Patients with chronic bronchiectasis (BQ) may suffer from psychological disorders. The objective of this study was to assess the presence of anxiety and depression in patients from a specialised BQ Unit, using validated questionnaires.
Patients and methodsWe included patients consecutively diagnosed with BQ (unrelated to cystic fibrosis) by high resolution computed tomography in the study. Patients were clinically stable in the previous three weeks and voluntarily completed the Beck Depression Inventory, State-Trait Anxiety Inventory and St. George's Respiratory Questionnaire, after signing the informed consent. They were classified according to their scores on the psychological screening questionnaires, and their results were compared with the clinical, radiological and functional parameters and Quality of Life.
Results70 patients were included, 48 women and 22 men, with a mean age of 64.19 years. Thirty-four percent (34%) of patients showed symptoms of depression, and around 55% had scores above the 50th percentile in trait and state anxiety. The amount of sputum was associated with trait anxiety. Bacterial colonisation was related to anxiety (trait and state), especially Pseudomonas aeruginosa colonisation. Female patients showed a higher risk of depression. There was no relationship between the Quality of Life scores and the established classifications of anxiety and depression.
ConclusionsA high percentage of patients with BQ presented anxiety (trait and state) and depression. The daily sputum production and bacterial colonisation (especially with P. aeruginosa) were the variables most related to anxiety; depression was more common in women. We believe that the presence of psychological disorders should be evaluated, especially in patients with this profile.
los pacientes con bronquiectasias (BQ), como enfermos crónicos, pueden verse afectados por trastornos psicológicos. El objetivo del trabajo fue valorar la presencia de síntomas de ansiedad y depresión, mediante cuestionarios validados, en pacientes con BQ controlados en una Unidad Monográfica.
Pacientes y métodosde forma consecutiva se incluyeron en el estudio pacientes diagnosticados de BQ, no relacionadas con fibrosis quística, mediante una tomografía axial computerizada de alta resolución. Los enfermos estaban en fase estable en las últimas 3 semanas y cumplimentaron los cuestionarios: Inventario de depresión de Beck, Escala de ansiedad estado-rasgo y St George, después de firmar el consentimiento informado. Los pacientes fueron clasificados según las puntuaciones obtenidas en los cuestionarios de cribado psicológico y sus resultados se compararon con las variables clínicas, radiológicas y funcionales y las puntuaciones de calidad de vida.
Resultados70 enfermos, 48 de ellos mujeres y 22 hombres, con una edad media de 64,19 años respondieron de forma voluntaria a los cuestionarios. El 34% de los pacientes mostraron síntomas de depresión y alrededor del 55% puntuaciones por encima del percentil 50 en ansiedad (rasgo y estado). La cantidad de expectoración se relacionó con la ansiedad rasgo. La colonización bacteriana se relacionó con la ansiedad (rasgo y estado), especialmente la colonización por Pseudomonas aeruginosa. El sexo femenino, mostró mayor riego de depresión. No existió relación entre las clasificaciones establecidas de ansiedad y depresión y las puntuaciones de calidad de vida.
Conclusioneslos pacientes con BQ muestran en un alto porcentaje presencia de síntomas de ansiedad, rasgo y estado, así como de depresión. Los más afectados por ansiedad son los más expectoradores y los colonizados por bacterias, y por depresión las mujeres. Creemos que es necesario valorar la presencia de psicomorbilidad asociada, especialmente en este perfil de enfermos.
Approximately two decades ago, non-cystic fibrosis (CF) bronchiectasis (BQ) was considered by Barker (1988) as an “orphan disease”, bereft of research studies, epidemiological data and interest by the pharmaceutical industry.1,2 It must be said, however, that the situation is changing, and BQ currently represents a more common than expected condition with a large impact on health and capable of causing significant respiratory morbidity and mortality.
Twenty years later, there continues to be little data on the incidence and prevalence of BQ, although it is estimated that these are low in industrialised countries and higher in developing countries. Thus in the native Alaskan population, the prevalence varies between 10 and 20/1000 population, while in the US it is calculated that it could be around 53 cases/100000 adults.3,4 Nevertheless, various data are available that lead us to believe that its prevalence is continuing to rise as a result of transplants, immunosuppressant treatment, the human immunodeficiency virus (HIV) epidemic, the return of tuberculosis, a longer life expectancy and, especially, the chronic nature of respiratory diseases.
