Spontaneous, complete resolution of inflammatory pseudotumour (IPT) of lungs is exceptionally rare. A 44-year-old male was referred for evaluation for «non resolving pneumonitis». He had cough and minimal expectoration for 5 months, chest pain, haemoptysis and fever for a fortnight. Computed tomography of thorax (CT-thorax) confirmed the presence of a homogenous mass with irregular borders in right middle lobe with areas of breakdown and air bronchogram. Transbronchial lung biopsy was suggestive of «plasma cell granuloma». Thoracotomy disclosed a hard mass in right middle lobe adherent to lower lobe, chest wall and mediastinum which could not be removed. A wedge biopsy confirmed IPT. Chest radiograph after 4 weeks revealed significant resolution. CT-thorax a year later showed fibrotic scar. Till date, there are only five reports documenting 6 patients with spontaneous resolution of IPT of lungs and in 4 this occurred within 3 months of an invasive diagnostic intervention.
La resolución completa y espontánea de un seudotumor inflamatorio (STI) de los pulmones es excepcional. Un hombre de 44 años de edad fue derivado para la valoración de una «neumonía no resuelta». Refería tos y expectoración mínima durante 5 meses, al igual que dolor torácico, hemoptisis y fiebre durante 2 semanas. La tomografía computarizada (TC) de tórax confirmó la presencia de una masa homogénea de bordes irregulares localizada en el lóbulo medio derecho con áreas de dispersión y broncograma aéreo. La biopsia pulmonar transbronquial era sugestiva de un «granuloma de células plasmáticas». En la toracotomía se puso de relieve una masa dura localizada en el lóbulo medio derecho y adherida al lóbulo inferior, la pared torácica y el mediastino, cuya resección no fue posible. Una biopsia en cuña confirmó un STI. La radiografía de tórax, efectuada 4 semanas después, reveló una resolución sustancial. En la TC de tórax, realizada un año más tarde, se demostró una escara fibrótica. Hasta la fecha solo se han publicado 6 casos de pacientes con una resolución espontánea de PTI de los pulmones, y en 4 se describió al cabo de 3 meses de una intervención diagnóstica cruenta.
Inflammatory pseudotumor (IPT) of the lungs is a rare entity that, in general, is not part of the list of differential diagnoses for solitary pulmonary masses. Although it may seem to behave as a neoplasm because the lesion may be either extensive, multifocal or recurrent, it is considered a reactive process with an excellent prognosis.1,2 In 1939, Brunn3 described this clinical entity for the first time, and since then sporadic descriptions of clinical cases in published studies1,2,4,5 have characterized the disease.
In 1981, Mandelbaum documented for the first time5 the spontaneous resolution of an IPT, which is an exceptional phenomenon.5 Although in some publications in India there have also been reports of the existence of this disease,6 spontaneous resolution has still not been documented. We present a 44-year-old male with this process who experienced spontaneous resolution after open lung biopsy. The rarity of the said description in the literature encouraged us to submit this present case for publication.
Case ReportThe patient is a 44-year-old male, with negative serology results for human immunodeficiency virus, who was sent to our institute for the evaluation of “unresolved pneumonitis”. Over the course of the previous 5 months, the patient had experienced cough with minimal expectoration, and on occasion the sputum was yellowish. In the 2 weeks prior to being referred to our department, he had experienced fever, hemoptysis and pain in the right lower hemithorax. The fever was associated with anorexia and weight loss. The patient had an accumulated tobacco consumption of 30 pack-years, but at the onset of the illness he had stopped smoking. He had received several oral medications, although could not specify which ones, and had experienced no improvement. Physical examination revealed a middle-age man who was thin but without apparently poor condition. We observed nail clubbing and paleness. Dullness on percussion was detected in the right inframammary and infrascapular regions. Diaphragmatic excursion was reduced on the right side. Vesicular murmur was decreased in the same areas, but with no pathological noises.
