In elderly seniors (>80 years), respiratory function may be compromised when, in addition to the presence of comorbidity and loss of mobility, there is also reduced respiratory muscle (RM) strength. The literature has shown that RM training could be an effective method to improve RM function and prevent clinical deterioration, particularly in population with RM weakness.
The main purpose of this paper was to assess the effectiveness of RM training on the respiratory muscle strength and endurance of institutionalized elderly women with functional impairment.
MethodFifty-four residents (mean=85 years, SD=6.7) were randomly assigned to either a control (n=27) or training (n=27) group. A supervised training program was developed with Threshold® IMT, five times per week for 6-weeks. The main variables of the intervention were: maximum inspiratory pressure (PImax), maximum expiratory pressure (PEmax) and maximal voluntary ventilation (MVV), all of which were measured at weeks 0, 4, 7 and 10.
ResultsStatistical analysis revealed no significant differences in PImax (F3,114=1.04, P=.368, R2=0.027), PEmax (F3,114=1.86, P=.14, R2=0.047) and MVV (F3,114=1.74, P=.162, R2=0.044) between the two groups after the intervention. However, the workload significantly improved with the training sessions (F5,100=72.031, P<.001, R2=0.791).
ConclusionIn a 6-week interval-based training program, the threshold loading device does not significantly improve parameters related to RM strength and endurance of the study population.
En el anciano de edad avanzada (>80 años) la función respiratoria puede verse afectada cuando a la presencia de comorbilidad y la pérdida de movilidad se suma el descenso de la fuerza de la musculatura respiratoria (MR). La literatura médica ha mostrado que el entrenamiento de la MR puede ser una intervención efectiva para mejorar la funcionalidad y prevenir el deterioro clínico, especialmente en la población con debilidad de la MR.
El objetivo del estudio fue evaluar la efectividad del entrenamiento de la MR en la fuerza y resistencia de esta musculatura, en ancianas institucionalizadas con limitación funcional.
MétodoSe asignaron aleatoriamente 54 residentes con limitación para deambular (media 85 años, DE 6,7) a un grupo control (n=27) y entrenado (n=27). Se desarrolló un programa de entrenamiento supervisado, mediante Threshold®IMT, 5 días por semana durante 6 semanas. Las variables principales fueron: la presión inspiratoria máxima (PImáx), la presión espiratoria máxima (PEmáx) y la ventilación voluntaria máxima (MVV), medidas en las semanas 0, 4, 7 y 10.
ResultadosLos análisis estadísticos no revelaron cambio en la PImáx (F3,114=1,04, p=0,368, R2=0,027), PEmáx (F3,114=1,86, p=0,14, R2=0,047) y MVV (F3,114=1,74, p=0,162, R2=0,044) entre ambos grupos tras la intervención. No obstante, la carga de trabajo mejoró significativamente con el entrenamiento (F5,100=72,031, p < 0,001, R2=0,791).
ConclusiónEl dispositivo de entrenamiento umbral en un programa interválico de 6 semanas no produce una mejora significativa de los parámetros relacionados con la fuerza y la resistencia de la MR, en la población estudiada.
One of the most important physiological changes in respiratory function that accompanies aging is the decline in respiratory muscle (RM) strength, associated with the overall loss of muscle mass or sarcopenia. In elderly seniors (>80 years), sarcopenia, as well as the presence of other diseases (comorbidities) can cause physical disability, functional deterioration1 and affect respiratory function, making it more vulnerable against disease.2 RM strength and resistance are related with the ability to move around freely and perform activities of daily living (ADL).3,4 Therefore, RM strength is an important physiological variable that helps prevent functional decline in the elderly5 and can reduce the risk for morbidity and mortality.2
Previous studies show that aerobic exercise in general is accompanied by physiological benefits, including increased RM strength and resistence.3,6,7 In addition, it seems that these benefits are greater when they are combined with specific RM training.6,7 Some elderly patients are not able to do aerobic exercise in general, and in that case specific RM training can be considered as an alternative to avoid deterioration in the most vulnerable elderly population. Recent studies emphasize the need for RM training in the elderly population with difficulty for performing overall aerobic exercise (walking, for example)5,8 and in general in the population with RM weakness,9 which are characteristics that define the population that is the object of this study.