Without question, the reason for the higher number of BQ diagnoses is due to the introduction of high resolution computed tomography (HRCT), which has enabled the lung parenchyma to be viewed in more detail, demonstrating that BQ is more common than expected and moreover, the cylindrical forms are able to modify the prognosis of the diseases that generate them.5,6
Quality of life studies in patients with BQ are important for determining their clinical status, which sometimes differs from the lung function or radiological extension, and for assessing the general response to treatments.7,8 An improvement in the quality of life has been achieved in patients with BQ in recent years, thanks to early diagnosis by HRCT, a notable improvement in treatment, respiratory physiotherapy and proper management of associated comorbidities.9
Patients with chronic lung diseases often have symptoms of depression, anxiety or both, causing deterioration in the quality of life, social and recreational functioning and, in some cases, affecting therapeutic compliance.10 Thus, it is important to evaluate the patient's condition from a psychological point of view, and to assess how these disorders could interfere in daily life. Patients with BQ, as chronically ill patients, can also suffer from psychological disorders, although there are few studies in this respect.11,12 As a working hypothesis, we proposed that patients with non-cystic fibrosis bronchiectasis (non-CF BQ) could have a high prevalence of depression and anxiety, and that these could be related with different clinical parameters. The aim of this study was to assess the presence of anxiety and depression symptoms using psychological screening questionnaires, in a sample of patients with non-CF BQ from a specialised BQ unit. We also aimed to assess how the main clinical variables and quality of life affect the psychological morbidity.
Patients and MethodsSeventy patients diagnosed with BQ by HRCT (using a 1mm or 1.5mm collimation technique at 10mm intervals in maximal inspiration, according to the criteria of Naidich et al.13), who consecutively attended the specialised BQ unit of Hospital Universitario de la Princesa (Madrid, Spain) were enrolled in the study. Patients diagnosed with CF (sweat test >60mmol/l or presence of clinically compatible mutations),9 those with symptoms of acute exacerbation in the previous three weeks and those who presented disease with a poorer prognosis for survival than the BQ itself and terminally ill patients were excluded.
The age, sex, body mass index (BMI) and smoking habits were collected, classifying the latter into non-smoker, ex-smoker (when the patient had not smoked for 1 year) and active smoker. The possible aetiologies of the BQ were established after performing the tests recommended in the diagnostic algorithm laid down in the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR) Bronchiectasis Guidelines.9 The following were evaluated: the Charlson comorbidity index,14 dyspnoea grade according to the Medical Research Council (MRC) scale,15 usual amount of expectoration in ml, estimated by the patient in 24h measured in: teaspoon (5ml), dessert spoon (10ml), wine glass (100ml) or water glass (200ml), and the macroscopic appearance of the secretions, classified into four grades: mucous (whitish), mucopurulent (light yellow), purulent (greenish) and brownish. The presence of haemoptysis ≥100ml/day and sinusitis (defined by suggestive symptoms: nasal blockage, postnasal drip, rhinorrhoea and local pain and/or consistent findings on the paranasal sinus CT scan) was assessed. Lung function tests were carried out close to completion of the questionnaire, using a spirometer (Vmax Sensormedics). BQ was classified by HRCT according to type (cylindrical or cystic) and extension of their location into: localised, if they affected a single lobe, and diffuse, if they affected more than four lobes (assessing the lingula as an independent lobe), unilateral, if they were present in a single lung and bilateral, if they were observed in both lungs. Data were also collected on previous bacterial colonisation, defined as the presence of the same microorganism in three consecutive samples with a minimum interval of one month, and whether they received aerosol antibiotic treatment. Respiratory exacerbations were evaluated, defined as the need for antibiotic treatments due to an increase in respiratory symptoms, and hospitalisation in the previous 2 years for this reason, and whether they received any treatment for anxiety or depression.
Patients completed the following questionnaires voluntarily, after having signed the informed consent form:
- -
Beck Depression Inventory (BDI-II): this is a 21-item questionnaire used to evaluate the severity (symptomatic intensity) of depression. For each item, the patient has to select the answer that best reflects his or her state at the present time and during the past week. The total score is obtained by adding the values of the selected phrases, which range from 0 to 3. The score obtained ranges from 0 to 63 points. The commonly accepted cut-off points for grading the intensity/severity are as follows: 0–9: no depression, 10–18: mild depression, 19–29; moderate depression and ≥30 points severe depression.16 However, higher cut-off points are recommended in patients with chronic disease.17 Therefore, we divided the patients into two groups: “no symptoms of depression” (<14) and “symptoms of depression” (≥14).
