The Coronavirus Disease 2019 (COVID-19) pandemic remains a global emergency ever since the first SARS-CoV-2 infections were reported over two years ago, causing a great impact on the health of the population and public consumption around the world. Because of the continuously changing characteristics of SARS-CoV-2, reflections on changing the COVID-19 response strategy are pivotal. They serve as preparation to strengthen the anti-pandemic efforts and scientifically respond to future outbreaks, which will guarantee the proper functioning of society.
Analysis of the COVID-19 situation in the world and ChinaThe COVID-19 pandemic has not ended yet. As of May 25, 2022, 524 million confirmed cases and 6.28 million deaths have been reported worldwide,1 with 65.8% of the global population having received at least one dose of vaccine.2 Recently, the number of new confirmed cases and the case fatality ratio in the six World Health Organization (WHO) regions has been declining visibly.3 The WHO statement highlighted that the virus will continue to evolve, but the severity of the disease will reduce over time as immunity increases due to vaccination and infection.4
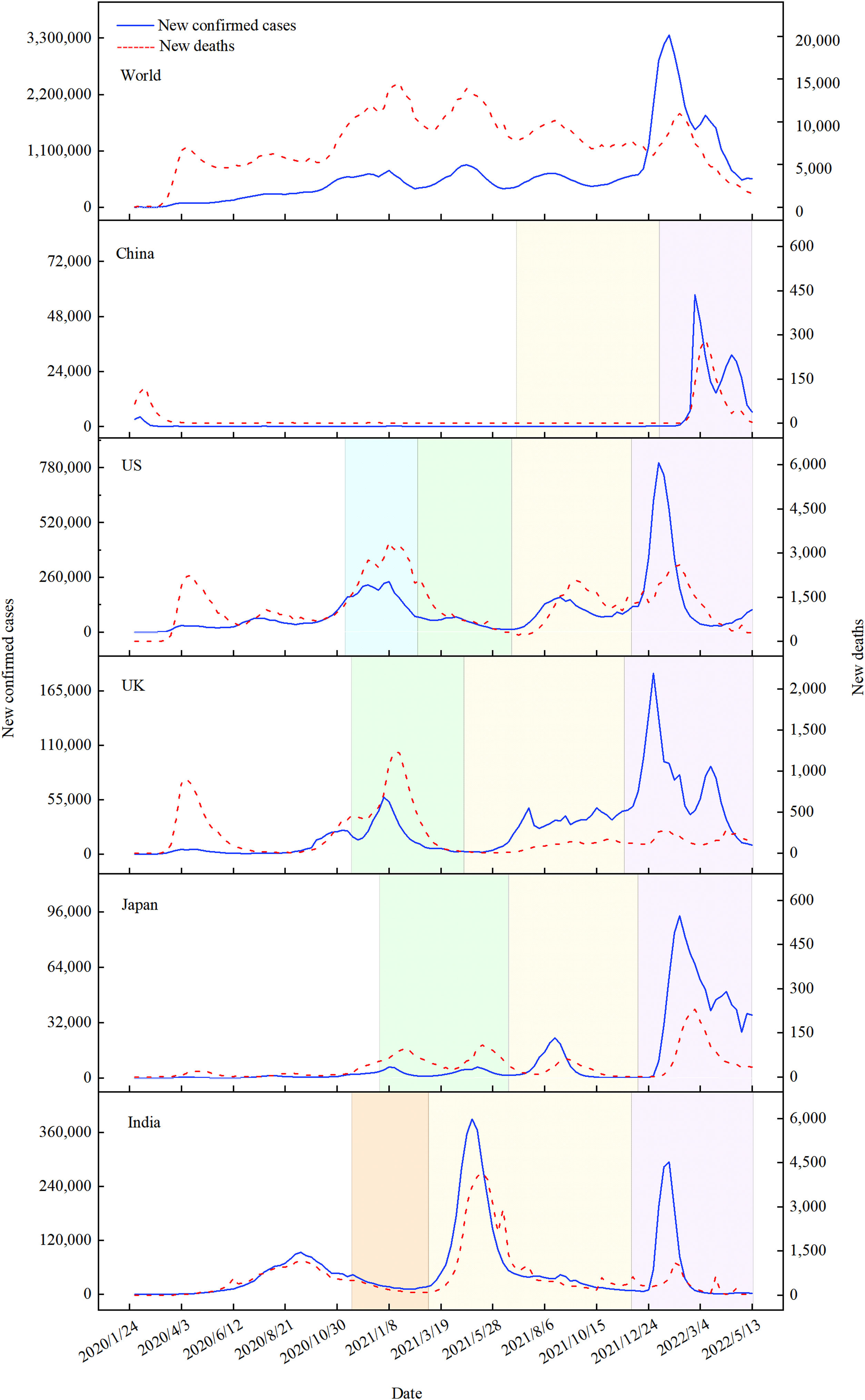
In terms of the situation across different countries and regions, there are variations related to factors such as the circulating viruses, number of waves, chances of exposure, policies and response capacity, health service provision and accessibility, such as nucleic acid and antigen tests, surveillance, diagnosis, screening, and disease-related subsidy policies. At present, the world in general is still at the peak of the fourth wave of the COVID-19 pandemic, and countries are in a different status due to varying public health interventions and dominant variants. For example, India, Japan, the United Kingdom (UK), and the United States (US) have all suffered from phased attacks caused by ancestral SARS-CoV-2, and Alpha, Delta, and Omicron variants. Moreover, India and the US have also had outbreaks of other confounding mutant strains (Fig. 1).5
Number of new confirmed cases and deaths of COVID-19 in selected countries worldwide. The shaded areas represented different variants, where green, yellow, and purple referred to Alpha, Delta, and Omicron, respectively, while the lake blue and orange both indicated multi-variants. The curve without shading was a stage of ancestral virus pandemic.
In mainland China, adjusted response objectives and strategies were adopted at different stages based on the epidemiological characteristics of COVID-19, each of which has yielded excellent effectiveness in prevention and control. The first stage (December 27, 2019–January 19, 2020) was a swift response to the public health emergency. In the second stage (January 20, 2020–February 20, 2020), making people's lives and health its first priority, China adopted extensive, stringent, and thorough containment measures to prevent inbound and intra-city transmissions, and succeeded in initially containing the virus. In the third stage (February 21, 2020–March 17, 2020), the number of newly confirmed domestic cases on the Chinese mainland dropped to single digits. Differentiated