As for the modalities for RM training, ventilation with threshold load (for example, Threshold® Inspiratory-Muscle Trainer) has been revealed to be a simple, effective method for increasing inspiratory muscle resistance and strength, regardless of the ventilatory pattern.10,11 Gosselink highlights as an additional advantage the fact that ventilation with threshold loading shortens inspiratory time and increases exhalation and relaxation time,12 which may avoid the appearance of inspiratory muscle fatigue. Several studies have demonstrated the effectiveness of Threshold® IMT, both in healthy populations as well as in those who present respiratory, cardiovascular and neuromuscular diseases. However, few studies have evaluated this type of training in elderly populations,8,13–15 and none have been done in elderly subjects with limited movement. According to Harms,16 elderly women present poorer lung function values and, therefore, greater limitation for physical activity than elderly men. In addition, women have a longer life expectancy, and consequently greater functional limitation in old age.
The objective of this study was to evaluate the effectiveness of a specific IMT program about RM strength and resistance in institutionalized elderly women with functional limitation. The general hypothesis was that the Threshold® IT equipment improves RM strength and resistance in this population.
Subjects and MethodsThe study is a randomized, controlled assay, approved by the Ethics Committee for Human Research at the University of Valencia (clinical assay no. H1325072291220). All the procedures used for measuring and respiratory training have respected the ethical principles included in the Helsinki Declaration, and informed consent was obtained.
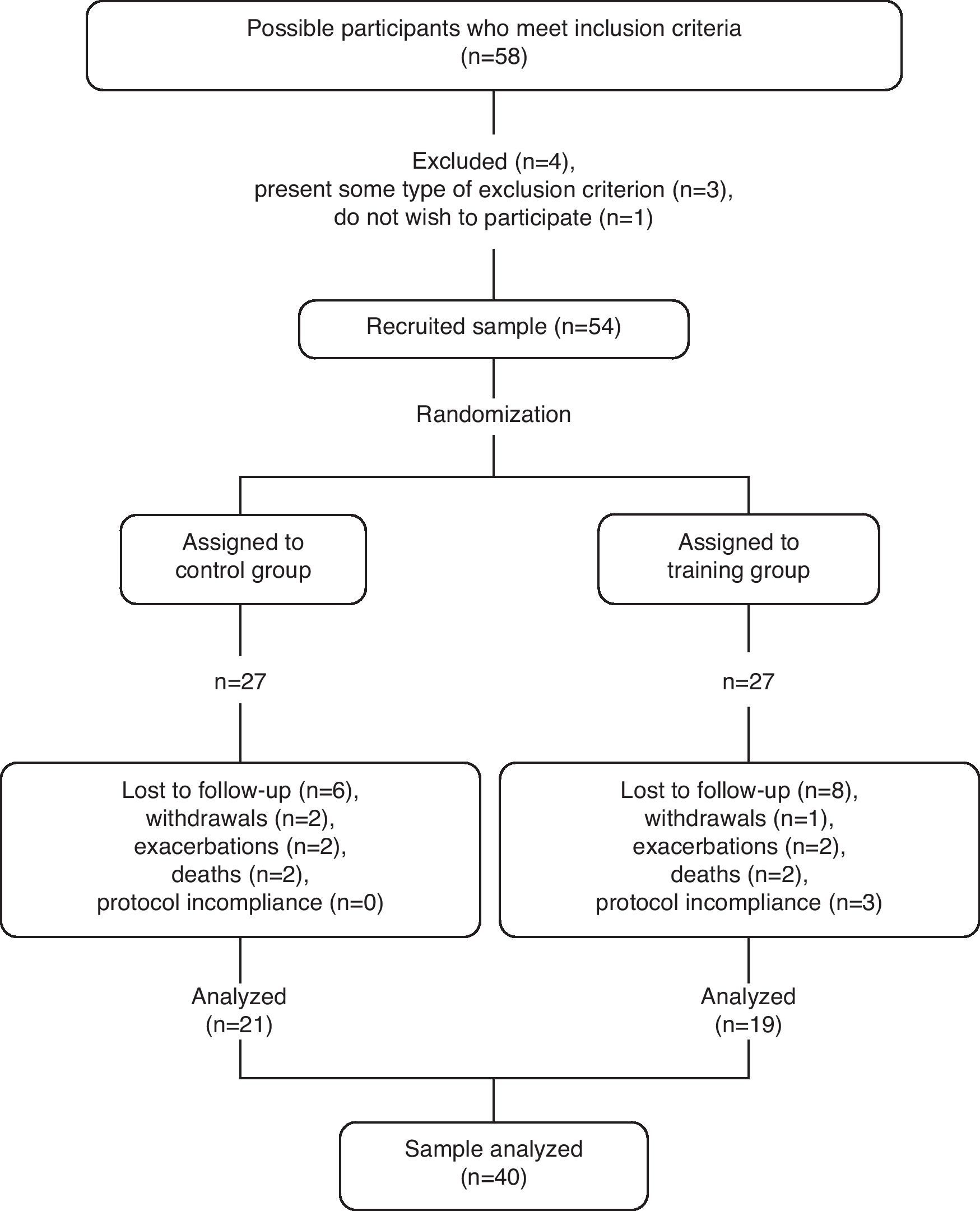
We selected 54 elderly institutionalized women (mean age 85, SD 6.7) from nursing homes located in the city of Valencia (Spain). The inclusion criteria were: (a) inability to walk more than 10m or use of wheel chair; (b) Mini Cognitive Test by Lobo score≥20 points (participants without moderate or severe cognitive deterioration); and (c) medical stability, determined by the healthcare personnel at each center. A questionnaire was completed about the medical history of the residents in order to identify any conditions that could exclude them, such as: (a) chronic cardiorespiratory problems; (b) acute cardiorespiratory episode (in the 2 previous months); (c) neurological, muscular or neuromuscular problems that could interfere with performing assessment tests and/or physical training; (d) active smokers or ex-smokers (<5 years); and (e) terminal patients. Throughout the 3 months of 2009, which was the time period of the study, 14 residents were lost to the study for different reasons, resulting in a total of 40 participants (Fig. 1).