- -
State-Trait Anxiety Inventory (STAI): this is a questionnaire composed of 20 items that assess “state anxiety” (temporary emotional state influenced by environmental factors that protect from or generate anxiety) and a further 20 items that evaluate “trait anxiety” (personality factor that predisposes an individual to suffer from anxiety). The score of both parts classifies patients into a percentile with respect to the general population. The general population are classified by sex and age18 (Table 1).
- -
St. George's Respiratory Questionnaire (SGRQ): this is a 50-item questionnaire (76 levels) divided into three components: symptoms, activity and impact. The score for each of the scales and a total score are calculated. The range of possible scores is between 0 (no impairment in quality of life) and 100 (maximum impairment in quality of life).19
The patients were not assessed by Mental Health specialists.
Statistical AnalysisDescriptive analysis of the quantitative variables was performed by calculating the means and standard deviations, using the percentage for the qualitative variables. The normality of the variables was verified using the Kolmogorov–Smirnov test; non-parametric tests were used in the absence of a normal distribution. Patient subgroups established by the psychological questionnaires were analysed (state-trait anxiety percentiles and according to the cut-off point in depression). The Chi-squared test was used for qualitative clinical variables and the Student's t-test for comparison of means when two subgroups were compared, using analysis of variance when there were more than two. All calculations were performed using SPSS v.15.0; P values <.05 were considered statistically significant in all cases.
ResultsCharacteristics of Patients With BronchiectasisTable 2 shows the patient characteristics and quality of life scores. With respect to the bronchiectasis aetiologies, 22 were secondary to tuberculosis, 6 to childhood infections, 1 to immotile cilia disease, 2 to immunoglobulin deficiency, 1 to post-lung transplant, and in 32 patients the cause could not be determined. Eight patients had asthma and 4 had COPD. Seventy-three percent (73%) of patients had cough and dyspnoea. With respect to chronic colonisation, 21 patients were colonised, 15 (71.4%) by Pseudomonas aeruginosa, 4 (19%) by Haemophilus influenzae, 1 by Moraxella catharralis and 1 by Staphylococcus aureus. Of the 21 patients with chronic colonisation, 16 (21.6%) received inhaled antibiotic treatment. Eleven patients received treatment for anxiety and 6 for depression.
Patient Characteristics.
| Variables | Results |
| Age (years), X±SD | 66.2±14.22 |
| Sex ♀/♂, n | 51/23 |
| BMI (kg/m2), X±SD | 24.56±3.81 |
| Smoking habit, % | |
| Non-smokers/ex-smokers/active smokers | 64.9/25.7/9.5 |
| Charlson Index, X±SD | 0.85±1.25 |
| MRC dyspnoea Grade 1/Grade 2, % | 47.3/27 |
| Estimated amount sputum/day, % | |
| <5ml | 25 |
| 5–30ml | 50 |
| >30ml | 25 |
| Colour, % | |
| Mucous | 35 |
| Mucopurulent | 38 |
| Purulent | 22 |
| Brownish | 4 |
| Haemoptysis ≥100ml/day/sinusitis, n | 4/5 |
| %FVC | 85.11±20 |
| %FEV1 | 74±23 |
| Cystic/diffuse bronchiectasis, % | 20/55 |
| Bacterial colonisation/P aeruginosa, n | 21/15 |
| Respiratory exacerbations (X±SD) | 2.58±1.46 |
| Hospitalizations, X±SD | 0.29±0.54 |
| SGRQ total | 32.55±19.1 |
| SGRQ symptoms | 41.48±21.40 |
| SGRQ activity | 41.12±24.64 |
| SGRQ impact | 23.84±19.16 |
FEV1, expiratory volume in the first second; FVC, forced vital capacity; BMI, body mass index; MRC, Medical Research Council; P. aeruginosa, Pseudomonas aeruginosa; SD, standard deviation; SGRQ, St George's respiratory questionnaire; X, mean.
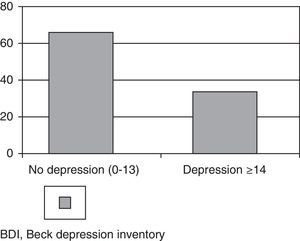
After analysing the results of the Beck depression Inventory using a cut-off point of 14, 34% of patients had symptoms of depression (Fig. 1).
