Latin America is made up of a number of developing countries. Demographic changes are occurring in close to 600 million inhabitants, in whom a significant growth in population is combined with the progressive ageing of the population. This part of the world poses great challenges for general and respiratory health. Most of the countries have significant, or even greater, rates of chronic respiratory diseases or exposure to risk. Human resources in healthcare are not readily available, particularly in the area of respiratory disease specialists. Academic training centres are few and even non-existent in the majority of the countries.
The detailed analysis of these conditions provides a basis for reflection on the main challenges and proposals for the management and training of better human resources in this specialist area.
América Latina está compuesta por países en vías de desarrollo. Los cerca de 600 millones de habitantes exhiben una transición demográfica que combina un crecimiento significativo de la población con un fenómeno de envejecimiento poblacional progresivo. Esta región del mundo exhibe grandes retos para la salud general y la respiratoria. La mayoría de los países muestran tasas significativas, incluso mayor, de enfermedades respiratorias crónicas o de exposiciones de riesgo. La disponibilidad de recursos humanos para la salud es escasa, particularmente en cuanto a especialistas en enfermedades respiratorias se refiere. Los centros de formación académica son pocos e incluso inexistentes en la mayor parte de los países.
El análisis detallado de estas condiciones permitirá reflexionar sobre los principales retos, así como sobre las propuestas para la gestión y la formación de más y mejores recursos humanos en la especialidad.
In 2011, the United Nations Organisation (UNO) estimated that the population of Latin America was 602.3 million inhabitants. It is a population that has practically quadrupled since 1950, and the estimate is that by 2050 it will reach 807 million inhabitants, after which it will slowly begin to decline. The region represents around 8% of the world population, similar to that of Europe, and this proportion will be maintained throughout the century due to the continued exponential rise in population in Asia and Africa.1
Latin America is made up of developing countries which are undergoing a process of demographic change characterised by a significant decrease in mortality rates and increase in life expectancy, accompanied by ever increasing birth rates. In addition, the population will rapidly become older in decades to come: it is estimated that by 2050, 79% of the world population over the age of 60 will be from developing countries.2
Latin American countries share not only the language and many cultural aspects, but they also share socioeconomic and political variables. Interaction between professional training and medical cover by specialists in the respiratory field in the region has not been clearly determined. Budget limitations are generally a common factor and policies for training in healthcare resources are often poorly planned and analysed.
This review is a detailed analysis of the respiratory health and epidemiological situation of respiratory diseases in Latin America, and how the population is covered in terms of respiratory specialists, and the status of medical resident training in the region.
Respiratory HealthAmong the 10 major causes of mortality reported by the World Health Organisation (WHO) are upper respiratory infections, chronic obstructive pulmonary disease (COPD), tuberculosis (TB) and lung cancer.3,4 Morbidity and mortality rates for COPD and lung cancer are growing and when all these conditions are pooled, the mortality rate is significantly greater than the next main cause of death worldwide: ischaemic heart disease (16.7% vs 12.8%). It could be argued that the main cause of death worldwide is lung disease.3,4 Other factors impacting significantly on respiratory health are tobacco use and exposure to contaminants in the workplace, at home and in the environment.
The WHO estimates that about 3.9 million deaths a year are due to acute respiratory infections. Seasonal influenza alone can produce around 600 million cases worldwide, of which 3 million will be severe, with an estimated mortality of 250000–500000 cases.5–7 Pneumonia is the main cause of death in children under the age of 5 and is responsible for 1.4 million deaths a year.8
Although COPD is currently the fourth cause of death worldwide, it is thought that by 2020 it will be the third.9 The overall prevalence of this disease has been estimated as 10% in the population over 40 years of age.10 Data on the prevalence of COPD in Latin America are derived principally from 2 epidemiological studies: PLATINO (Proyecto Latinoamericano de Investigación en Obstrucción Pulmonar – Latin American Lung Obstruction Research Project) and PREPOCOL.11,12
The first is an epidemiological study carried out in 5 Latin American cities: Mexico City (México), São Paulo (Brazil), Montevideo (Uruguay), Santiago de Chile (Chile) and Caracas (Venezuela).11 According to this study, the overall prevalence of the disease, using the post-bronchodilator FEV1/FVC ratio<0.70 as a diagnostic criterion, was 14.3% (ranging from 7.8% in Mexico City to 19.7% in Montevideo), while if the lower limit of normal of the FEV1/FVC ratio is used, prevalence was 11.7%.13 Other findings from PLATINO describe that the subdiagnosis of COPD reaches 89%, while 64% of the individuals with a prior diagnosis of COPD did not have airways obstruction (diagnostic error), principally attributed to the poor use of spirometry.14 PREPOCOL investigated the prevalence of COPD in 5 Columbian cities.12 This study reported an overall prevalence of COPD in Colombia of 8.9%, ranging between 6.2% in Barranquilla and 13.5% in Medellín.