MeasurementsBoth groups, the control group (CG) and the training group (TG), were measured at 4 different moments: baseline (time 0); midway through the training program (week 4); end of training program (week 7); and follow-up (week 10). The main variables were: maximum inspiratory pressure (PImax), maximum expiratory pressure (PEmax) and maximum voluntary ventilation (MVV).
SpirometryLung function was assessed with a portable spirometer by Jaeger (VIASYS® Healthcare GmbBH, Höchberg, Germany). The tests were simple spirometry (volume-time) and forced spirometry (flow-volume curve), which provided data for the following variables: vital capacity (VC), forced vital capacity (FVC), forced expiratory volume in one second (FEV1), peak inspiratory flow (PIF), and peak expiratory flow (PEF). For both tests, we followed the standards required by the American Thoracic Society and the European Respiratory Society (ATS/ERS).17 In the case of forced spirometry, this was repeated until it obtained a minimum of 3 technically satisfactory maneuvers, with a minute of rest in between, and the highest and most reproducible value was recorded, as long as the difference of the 2 highest values, FEV1 and FVC, were not >0.150 l (ATS/ERS, 2005: p. 325).17
Respiratory Muscle StrengthPImax and PEmax were measured with an aneroid manometer (Series 2000 Magnehelic® Pressure Gauge, Dwyer Instruments, Michigan City, Indiana, United States) with a sensitivity range between 0 and 300cm H2O of pressure. The measurements were repeated until 3 readings were obtained with a variance ≤10%,18,19 and the highest value was used. The reference values used to obtain the percentages were those chosen by Enright et al.,19 taking into account the following circumstances: (a) the values for normalcy included the population ≥85, with a sample size higher than that of other studies (n=193), and excluded the institutionalized population and/or those who were unable to walk; and (b) the present study reproduces the methodology developed by these authors, following the indications of Black and Hyatt.20