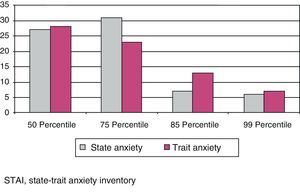
State-Trait Anxiety InventoryThe results obtained in the STAI questionnaire showed that, with respect to the general population, 43 patients (58.1%) were above the 50th percentile for state anxiety, and 42 patients (56.8%) for trait anxiety (Fig. 2).
Twenty-one patients had symptoms of both anxiety and depression. The scores in the questionnaires were related with the most significant clinical variables, such as age, sex, dyspnoea, cough, amount of expectoration, lung function, localised or diffuse extension of the BQ, chronic colonisation, exacerbations and hospitalisations in the previous 2 years.
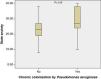
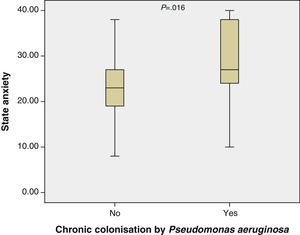
State-trait Depression and Anxiety and Clinical VariablesThe amount of expectoration was significantly related with trait anxiety (P=0.024). A relationship was also found between anxiety (state and trait) and bacterial colonisation (P=.037), and specifically with colonisation by Pseudomonas aeruginosa (P=.16) and trait anxiety (Tables 2, 3 and 4 and Fig. 3). The depression scores were related with sex, with women being more affected.
Relationship of STAI and BDI Questionnaires With the Clinical Variables.
| Age, years Mean±SD | BMI, kg/m2 Mean±SD | Charlson Mean±SD | Amount of expectoration, mlMean±SD | %FEV1 Mean±SD | Exacerbations Mean±SD | Hospitalizations Mean±SD | |
| STAI (State), n | |||||||
| P50 (27) | 62.2±12.9 | 23.4±3.6 | 1.2±1.6 | 20±27 | 72.1±24.3 | 2.4±1.3 | 0.3±0.6 |
| P75 (31) | 65.9±15.1 | 25.5±3.6 | 0.6±0.9 | 28±24.5 | 70.4±19.9 | 2.8±1.4 | 0.3±0.5 |
| P85 (7) | 75.1±8.5 | 23.4±3.8 | 0.4±0.7 | 22.1±35.3 | 88.87±26.1 | 1.7±0.9 | 0±0 |
| P99 (5) | 66.1±16.8 | 23.2±3.9 | 0±0 | 44.1±43.4 | 89±26 | 3.1±2.1 | 0.6±0.5 |
| P | .195 | .138 | .085 | .281 | .103 | .225 | .191 |
| STAI (Trait), n | |||||||
| P50 (28) | 62.3±12.7 | 23.6±4 | 1.1±1.4 | 26.9±31.9 | 73.1±23.5 | 2.6±1.6 | 0.3±0.6 |
| P75 (23) | 64.8±16 | 25.1±3.7 | 0.6±1.1 | 22±19.2 | 70.5±21.7 | 2.4±1.3 | 0.3±0.5 |
| P85 (13) | 74.5±7.4 | 23.5±2.8 | 0.4±0.6 | 14.2±13.9 | 83.8±25.4 | 2.3±1.2 | 0.1±0.3 |
| P99 (6) | 63±17.8 | 25.6±4.1 | 0.4±1.1 | 53.5±43.8 | 75.2±24.1 | 3.4±1.7 | 0.4±0.5 |
| P | .360 | .071 | .276 | .024 | .430 | .381 | .674 |
| BDI | |||||||
| <14 (49) | 64.4±13 | 24.5±3.8 | 0.9±1.3 | 24.5±26.9 | 71.5±21.7 | 2.5±1.4 | 0.2±0.5 |
| ≥14 (25) | 70±15.9 | 24.7±3.9 | 0.6±1 | 26.6±30.7 | 79.2±24.9 | 2.6±1.5 | 0.4±0.6 |
| P | .110 | .761 | .305 | .761 | .179 | .247 | .247 |
BDI, Beck Depression Inventory; BMI, body mass index; FEV1, expiratory volume in the first second; SD, standard deviation; SGRQ, St George's respiratory questionnaire; STAI, State-Trait Anxiety Inventory; X, mean.