TB continues to be a significant threat to public health in Latin America.15 According to the WHO, the Americas make up 6% of the worldwide TB burden.16 The majority of Latin American countries have intermediate TB rates (26–100 cases/100000).16 In 2004, around 220000 of the estimated 350000 cases were reported in Latin America and the Caribbean, with an incidence rate of 39.6/100000 inhabitants16; over 80% of the cases came from 17 countries in Latin America, primarily Brazil and Peru.17 Human immunodeficiency virus (HIV) infection, Mycobacterium tuberculosis resistance to antituberculosis drugs, the increasing poverty gap and the existence of inadequate sanitary systems have exacerbated the TB problem. In 2009, 36000 new cases of TB with HIV were estimated in the Americas, representing 13% of all new cases. The TB seropositivity rate was 3.9/100000 inhabitants.18 Over half of all new HIV cases occurred in Brazil.
Lung cancer is the most common neoplastic disease in the world and the greatest cause of death from cancer, particularly in men.19,20 Although the incidence in Europe, North America and Asia is greater (39–57/100000 in men), Latin America has intermediate rates (12.4–20.4/100000). Statistics from the year 2000 on lung cancer mortality show that the rates in men were lower in most of the Latin American countries (13–21/100000) than in North America (rates of 40/100000). The highest rates for men were recorded in Argentina and Cuba (35.0 and 38.3/100000, respectively), while the lowest rate was seen in Ecuador (7.7/100000).
Other public respiratory health problems that do not produce high mortality rates but can cause significant morbidity and generate high costs and demand on specialist services include asthma and obstructive sleep apnoea hypopnoea syndrome (OSAHS). The prevalence of asthma in children in 8 Latin American countries who participated in phase III of the ISAAC study ranged between 8.6% in Mexico (lowest value) and 32.1% in Costa Rica (highest value).21 The vast majority of Latin American patients with asthma receive unacceptably poor care in terms of diagnosis and monitoring, resulting in a significant rate of morbidity.22 There is little information on the prevalence of asthma in adults in Latin America. PLATINO study data indicate that 12.9% of the population aged >40 years reported a previous medical diagnosis of asthma (self-reported asthma).23
Clinical and epidemiological aspects of OSAHS in the Hispanic and Latin population were recently reviewed in detail.24,25 The reported prevalence of OSAHS in Latin America is similar to that of other Western countries, but the situation in Latin American countries is less favourable, due to a process of acculturation, and with rapid growth in obesity rates accompanied by a scarcity of sleep medicine resources and the need for the creation of a specific infrastructure and training of specialised human resources. An estimation of the prevalence of OSAHS was made in the PLATINO study on the basis of habitual snoring, apnoeas experienced and excessive daytime somnolence.26 Prevalence in women and men was 2.4% vs 1.5% in Caracas, 0.5% vs 3.7% in Montevideo, 2.4% vs 4.4% in Mexico and 5.0% vs 8.8% in Santiago, respectively. Recently, Tufik et al.27 reported on the prevalence of OSAHS in a sample of 1042 volunteers representative of the overall population aged between 20 and 80 years residing in the city of São Paulo, Brazil. All participants underwent full polysomnography in the laboratory, using current diagnostic criteria. The overall prevalence of OSAHS was 16.9%, on the basis of an apnoea–hypopnoea index of 15 or more episodes per hour of sleep. This study also describes a growing incidence in subjects between the ages of 30 and 80, 0%–36% in women and 4%–85% in men.27
Tobacco use and exposure to contaminants also deserve analysis. The Panamerican Health Organisation (PHO) has reported a smoking rate in the majority of the region's countries of between 15% and 40%, although prevalence in adolescents (13–15 years) tends to be greater.28 Active smoking habits in subjects over 40 years of age were reported in the PLATINO study: between 16.6% and 35.9% in women and 30.2% and 42.6% in men.29 Using a retrospective cohort analysis, the study found that the greatest prevalence of tobacco use is between the ages of 20 and 29 years, while the highest incidence is between 10 and 19 years of age.29 However, WHO Framework Agreement on Tobacco Control was only signed recently by Latin American countries (2004).
