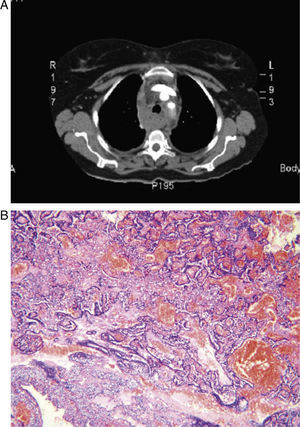
We would like to describe the case of a 61-year-old woman who was seen in our consultation due to atraumatic mediastinal hematoma. In addition, she reported having had a snakebite on her right arm 5 days earlier, which had caused a local reaction. Imaging studies ruled out vascular or cardiac lesions. On exploration thoracotomy, we observed a large mediastinal hematoma that infiltrated the mediastinal tissue, while no tumors or bleeding vessels were identified (Fig. 1A). There was no injury to the superior vena cava. The pericardium was opened and the root of the aorta and the pulmonary artery were explored, and no lesion or bleeding was found. Multiple clots as well as fatty tissue infiltrated with blood were extracted. With the material sent to the Pathology Department, the diagnosis was determined to be rupture of an ectopic parathyroid gland cystadenoma. The macroscopic study showed evidence of tissue that was extensively infiltrated with hemorrhage. The microscopic study revealed a proliferation of polygonal cells, without atypia, with clear cytoplasm, arranged in solid nests and surrounded by a densely vascularized stroma, with widespread hemorrhage (Fig. 1B). Said cells were positive for CK7, AE1/AE3, SYN, and RCC. Mediastinal hematomas are caused by trauma, aneurisms or the rupture of large vessels or the heart and iatrogenesis associated with invasive or surgical procedures.1 Among other possible etiologies are: coagulation alterations, tumors (benign and malignant), cough or sneezing (Valsalva maneuver), uremia, renovascular hypertension, thymic rupture, thyroid and parathyroid cysts, metastasis, extramedullary hematopoiesis, and mediastinal lipomatosis.1 If the cause of the hematoma has not been able to be identified clinically, then diagnostic methods should be used. The gold-standard methods are aortography and surgical exploration. Kodolitsch et al. demonstrated that the combination of the studies had a better yield than each one used separately. Transthoracic echocardiogram and computed tomography had a sensitivity of 75% and a specificity of 99%, and transesophageal echocardiogram and nuclear magnetic resonance (NMR) had a sensitivity of 92% and a specificity of 97%. There are still no specific data that endorse the use of the PET-scan for diagnosis.2 The treatment of these patients varies according to their state and the results of the complementary methods. If the patient is stable and there are certain suspicions for the etiology due to the results of the studies, the approach may be conservative. Another alternative is percutaneous embolization. If the patient is unstable and the cause has not been found, the treatment is surgical exploration (thoracotomy or sternotomy).1,2 As for histopathologic findings, in a study published in 1995, 97 patients were studied with diagnosis of renal hyperparathyroidism, detecting 60 ectopic glands in 34 patients. In this study, the most frequent ectopic location was mediastinal.3 In another study with 231 patients who underwent surgery due to hyperparathyroidism, 16% had gland ectopia. Ectopic inferior parathyroid glands were 62% of the total, finding 22% in the anterosuperior mediastinum. Ectopic superior parathyroids, corresponding to 38%, were observed in the posterior superior mediastinum in 14%.4 Ectopic parathyroid tissue can undergo hyperplastic and adenomatous processes. In 1992, Nies reported that out of 126 patients with parathyroid adenomas, 6 patients (4.8%) had 7 cystadenomas. Out of these, a significant number were found in the mediastinum, giving rise to the possibility that cystic parathyroid adenomas may have the tendency to be located outside of their usual anatomical location.5 Given the hemorrhage and fragmentation of the tissue, the macroscopic study of the resected material was not able to identify a tumor lesion, much less make an approximation of the size or weight of the lesion. Under the microscope, the tumor cells presented the typical morphology and architecture of parathyroid tissue. Immunohistochemistry was able to confirm the origin by showing immunomarking for CK7, AE1/AE3 and SYN. The expression of the RCC marker determined the adenomatous nature of the lesion, as a study by McGregor et al. showed evidence that 100% of parathyroid adenomas studied were positive for RCC.6 The lesion also presented extensive hemorrhage with marked vasocongestion, linked to the origin of the mediastinal hematoma.
Atraumatic spontaneous mediastinal hematomas are infrequent. In the absence of the most common etiologies, the possibility for rupture of ectopic cystic lesions should be contemplated. This underlines the importance of understanding ectopic parathyroid lesions and knowing their most frequent locations due to the possibility of atypical manifestations that can involve various differential diagnoses with different therapeutic approaches. Complementary studies can facilitate the etiologic diagnosis and aid in the choice of the best method of treatment. Histopathologic studies and immunohistochemistry are useful for determining the cause of the hemorrhage, in this case determining the parathyroid origin of the lesion and ruling out other neoplasms.
Please cite this article as: Bürgesser MV, et al. Hematoma mediastinal espontáneo como manifestación inicial de adenoma quístico de paratiroides ectópica. Arch Bronconeumol. 2012; 48: 185-6.