STAI and BDI Questionnaire With the Clinical Variables.
| Sex | Cough | Dyspnoea, MRC | Bacterial colonisation | Bronchiectasis | |||||||
| Female | Male | Yes | No | 0 | 1 | 2 | No | Yes | Diffuse | Localised | |
| STAI (State), n | |||||||||||
| P50 (27) | 17 | 10 | 18 | 9 | 8 | 11 | 8 | 23 | 13 | ||
| P75 (31) | 19 | 11 | 24 | 6 | 6 | 17 | 7 | 22 | 18 | ||
| P85 (7) | 6 | 1 | 4 | 3 | 3 | 3 | 1 | 5 | 4 | ||
| P99 (5) | 6 | 0 | 5 | 1 | 2 | 2 | 2 | 1 | 3 | ||
| P | .214 | .475 | .790 | .009 | .832 | ||||||
| STAI (Trait), n | |||||||||||
| P50 (28) | 20 | 8 | 22 | 6 | 9 | 12 | 7 | 23 | 5 | 18 | 10 |
| P75 (23) | 14 | 8 | 15 | 7 | 5 | 12 | 5 | 17 | 5 | 7 | 15 |
| P85 (13) | 10 | 3 | 7 | 6 | 2 | 7 | 4 | 9 | 4 | 5 | 8 |
| P99 (6) | 4 | 3 | 7 | 0 | 3 | 2 | 2 | 2 | 5 | 2 | 5 |
| P | .753 | .128 | .815 | .037 | .082 | ||||||
| BDI | |||||||||||
| <14 (49) | 29 | 20 | 34 | 15 | 13 | 24 | 12 | 36 | 13 | 25 | 24 |
| ≥14 (25) | 22 | 3 | 21 | 4 | 6 | 11 | 8 | 13 | 8 | 8 | 17 |
| P | .009 | .140 | .789 | .408 | .095 | ||||||
BDI, Beck Depression Inventory; SD, standard deviation; SGRQ, St George's respiratory questionnaire; STAI, State-Trait Anxiety Inventory; X, mean.
No relationship was found between the groups established by the psychological screening questionnaires and the quality of life scores (Table 5).
Relationship of BDI and STAI Questionnaires With SGRQ.
| SGRQ total, mean±SD | SGRQ symptoms, mean±SD | SGRQ activity, mean±SD | SGRQ impact, mean±SD | |
| STAI (State), n | ||||
| P50 (27) | 30.5±20.8 | 37.2±22.6 | 38.5±27.4 | 21.7± 19.1 |
| P75 (31) | 34.2±19.1 | 44.1±19.9 | 41.8±22.4 | 25.8±21.1 |
| P85 (7) | 27.4±17.2 | 34±22.1 | 35.8±18.1 | 20±17.3 |
| P99 (5) | 38±13.1 | 55.5±23.2 | 53.48±34.1 | 27±11 |
| P | .709 | .228 | .612 | .799 |
| STAI (Trait), n | ||||
| P50 (28) | 32±22.3 | 38.9±23.5 | 41.4±28.9 | 23.3 ±19.5 |
| P75 (23) | 33.8±18.7 | 43.6±20.7 | 41.4±17.9 | 24.7±22.4 |
| P85 (13) | 33±15.8 | 45.6±20.9 | 40.4±22.3 | 23.6±15.9 |
| P99 (6) | 27.3±16.6 | 33.7±19.6 | 36.3±35.9 | 22.8±15.2 |
| P | .906 | .624 | .975 | .994 |
| BDI | ||||
| <14 (49) | 30.9±19.1 | 41.7±21.9 | 38.9±24.3 | 21.5±18.3 |
| ≥14 (25) | 36±19 | 41.±20.7 | 45.9±25.2 | 28.8±20.4 |
| P | .308 | .902 | .268 | .141 |
BDI, Beck Depression Inventory; SGRQ, St George's respiratory questionnaire; STAI, State-Trait Anxiety Inventory.
Several studies have been published in recent years assessing psychological disorders in chronic respiratory diseases,20 finding a high prevalence of anxiety and depression. Similarly, in patients with BQ, although there are very few studies, a higher prevalence of anxiety and depression has been observed compared to the general population. The presence of psychological morbidity may be associated with poor treatment adherence21 and consequently, worse disease control and a deterioration in the quality of life. There is only one recently published study in Spain that includes a mixed population of patients with BQ (CF and non-CF), but with a lower median age (32 years) than patients we normally see in clinical practice.12 Therefore, we considered it interesting to explore the psychological morbidity exclusively in patients with non-CF BQ, using two validated questionnaires in Spanish, specific for screening depression and anxiety respectively.
