Pancreatic-thoracic fistula (PTF) is an extremely rare complication of chronic pancreatitis or pancreatic trauma. We report the case of a patient in whom this complication resulted in severe respiratory failure.
This was a 46-year-old man, with a history of smoking, alcoholism, emphysematous type COPD, and chronic pancreatitis with pancreatic pseudocyst, which required percutaneous drainage 5 months prior to the admission referred to in this report.
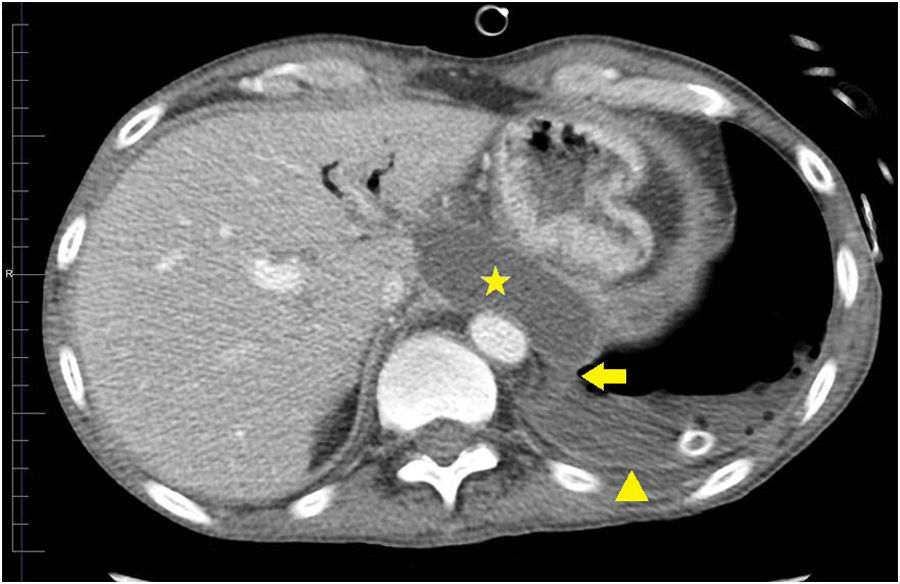
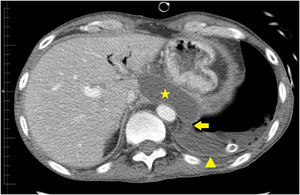
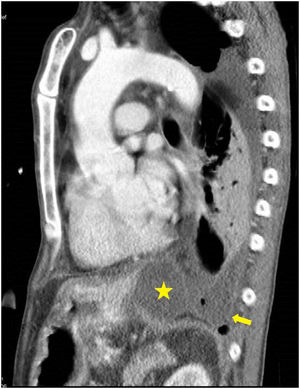
He was taken to a hospital emergency department by the ambulance services in a situation of severe hypoxemic respiratory failure and semi-consciousness. The chest X-ray showed an interstitial alveolar pattern throughout the right lung field and left hemithorax white-out, with right tracheal deviation, suggestive of massive pleural effusion. Orotracheal intubation was performed, after which a left chest tube was placed. Severe respiratory failure persisted, and a bilateral interstitial alveolar pattern with an image of left pneumothorax was observed, probably associated with limited lung compliance and mechanical ventilation. Another left chest tube was then placed, without improvement. The patient was referred to our center. Pleural fluid biochemistry was: glucose 181 mg/dl, protein 3 g/dl, LDH 528 IU/l, and amylase 14,106 IU/l. Microbiological cultures of pleural fluid, tracheal aspirate, blood, and urine were negative. In view of these results, the possibility of PTF was suggested. There were no signs of heart failure, no changes were observed on echocardiogram, and no involvement of other organs or systemic inflammatory response were detected. A third chest tube was placed, with some reduction of the pneumothorax. The patient subsequently improved progressively, with disappearance of the alveolar-interstitial infiltrate, and he was weaned from mechanical ventilation after a 9-day of stay in the intensive care unit. We then performed a CT scan of the chest and abdomen which revealed PTF (Figs. 1 and 2). The patient was discharged home.
PTF is caused by a disruption of the pancreatic duct, which causes pancreatic secretions to leak to the thorax through the aortic or esophageal hiatus,1 causing mediastinal pseudocyst,2,3 pancreatic-bronchial fistula, pancreatic-pericardial fistula,4 or pancreatic-pleural fistula.5 Most cases of PTF are caused by chronic pancreatitis. The case described here was a pancreatic-pleural fistula. Computed tomography,6 magnetic resonance imaging (MRI), MRI cholangiopancreatography, and endoscopic retrograde cholangiopancreatography are used for diagnosis. The latter 2 procedures help locate the disruption more precisely. Treatment involves the suspension of enteral diet, the administration of somatostatin or octreotide, and the endoscopic placement of a pancreatic stent or suturing of the disruption in open surgery. Conservative treatment is another option,7 and was the approach selected for our patient, consisting mainly of drainage of pleural fluid. The clinical outcome was favorable. We decided to offer conservative treatment due to the patient’s good initial response after placement of the last pleural drainage in our center. This was also the reason why we did not request an MRI cholangiopancreatography during the patient’s stay in intensive care.
Although this complication is rare, it should be borne in mind due to its clinical impact, especially in patients with chronic pancreatitis and massive left pleural effusion.
Please cite this article as: Arméstar F, et al. Insuficiencia respiratoria secundaria a fístula pancreático-torácica. Arch Bronconeumol. 2019;55:656–657.