control measures were adopted to address the problems in different regions. The city of Wuhan and Hubei province continued upholding the measures for preventing the virus from spreading within their local area and beyond. In the fourth stage (March 18, 2020–April 28, 2020), China won a critical battle in defending Wuhan and Hubei province against COVID-19, which was a major step forward in the nationwide effort to control the virus. Chinese government adopted an approach to prevent the coronavirus from entering the country and halt its domestic resurgence. The continuing prevention and control have been going well in the fifth stage (since April 29, 2020) when the strategy of “dynamic zero COVID-19” was proposed in addition to the previous policy. Thereafter, China has continued to hierarchically elevate the level of differentiated and precise prevention and control, quickly and effectively deal with localized clusters, maximize the protection of people's lives and health, and maintain a global leadership position in economic development and COVID-19 response.6
China's response has shown achievements in COVID-19 morbidity and mortality. However, we should be highly aware of the complexity, magnitude, and recurrence of the pandemic, and remain vigilant at all times. Over three billion doses of vaccines have been distributed in China, and 88% of the population has been fully vaccinated.7 Currently, a low natural-induced immunity rate and short duration of vaccine-induced immunity in China have generated an “immune gap” with countries that have had multiple waves of natural infections and high vaccine coverage. The recommendation from WHO to lift or relax international travel restrictions poses a new challenge for China in resuming normal international travel.
As the predominant strain in the current global pandemic, Omicron has a shorter incubation time (approximately 3 days),8 faster transmission rate,9 and greater infectivity than previous variants such as Delta. Since January 2022, Omicron-related outbreaks of various scales have successively surfaced in Hong Kong SAR, Shanghai, Beijing and other cities, forming the most urgent and severe scenario since the first Wuhan lockdown lifted. It has alerted the huge population of China again that lifting public health measures, while Omicron is rapidly spreading, would create opportunities for SARS-CoV-2 to spread and even lead to large-scale outbreaks.
Countermeasures for prevention and control in the futureThere is a high degree of uncertainty in the mutation and evolution of SARS-CoV-2, as it is characterized by diverse and variable pathogens, complex and diverse sources of infection, transmission factors, and infection spectrum. It remains unpredictable when the pandemic will transform into an endemic status.
China has a large geographical area and huge population size, and the proportion of elderly people aged 60 and 65 years or older is 19% and 14%, respectively. In light of this, China is currently adhering to the general policy of “dynamic zero-COVID”, while further improving the level of scientific and strict prevention and control, and continuously optimizing response initiatives.