There are few studies on this topic in the medical literature, notwithstanding the previously cited study by Olveira et al.12 This study analysed the prevalence of anxiety and depression using the Hospital Anxiety and Depression Scale (HADS), and assessed the quality of life in patients with BQ (with and without CF). The authors reported that 20% of patients had high scores for depression and 38% for anxiety. Age was related with symptoms of both anxiety and depression, and anxiety was related with frequent exacerbations. After controlling for confounding variables, demographic (age and sex) and clinical (exacerbations, daily sputum production, aetiology and spirometry values), both depression and anxiety predicted worse quality of life.
Similarly, the study by O’Leary et al.11 assessed anxiety and depression using the HADS and quality of life using the SGRQ in 111 patients with a mean age of 52 years. The authors found moderate to severe anxiety in 17% of cases and depression in 9%, relating both with the quality of life. Neither anxiety nor depression was related with the extension of the BQ in the HRCT, lung function, PaO2 or sex. Depression was related with dyspnoea, physical and mental fatigue and exercise tolerance.
A Korean study conducted in outpatients, 84 with COPD, 33 with bronchiectasis and 7 with asthma, evaluated using the same questionnaires as those used in our study (BDI-II and STAI), described 55% depression in patients with BQ (similar to COPD) and 39% anxiety (higher than in COPD and asthmatic patients). They concluded that BQ patients who were most affected by psychological symptoms were those with greater bronchial obstruction and a history of smoking.10
In this study, it was observed that more than half the patients had scores above the 50th percentile for anxiety (state and trait), and one-third had depression. Unlike other studies, it was found only that the amount of expectoration and bacterial colonisation, specifically for Pseudomonas aeruginosa, was related with anxiety. Women had higher scores for depression, a finding that does not agree with the aforementioned studies, although it is consistent with data found in the general population, which describe a two or three times higher prevalence of depression in women.22 We did not find any relationship between quality of life and psychological morbidity. Although patients with depression had higher scores, they were not significant on any questionnaire. This could be because patients did not have very high scores on the SGRQ and there could have been other factors such as age, the obligation to have daily treatment, as well as some aspects not considered, like the civil status or social factors, which may have caused the high prevalence of anxiety and depression.
It is important to highlight the proportion of patients with symptoms of depression and anxiety in our study. These differences could be partly due to the older age of the patients enrolled, but mainly to the differences in sensitivity of the questionnaires, as the HADS was used in previous studies while this one used the STAI and BDI-II. Thus, in the Korean study, the percentages were closer to ours. The BDI-II is more sensitive than the HADS, as it evaluates a wide spectrum of depressive symptoms, although as it includes not only symptoms in the cognitive sphere (items 1–14) but in the somatic sphere (items 15–21), these may overlap with those of the disease itself, overestimating the prevalence of depression. In order to avoid this, we increased the cut-off point, as recommended in the literature for chronically ill patients. Similarly, the STAI questionnaire provides more information than the HADS, as its two sub-scales allow differentiation between temporary anxiety (state) and anxious personality (trait). In addition, the patient characteristics or variables analysed were different, which could likewise affect the difference in results. Therefore, studies are required with a larger number of patients using the same questionnaires to refine these differences. It is clear that any psychological disorder can have consequences on therapeutic compliance, and thus on the course of the disease, so their diagnosis is very important. Validated psychological screening questionnaires can help in routine clinical practice to select patients who should be referred to Mental Health specialists.
There are somewhat more studies on psychological morbidity in BQ patients with CF, which also show a high prevalence, although on analysing the relationship with the clinical variables, not all of the results agree, as happened in our case. While some find agreement between the exacerbations and anxiety, not all show a relationship between lung function or extension of the lesions on HRCT with anxiety or depression.23–25
This study has some limitations: the first is the number of patients enrolled and the second, not having used, in addition to the aforementioned questionnaires, the HADS, with which there is previous experience in patients with BQ. The third limitation was not having referred all patients for formal psychological interviews and having been able to establish the sensitivity and specificity of the questionnaires.
We can conclude that there is a high prevalence of depression and anxiety in patients with non-cystic fibrosis bronchiectasis. This disease should therefore be assessed for proper management and to prevent the consequences of psychological morbidity.
Conflict of InterestsThe authors declare no conflicts of interests with respect to the present article.
Please cite this article as: Girón Moreno RM, et al. Trastornos psicológicos y calidad de vida en pacientes con bronquiectasias no relacionadas con fibrosis quística. Arch Bronconeumol. 2013;49:415–20.