Respiratory Muscle ResistanceMVV (maximum volume of air that a person breathes voluntarily during an interval of 12s) was measured a minimum of 2 times with a variation ≤20%.17,21 MVV diminished progressively with weak and fatigable RM. In accordance with the ATS/ERS, MVV is an index that is representative of overall RM resistance: “The most important advantage to measuring MVV as an indicator of respiratory muscle endurance is its close resemblance to the task performed during exercise.” (ATS/ERS, 2002, p. 563).18 The reference values used to obtain the percentages were those published by Neder et al.21 All spirometry measurements, as well as PImax, PEmax and MVV, were done by specialized personnel, and with the participants sitting and wearing nasal clips.17,18
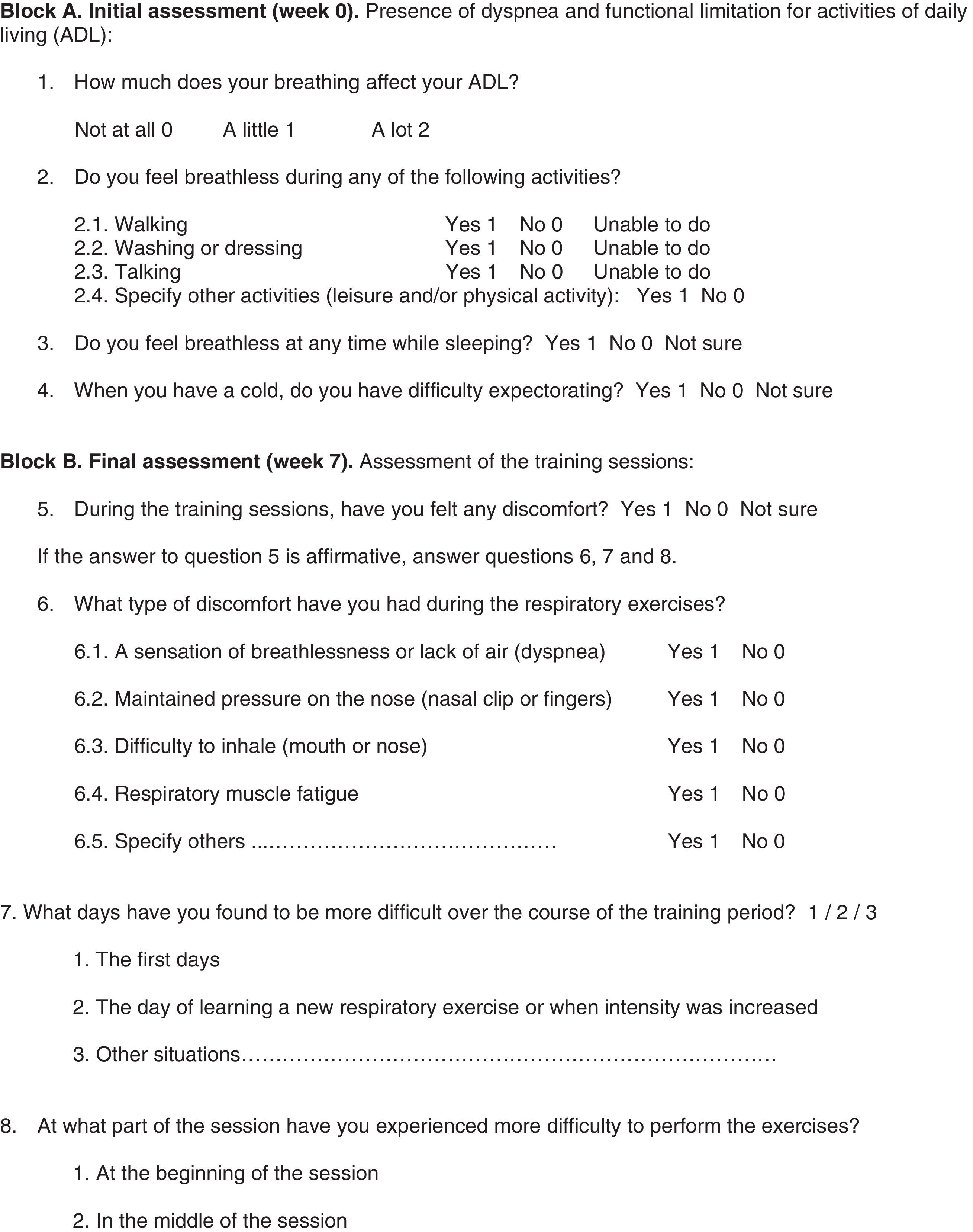
Ad hoc QuestionnaireThe research team and several experts (physicians specialized in geriatrics and pulmonology, physiotherapists and psychologists) elaborated a questionnaire (Appendix A) that allowed us to know: (a) the presence of dyspnea and functional limitation for ADL; (b) the experience during the training sessions; and (c) observations about the training protocol. The members of the research team that carried out the survey were not involved in the development of the training protocol. During the initial assessment, both groups responded to questions 1–4. Later, in the post-training assessment (week 7), only the TG answered questions 5–15. It is an ad hoc questionnaire created for the purpose of this study alone, with descriptive purpose and content validity, because the Spanish versions of the validated scales did not adjust to the characteristics of the population studied.
Inspiratory Muscle Training ProgramThe RM training program was carried out with the Threshold® IT device (Respironics Health Scan Inc., Cedar Grove, NJ, United States). It is a device that is able to work against a threshold load that is adjustable between 7 and 41cm H2O of negative pressure. Physiotherapists who were not involved in the measurements supervised the 5 weekly sessions for 6 consecutive weeks. The interval of the training program consisted of 7 alternating cycles of 2min of work and 1min of rest.22 The initial days of the first week of training were dedicated to the familiarization of the participants with the training process, and low workloads of 7–10cm H2O were used. Afterwards, the workload was increased, taking into consideration the tolerance to exertion of each participant, while inspiring against a load of between 30% and 