Between 30% and 75% of homes in Latin America use solid fuels, almost always in poorly ventilated kitchens.30,31 Under these conditions, biomass combustion creates excessive levels of indoor contaminants.32 According to the estimates, half of COPD deaths in Latin America are caused by biomass contamination, 75% of which are in women.33
Occupational lung diseases originate from airborne contaminants in the working environment. These diseases contribute significantly to the health burden of the general population, and particularly to the economically active subgroup. Working environment agents are the etiological origin of between 1% and 40% of lung cancers, 10% and 20% of asthma and approximately 15% of COPD.34,35
Number of PulmonologistsThere is very little information available on the number of respiratory disease specialists in Latin America. To estimate how many specialists there are in each region, information was gathered with a direct survey on the number of respiratory specialists and the status of medical resident training in 19 countries, including 2 Caribbean countries (Cuba and Dominican Republic). The survey included a total of 17 questions on the population, the number of pulmonologists attending adults, the number attending children and the number of chest surgeons, and the information on professional societies, respiratory medicine resident training programmes, associated specialties and funding of medical residents.
Most of the countries interviewed had only one professional society, which usually included pulmonologists attending adults, pulmonologists attending children and chest surgeons. The survey was sent to renowned regional specialists, the majority of who were active chairmen, ex-chairmen or professionals directly related to the society in each country (see Appendix 1, Sources of information). In a few cases, almost always in countries with the smallest populations, the survey was addressed to specialists known to the authors. The total estimated population for each country was obtained from World Bank data from the year 2011.36
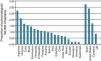
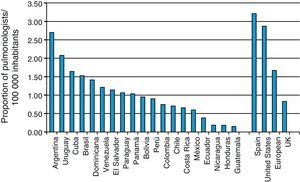
Table 1 is a list of the countries surveyed, their total population, the total number of specialists (pulmonologists attending adults, pulmonologists attending children and chest surgeons) and the number of pulmonologists per 100000 inhabitants, as an indicator of how the population was covered by specialists. The total population of the 19 countries included in the surveys was 571538587 inhabitants, with a total number of 6706 pulmonologists attending adults, corresponding to a rate of 1.20 pulmonologists per 100000 inhabitants. A total of 686 paediatric pulmonologists and 292 chest surgeons were recorded. The best cover by specialists was found in Argentina, with a rate of 2.70 and the lowest in Guatemala, with 0.15 (Fig. 1). Only 2 countries (10.5%) had a rate higher than 2 (Argentina and Uruguay); five countries (31.6%) had a rate of 1–1.9 and in 10 countries (52.6%), the rate was lower than 1 (Table 1).
Population in Latin America and Distribution by Number of Pulmonologists.
| Country | Population (millions) | Total number | Pulmonologists attending adults/10000 | ||
| Pulmonologists attending adults | Paediatric pulmonologists | Chest surgeons | |||
| Argentina | 40764561 | 1100 | 250 | 170 | 2.70 |
| Brazil | 196655014 | 3000 | 550 | 1.53 | |
| Bolivia | 10088108 | 89 | 4 | 3 | 0.95 |
| Chile | 17269525 | 122 | 150 | 30 | 0.71 |
| Colombia | 46927125 | 350 | 75 | 0.75 | |
| Costa Rica | 4726575 | 31 | 8 | 14 | 0.66 |
| Cuba | 11253665 | 185 | 1.64 | ||
| Dominican Republic | 10056181 | 142 | 35 | 6 | 1.41 |
| Ecuador | 14666055 | 100 | 5 | 8 | 0.38 |
| El Salvador | 6227491 | 75 | 1.20 | ||
| Guatemala | 14757316 | 22 | 18 | 6 | 0.15 |
| Honduras | 7754687 | 14 | 8 | 3 | 0.18 |
| Panama | 3571185 | 37 | 8 | 3 | 1.04 |
| Paraguay | 6568290 | 70 | 3 | 4 | 1.07 |
| Peru | 29399817 | 265 | 38 | 0.90 | |
| Mexico | 112336538 | 670 | 125 | 80 | 0.60 |
| Nicaragua | 5869859 | 11 | 20 | 2 | 0.19 |
| Uruguay | 3368595 | 70 | 6 | 12 | 2.08 |
| Venezuela | 29278000 | 353 | 120 | 60 | 1.21 |
| Total | 571538587 | 6706 | 686 | 292 | 1.20 |
Recommendations made several decades ago suggested that at least 1 specialist was required per 50000 inhabitants, i.e., a rate of 2/100000. Other studies refer to WHO recommendations of up to 3.5–4 pulmonologists/100000,36 but this figure was not reached in any of the countries surveyed. According to these recommendations, the deficit of specialists would exceed the current figure by 2- to 3-fold. However, even among Latin American countries, the differences are very wide (rates ranging from 0.15 to 2.70).
