affected the left upper lobe (Part D). After endobronchial valve placement (thin arrow), complete atelectasis of the treated lobe (thick arrow) was achieved (Part E). After 12 months of follow-up, a solitary pulmonary nodule (thick arrow) diagnosed to be a squamous cell carcinoma was seen in upper right lobe (Part F).
Lung Function of Two Patients.
| Before EBV treatment | At time of cancer detection | After cancer resection | |||||||
|---|---|---|---|---|---|---|---|---|---|
| FEV1 | FVC | RV | FEV1 | FVC | RV | FEV1 | FVC | RV | |
| Case 1 | 0.98 (23) | 1.1 (27) | 4.8 (215) | 1.3 (31) | 1.5 (36) | 3.3 (133) | 1.2 (29) | 1.3 (34) | 3.2 (125) |
| Case 2 | 1.59 (29) | 1.4 (27) | 5.1 (209) | 1.9 (40) | 1.8 (38) | 3.5 (147) | 1.6 (35) | 1.7 (36) | 3.3 (133) |
Data are expressed as liters and (percent of predicted value). FEV1=forced expiratory volume in 1s; FVC=forced vital capacity; R=residual volume.
A 69-year-old male smoker was admitted for severe dyspnea (Table 1) due to emphysema mostly affecting the upper left lobe (Fig. 1D). Two EBVs were sequentially placed in the superior and inferior trunk of the affected lobe. Complete atelectasis of the upper left lobe was achieved with improvement of respiratory function (Fig. 1E). After 12 months of follow-up, an HRCT scan detected a solitary nodular lesion in the upper right lobe (Fig. 1F). Wedge resection was performed via thoracoscopy. Pathological findings revealed a squamous cell carcinoma (pathological stage T1N0M0). No other treatments were given. After 15 months of follow-up, the patient was alive without recurrence.
DiscussionConsidering the growing number of emphysematous patients treated with EBVs,1,2 this paper has two important messages for physicians: (i) emphysematous patients who are candidates for EBV treatment should be included in lung cancer screening programs; and (ii) lung function improvement achieved by EBV placement allows some of them to undergo limited surgical resections (open vs thoracoscopic).
The potential development of lung cancer in emphysematous patients treated with EBV is under-evaluated. In the literature, we found only 1 case where a patient developed cancer in the emphysematous lobe treated with valve placement.3 The diagnosis was obtained with trans-bronchial biopsy after valve removal, and oncological treatment was limited to chemotherapy alone due to the patient's altered lung function. In our cases, however, detection of cancer was easier because it developed in the opposite lung. Moreover, surgery was possible due to improved respiratory function achieved after EBV treatment and maintained at the time of the cancer diagnosis. After surgery, in Case 1, respiratory function was similar to post-EBV values, probably due to the effect of lung volume reduction, as part of the surrounding hyper-expanded non-functional lung was removed with the tumor. In Case 2, the slight decline of respiratory function may be attributable to the wedge resection alone.
Obviously, valve placement does not foster the development of cancer associated with the underlying disease. Several mechanisms have been suggested to explain the strong association between emphysema and lung cancer. Smoking is the main risk factor for both lung cancer and emphysema, and induces a chronic inflammatory state in the lung through generation of reactive oxidant species that lead to emphysema and lung cancer.4 Moreover, emphysema and air-flow obstruction are risk factors for lung cancer independently of smoking, as shown by a study from the Mayo Clinic and 2 lung cancer screening programs. In emphysema, mucociliary clearance is impaired, allowing carcinogens to pool in the airway and leading to the development of lung cancer.5 Thus, the potentially prolonged survival obtained with EBV treatment may allow a patient to live long enough to develop a malignancy.
Finally, lung cancer screening programs may improve early detection of cancer in emphysematous patients undergoing EBV procedure, and cancer therapies, including surgery or non-operative therapy (stereotactic body radiotherapy or chemotherapy) may be offered in accordance with patient's clinical status.
FundingThe authors declare that they did not receive funding for this paper.
Conflict of InterestThe authors declare that they have no conflict of interest.
Please cite this article as: Fiorelli A, Costanzo S, di Costanzo E, Santini M. Detección precoz de cáncer de pulmón durante el seguimiento de pacientes tratados con válvulas endobronquiales unidireccionales para el tratamiento del enfisema. Arch Bronconeumol. 2015;51:e13–e15.