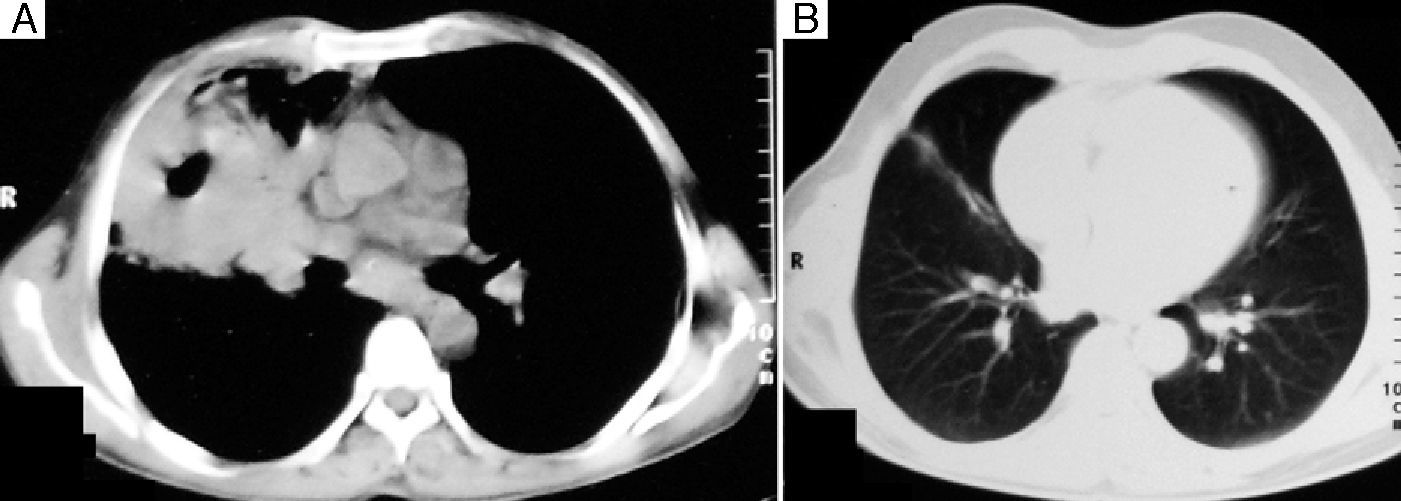
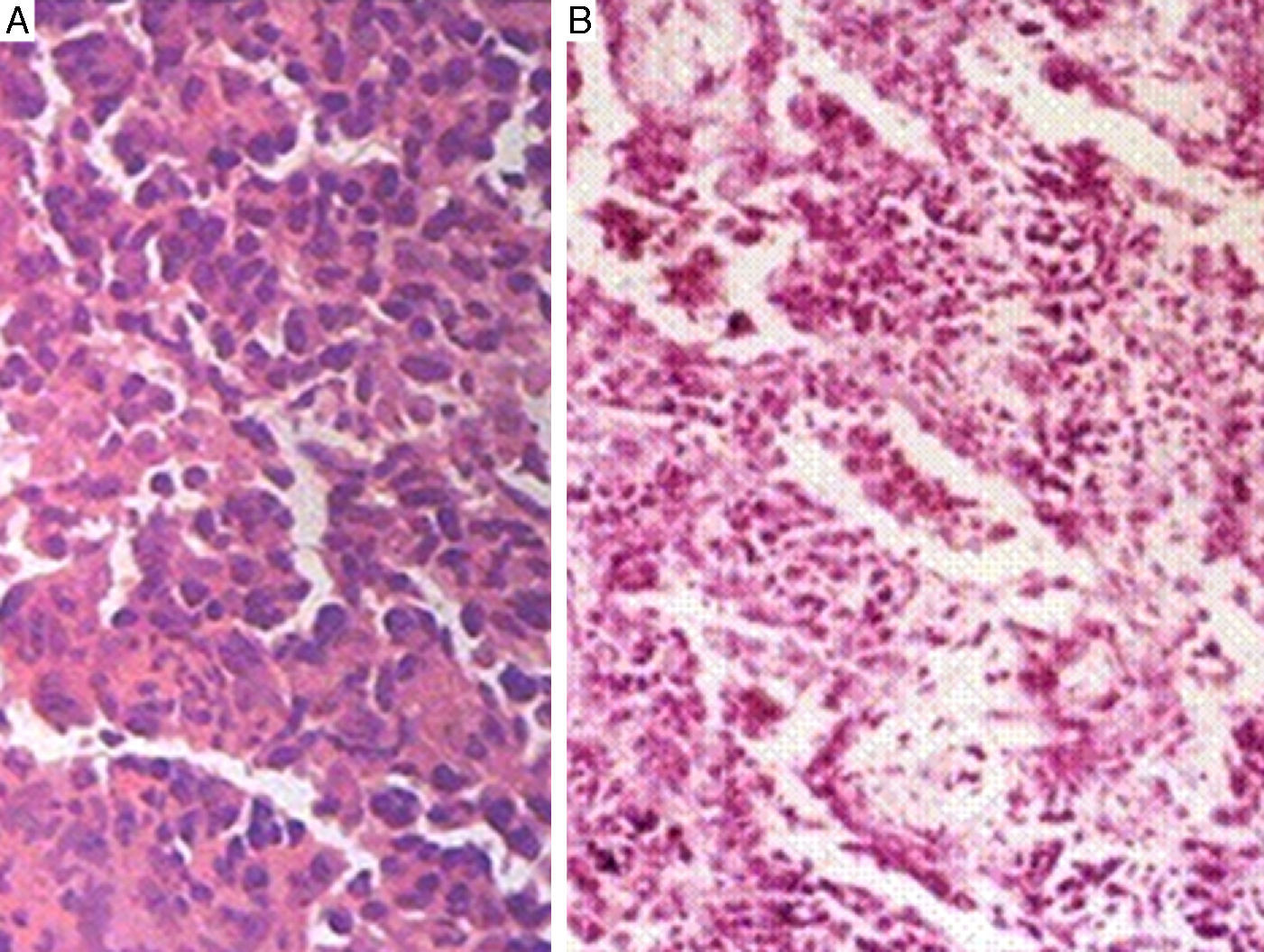
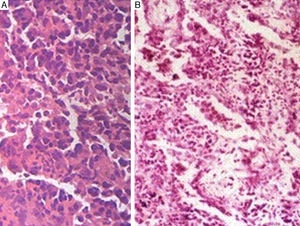
Chest radiography revealed a well-defined homogeneous opacity in the right middle and lower areas, adjacent to the heart. Hemogram demonstrated leukocytosis (13,400cells/mm3) with predominant neutrophilia, as well as microcytic hypochromic anemia. Hepatic and renal function tests were normal. Stains and sputum culture for Mycobacterium tuberculosis and other aerobic microorganisms were negative. Thoracic computed tomography (CT) of the chest demonstrated a solitary homogenous soft-tissue mass with irregular edges located in the right middle lobe, multiple air collections and an air bronchogram indicative of consolidation (Fig. 1A). CT-guided fine-needle aspiration cytology was not conclusive. Fiber optic bronchoscopy demonstrated a well-outlined carina with no endobronchial lesions. The liquid from the bronchoalveolar lavage was negative for M. tuberculosis and other aerobic microorganisms. The histopathologic study of the sample from the transbronchial biopsy demonstrated chronic inflammatory granulation tissue, rich in plasma cells and containing scarce neutrophils. The suspected diagnosis was plasma cell granuloma (Fig. 2A). After bronchoscopy, the patient experienced an increase in fever with purulent sputum and thoracic pain. These symptoms were associated with leukocytosis (19,100cells/mm3) with a predominance of neutrophils, and sputum cultures and stains were negative for aerobic bacteria. Thoracic radiography revealed an increase in size of the opacity with areas of degradation. The patient responded well to the antibiotics administered. Six weeks after bronchoscopy, the patient underwent right posterolateral thoracotomy, which revealed a hard mass in the right middle lobe that was adhered to the lower lobe, thoracic wall and mediastinum. Due to the adherent nature of the mass, a wedge biopsy was taken of the lesion, which demonstrated an accumulation of inflammatory cells with a predominance of lymphoplasmacytic cells. There was no mitotic activity (Fig. 2B). General characteristics confirmed the diagnosis of inflammatory pseudotumor. After thoracotomy, the patient manifested symptomatic and radiological improvement after 3 weeks. One year later, radiography revealed the resolution of the lesion, and chest CT showed a thin residual fibrotic band located in the right middle lobe (Fig. 1B).