The optimal number of specialists for a country or a population cannot be defined homogeneously due to the wide differences between demographics and healthcare systems. In addition to the size of the population, the main factors influencing the number of specialists required are: population growth and ageing; activities carried out by each specialist (clinics, teaching, research, administration); the distribution of the healthcare system (private and public); working hours and multi-employment (very common in Latin America); feminization of medicine; and the rate of ageing and retirement among specialists.37,38
In Spain (Fig. 1) with a healthcare system with universal coverage, in 2002 there was an average rate of 3.21 pulmonologists/100000, with a distribution of 1.62–6.66/100000 over all the provinces,37 which was generally greater than the European mean of 1.67 reported in 1998.39 However, the authors of the study conclude that respiratory specialisation in Spain was not fully covered and there is a significant deficit in many provinces. In the United States, the Committee on Manpower for Pulmonary and Critical Care Societies (COMPACCS)40 investigated the medical services provided by pulmonologists throughout the country. In the year 2000, there were a total of 8080 pulmonologists (2.87/100000) in the US, most of whom were also critical care specialists, working an average of 68h a week, dedicating 78% of their time to clinical activities. This study estimated that the growth and process of ageing in the population would mean that the services provided by these specialists would fall by 22% by 2020, and by 35% in 2030, unless better human resources were made available.
The estimation made by this study regarding the number of specialists has its limitations. The first is that it only takes in account those physicians registered in the professional societies of each country, which could lead to an underestimation in the total number, which in some cases was approximate. Some societies recognised that up to 30% of specialists are not active members; moreover, the younger, recently qualified pulmonologists, may take some years to become active members. The second limitation is that the rate of pulmonologists given in this report is not an exact measurement of the specialist cover in each country. A relevant factor is the distribution in the provinces compared to cities, as services tend to be concentrated in the large cities and in the best tertiary reference centres. In Spain, the rate of pulmonologists varies more than 4-fold among the provinces.37 In Mexico, in 2010, almost half of the pulmonologists were found to live in the metropolitan area of Mexico City, while 72 cities or communities with populations ranging from 100000 to 400000 did not have any specialists at all.41
As in other countries, the factor that probably will impact most on the number of pulmonologists required in Latin America in the coming years will be the phenomenon of the ageing population.40,41 It is estimated that two-thirds of the clinical activity of pulmonologists consists of attending patients of 65 years of age and older.40 For example, the age group of 65 years and older in Mexico currently comprises 5.9% of the population, but demographic projections indicate that 1 in 10 Mexicans in 2030 and 1 in 5 in 2050 will fall within this group.41 It has recently been calculated that, according to the most conservative recommendations, the deficit of pulmonologists in Mexico could be as high as 1500 specialists (2.3 times the current figure).
In Mexico, as in many other Latin American countries, if corrective measures are not taken, the deficit of specialists will multiply several fold.41,42 Although the cover of the population by paediatric pulmonologists and chest surgeons has not been analysed in detail, it is obvious that in general their numbers are much lower, so the challenges in this area can be expected to be greater.
Human Resources TrainingThe distribution of academic faculties specialising in respiratory medicine is also unevenly distributed throughout Latin America. Table 2 shows the number of academic faculties per country and the duration of the study programmes, including the prerequisite internal medicine and respiratory care programme. Only Brazil and Argentina have a substantially high number of specialised faculties: 27 and 20, respectively. Another 13 countries have between 1 and 8 faculties, while 3 countries in Central America do not have any. In 7 countries, a selection process for medical residency is organised on a national basis, and in 6 countries only (31.6%) is there a single national academic programme. Only 2 counties reported having joint pulmonology and critical care programme, one in Ecuador, which they reported is currently under review, and another in Mexico (one of its 6 academic faculties). With the exception of Chile and Colombia, all countries provided funding to medical residents, which generally ranged from an equivalent of 700 to 1500 US dollars.