The four core points of strict prevention and control are: “earlier”, “smaller”, “stricter”, and “more practical”. “Earlier” refers to the early detection and response to infections and outbreaks. Early detection of latent COVID-19 dissemination requires a strict, sensitive, and professional disease surveillance and reporting system. “Smaller” pertains to keeping the scope of management as small as possible so that the social cost and the impact on production and daily life can be minimized. “Stricter” means that the interventions should be stringent while avoiding loopholes; especially the monitoring and protection of vulnerable populations such as the elderly should not be neglected. “More practical” implies that measures against COVID-19 should be put into practice, not merely being formalized. Rough handling not only consumes valuable resources but also overlooks the focus of response efforts and the priority populations. The above four points demand a higher level of governance. In addition to an effective response, these measures can reduce the impact on production and daily life to the maximum extent, and achieve a win–win situation of fighting against COVID-19 and economic construction at minimal social cost.
Professional surveillance networks should be enhanced, which include the fever clinic, and symptom and pathogen surveillance. Surveillance and early warning networks should operate well routinely, aiming to detect and notify abnormal signals and outbreaks, grasp pathogenic variation, and respond to an emergency. Furthermore, reinforced monitoring and research on virus mutation necessitate the inclusion of real-time statistics on COVID-19 morbidity, mortality, severe illness and hospitalization rates, and changes in disease transmissibility and virulence to provide scientific evidence for the dynamic assessment of epidemic trends.
It is imperative to improve the rate of completed vaccination and booster shots in high-risk populations, especially the elderly. For example, during the outbreak in Hong Kong SAR, the second dose vaccination rate of people over 80 years old was only 33.43%. Ninety-one percent of deaths occurred in unvaccinated people or those who only received one dose.10 The case fatality rate was significantly higher in the unvaccinated population than in those who have received two doses. Since China is an aging society and has a substantial elderly population, they constitute a large proportion of high-risk groups for severe COVID-19 illness and fatal outcomes. COVID-19 vaccine booster shots can effectively reduce the risk of severe disease and death associated with the Omicron infection. Therefore, accelerating the rollout of COVID-19 booster vaccines among the eligible priority groups as widely as possible is an urgent matter.
Promoting the multichannel development and stockpiling next-generation COVID-19 vaccines and antiviral drugs should be continually enhanced. The emergency production and technical inventory of vaccines and drugs are essential in the preparation against continuously evolving variants. Moreover, it is necessary to explore alternative technologies for future vaccine strains, which are encouraged in the development of universal SARS-CoV-2 vaccines to provide multiple options for pandemic response. Compared to neutralizing antibodies, small molecule chemicals have the advantages of convenience and accessibility. China has granted conditional approval for the import of Paxlovid.11 Molnupiravir has also received emergency approval for use in the UK and other countries.12 The development and accelerated launch of small-molecule chemicals should be supported to provide a technical reserve in the response to variants that may emerge in the future.
A system for the reservation and distribution of medical and public health resources should be developed and suitable for both periods of peace and outbreak. During a flexible window period for preparation, weekly inventories of the number of personnel and equipment resources related to medical treatment, laboratory testing, and epidemiological research, including isolation beds, ICU beds, ventilators, epidemiological investigators, sampling personnel, testing reagents and consumables, etc., and timely adjustment of resource assessment based on the situation are warranted. The immediate launch of an emergency response, the construction of a backup emergency response team of non-respiratory infection specialists and medical students, as well as specialized training in respiratory support and intensive care, is also essential to improve the protection of the population's health and lives. If a shortage of medical resources occurs, public facilities such as stadiums, exhibition halls, hotels, and schools should be requisitioned as Fangcang shelter hospitals to isolate mild cases.13
In conclusion, there are many complex and unpredictable factors in fighting the COVID-19 pandemic. As the anti-pandemic rules are being refined, SARS-CoV-2-related surveillance, vaccination, novel vaccines and drugs research and storage, assessment and deployment of medical resource demand, and the peacetime-wartime transition pattern are the key points to improve the avoidance of risks and response to virus transmission.
FundingThis work was funded by the Chinese Academy of Medical Sciences (CAMS) Innovation Fund for Medical Sciences (No. 2021-I2M-1-044), the Non-profit Central Research Institute Fund of Chinese Academy of Medical Sciences (No. 2021-RC330-002) and the Special Fund for Health Development Research of Beijing (No. 2021-1G-3013).
Conflicts of interestNone.