Inflammatory pseudotumor of the lung is a rare, locally-aggressive lesion that has an inflammatory composition and favorable prognosis.1,2,7–10 This entity is also known as “inflammatory myofibroblastic tumor”, “histiocytoma”, “plasma cell granuloma” and “xanthofibroma”.1,2,7,10 Umiker and Iverson4 coined the term “post-inflammatory pseudotumor”, which is perhaps the best to describe this entity. The review of recorded institutional cases estimated that the prevalence of pulmonary IPT is 0.7% in lung and bronchial tumors11 and 0.04% in general thoracic surgery procedures.9 Apart from the lungs, IPT has been documented in other body locations.10
IPT of the lung is characterized by variable clinical presentations that range from incidental findings (asymptomatic, revealed by systematic chest radiography) to aggressive presentation, similar to neoplasms.1,2,7–10 Common clinical characteristics include cough, chest pain, dyspnea, hemoptysis, fever, malaise and weight loss.1,2 In children12 and in adults1,2 nail clubbing and hypertrophic osteoarthropathy have been reported. It has been documented that both processes resolve after the surgical excision of IPT.1,12 Although the patient described was a carrier of nail clubbing, this was not inverted after the resolution of the lesion.
From a radiological standpoint, IPT is characterized by its variable presentation. In general, it presents as a solitary nodule or a well-defined lobulated mass,1,8,10 while showing predilection for the lower lobe.8,10 On chest CT, its aspect is non-specific and it is frequently associated with a pattern of heterogeneous attenuation as revealed with contrast.1,2,8,10 Occasionally, it may present with consolidation, atelectasis, bronchiectasis, cavitations or associated lymphadenopathy.1,2,8,10
More rarely, characteristics of local aggressiveness are observed. IPT can become dispersed in the pulmonary artery, left auricle, pleura and mediastinum, which requires major procedures like chest wall resection, pneumonectomy or post-surgery radiotherapy.8,9 Relapse has also been described, which is treated similarly.1,2 In a published series, the overall 5-year survival rate was 91% after resection.9
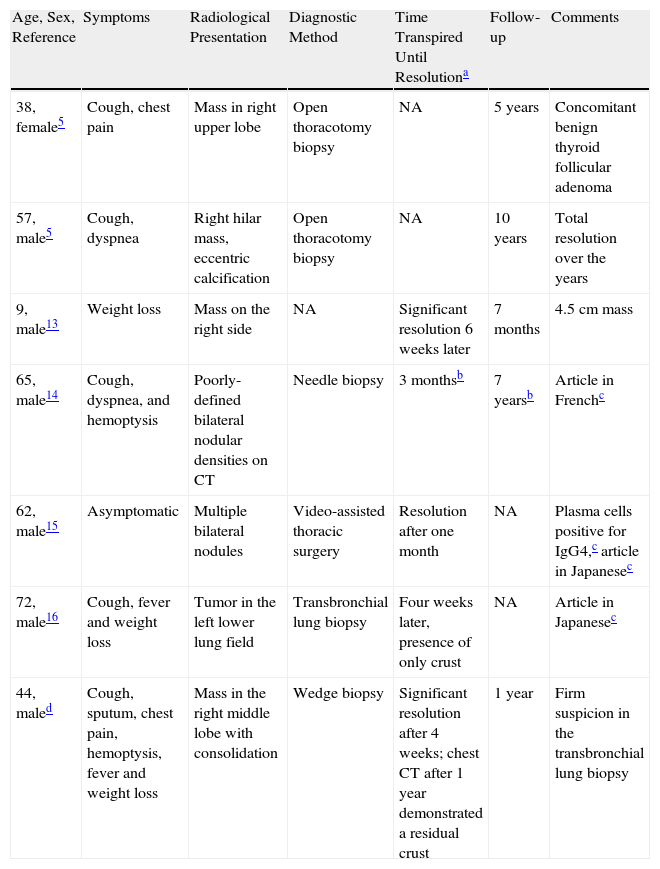
Spontaneous resolution of this entity is an uncommon phenomenon. A search of the published studies in the Medline/PubMed database and other databases with keywords “lung”, “inflammatory pseudotumor” and “spontaneous resolution” produced articles from 1956 to 2011. Afterwards, the references of these articles were located to search for additional pertinent articles. The search turned up five articles5,13–16 that documented six patients with spontaneous, complete resolution of IPT of the lung (Table 1). In addition, there was also a published case of a patient without documented complete resolution.5 Another published case demonstrated growth of the IPT being detained with no intervention and remaining stable for 2 years.17 In another patient, the IPT was completely resolved with corticosteroid treatment.