Number of Specialist Academic Faculties and Duration (Years) of Respiratory Medicine Training Programme in Latin America.
| Country | Specialist schools | Years of training | Professionals qualified/year | ||
| Internal medicine | Respiratory medicine | Total | |||
| Argentina | 20 | 1–3 | 3 | 4–6 | 20 |
| Bolivia | 3 | 1 | 3 | 4 | 6 |
| Brazil | 27 | 2 | 2 | 4 | 75 |
| Chile | 2 | 3 | 2 | 5 | 6 |
| Colombia | 5 | 3 | 2 | 5 | 5–8 |
| Costa Rica | 4 | 2 | 2 | 4 | 3–6 |
| Cuba | 3 | 1 | 3 | 4 | 3–8 |
| Dominican Republic | 2 | 3 | 3 | 6 | 4 |
| Ecuador | 1 | 3 | 3 | 6 | 1 |
| El Salvador | 1 | 3 | 2 | 5 | 2 |
| Guatemala | 0 | – | – | – | – |
| Honduras | 0 | – | – | – | – |
| Panama | 2 | 1–4 | 3 | 4–7 | 30 |
| Paraguay | 2 | – | 3 | 3 | 6–8 |
| Peru | 8 | – | 3 | 3 | 10 |
| Mexico | 6 | 1–4 | 3 | 4–7 | 30 |
| Nicaragua | 0 | – | – | – | – |
| Uruguay | 1 | 1 | 2 | 3 | 2 |
| Venezuela | 4 | 1–3 | 2 | 3–5 | 9 |
The duration of the respiratory medicine training programmes is usually between 2 and 3 years. However, the total number of years required varies from country to country, since the prerequisites for internal medicine qualifications vary widely, from no requirement to up to 4 years (Table 2).
ConclusionsLatin America is facing significant healthcare challenges, particularly in the area of respiratory health. The demographic changes occurring in these countries, particularly the significant growth in population and increased ageing, and the process of development and globalisation, favour urban immigration and acculturation, including the adoption of sedentary lifestyles and changes in eating habits, leading to rising obesity rates, even in the presence of child malnutrition. Countries in the region have high levels of tobacco use and exposure to domestic and environmental contaminants. The high rates of respiratory diseases with significant morbidity and mortality are an important burden on the economy and social welfare of these countries. In contrast, there is an acute lack of human resources in specialised healthcare in respiratory medicine, for example, the cover of the population by pulmonologists. Specialist academic faculties for respiratory medicine training are scarce and even non-existent in most Latin American countries. Requirements for internal medicine qualifications and academic and practical training programmes vary widely among the countries, and often within them. Increasing the number of specialist medical schools, residencies in specialities and widely regulated, integrated programmes must be a common goal for countries in the region; otherwise, the lack of specialists, the underdevelopment of respiratory specialisation and the lack of medical cover for the population will persist for many years.
FundingCommittee for Continuing Medical Education of the Latin American Chest Association (ALAT). Department of Teaching, The Ismael Cosío Villegas National Institute of Respiratory Diseases, Mexico DF, Mexico.
Conflict of InterestThe authors state they have no conflict of interests.
Dr Gustavo Zabert, former Chairman, Asociación Argentina de Medicina Respiratoria (AAMR). Dr José Jardím, Professor of Respiratory Medicne, Escuela Paulista de Medicina, Universidad Federal de São Paulo, Brazil. Dr Marco Antonio García, Chairman, Sociedad Boliviana de Neumología. Dr Patricia Schonnfeltd and Jessica Tapia, Sociedad Chilena de Enfermedades Respiratorias. Dr Carlos Torres, Fundación Neumológica Colombiana. Dr José Alberto Mainieri Hidalgo, Chairman, Asociación Costarricense de Neumología y Cirugía de Tórax. Dr Juan Carlos Rodríguez Vázquez, Clinical Vice-Director, Hospital Hermanos Ameijeiras, La Habana, Cuba, and the Sociedad Cubana de Neumología. Dr Salvador Martínez Selmo, Dominican Republic. Dr Fernando Cano Pazmiño, Ecuador. Dr Mark Cohen, Guatemala. Dr Miguel Ángel Salazar Lezama, Chairman, Sociedad Mexicana de Neumología y Cirugía de Tórax. Dr Jorge Cuadra, Nicaragua. Dr Mario Lanza, Honduras. Dr Johnny Galina, Chairman, Asociación Panameña de Neumología y Cirugía de Tórax. Dr Guillermo Arbo, Chairman, Sociedad Paraguaya de Neumología. Dr Katherine Gutarra Chuquin, former Chairman, Sociedad Peruana de Neumología. Dr María Victorina López Varela, Uruguay. Dr Gur Levy, Venezuela.
Please cite this article as: Vázquez-García JC, Salas-Hernández J, Pérez Padilla R, Montes de Oca M. Salud respiratoria en América Latina: número de especialistas y formación de recursos humanos. Arch Bronconeumol. 2014;50:34–39.