Summary of the Information Available on the Seven Patients (Including the Patient Described in This Present Article) With Spontaneous Resolution of Inflammatory Pseudotumor.
| Age, Sex, Reference | Symptoms | Radiological Presentation | Diagnostic Method | Time Transpired Until Resolutiona | Follow-up | Comments |
| 38, female5 | Cough, chest pain | Mass in right upper lobe | Open thoracotomy biopsy | NA | 5 years | Concomitant benign thyroid follicular adenoma |
| 57, male5 | Cough, dyspnea | Right hilar mass, eccentric calcification | Open thoracotomy biopsy | NA | 10 years | Total resolution over the years |
| 9, male13 | Weight loss | Mass on the right side | NA | Significant resolution 6 weeks later | 7 months | 4.5cm mass |
| 65, male14 | Cough, dyspnea, and hemoptysis | Poorly-defined bilateral nodular densities on CT | Needle biopsy | 3 monthsb | 7 yearsb | Article in Frenchc |
| 62, male15 | Asymptomatic | Multiple bilateral nodules | Video-assisted thoracic surgery | Resolution after one month | NA | Plasma cells positive for IgG4,c article in Japanesec |
| 72, male16 | Cough, fever and weight loss | Tumor in the left lower lung field | Transbronchial lung biopsy | Four weeks later, presence of only crust | NA | Article in Japanesec |
| 44, maled | Cough, sputum, chest pain, hemoptysis, fever and weight loss | Mass in the right middle lobe with consolidation | Wedge biopsy | Significant resolution after 4 weeks; chest CT after 1 year demonstrated a residual crust | 1 year | Firm suspicion in the transbronchial lung biopsy |
NA: (information) not available.
Table 1 summarizes the five publications that document six patients with spontaneous resolution. Out of the six patients, five were males.5,13–16 There were five adults,5,14–16 three of whom were over the age of 60,14–16 and one was a child.13 Cough was present in four5,14,16 out of five patients, while one remained asymptomatic.15 From a radiological standpoint, four patients5,13,16 presented solitary masses, one of which5 was also associated with an eccentric calcification, while two14,15 presented bilateral nodules. The diagnosis was established with thoracotomy5/video-assisted thoracoscopic surgery15 in three patients, while in one patient needle biopsy was fundamental14 and in another transbronchial lung biopsy was used.16 After the diagnostic intervention, in three13,15,16 of the six patients (for whom information was available), at the end of a period of 4 weeks to 3 months there was an observed resolution of the symptoms together with substantial radiological resolution. The course of the follow-up (7 months to 10 years in three patients5,13) transpired without incident.
The patient described experienced spectacular asymptomatic improvement in the third week and chest radiography, done after 4 weeks, demonstrated a notable resolution of the lesion. Follow-up CT one year later revealed complete resolution.
The reasons for the spontaneous resolution of this lesion are unknown. However, in four out of seven patients, including the patient of this case report, IPT was spontaneously resolved weeks after an invasive, bloody diagnostic procedure. The case described emphasizes the fact that the spontaneous resolution of this entity could possibly be triggered by the invasive nature of the diagnostic procedure and, consequently, it is prudent to observe patients who may potentially present this phenomenon before planning the surgical resection of the lesion.
The authors would like to express their thanks to Dr. Antoine Chucrallah for sending us details of the case report published in France.14
Please cite this article as: Maurya V, et al. Resolución espontánea de un seudotumor inflamatorio del pulmón como consecuencia de una biopsia en cuña. Arch Bronconeumol. 2012;49:31–4.