50% of the baseline values of PImax, during the first 3 weeks of training. In order to ensure that each participant was subjected to the appropriate workload, the intermediate measurement of PImax allowed us to calculate the load at which each subject should train the 3 remaining weeks. Thus, the load was readjusted between 30% and 50% of intermediate PImax, and it was adequately increased between weeks 4 and 6. Throughout the 6 weeks of training, all patients were controlled for percentage of oxygen saturation (SaO2) and heart rate (beats/min), at least once a week during the interval program. Data were collected daily for inspiratory workload (cm H2O), subjective perception of exertion (Borg CR10 scale)23 and compliance with the session, and the reasons for any absences were recorded. The CG did not train, but were merely measured at the same time intervals (weeks 0, 4, 7, and 10).
Statistical AnalysisThe statistical data analysis was done with the SPSS version 20 computer program. The descriptive statistics were calculated for all the variables, means, standard deviations and percentages. We used the statistical and graphic techniques recommended in the medical literature to evaluate assumptions (normalcy, homoscedasticity, etc.) as well as atypical values. In order to calculate the sample size, a priori, from a statistical standpoint, it is necessary to have a size for the estimated reasonable effect. In this case, there were no studies with conditions that were even similar to the population being studied in this randomized clinical assay. Therefore, it was not possible to make a reliable statistical estimation. We then turned to the medical literature to assess the typical sample size at which significant effects begin to be shown with the technique. Based on those studies,6,7,10,11,14 we opted for a larger sample size that therefore had greater statistical power than the studies for the same effect size. Additionally, inferential techniques were used (t and chi-squared tests) to compare both groups at baseline, as well as mixed ANOVA 2 (group)×4 (time) to analyze the effects of the intervention with threshold versus control. Mixed ANOVA is the recommended statistical method for assessing the evolution of groups (trained and control) at several moments in time. Post hoc tests were calculated for statistically significant differences with the Bonferroni correction, as well as estimations of the magnitude of the effect with the determination coefficient.
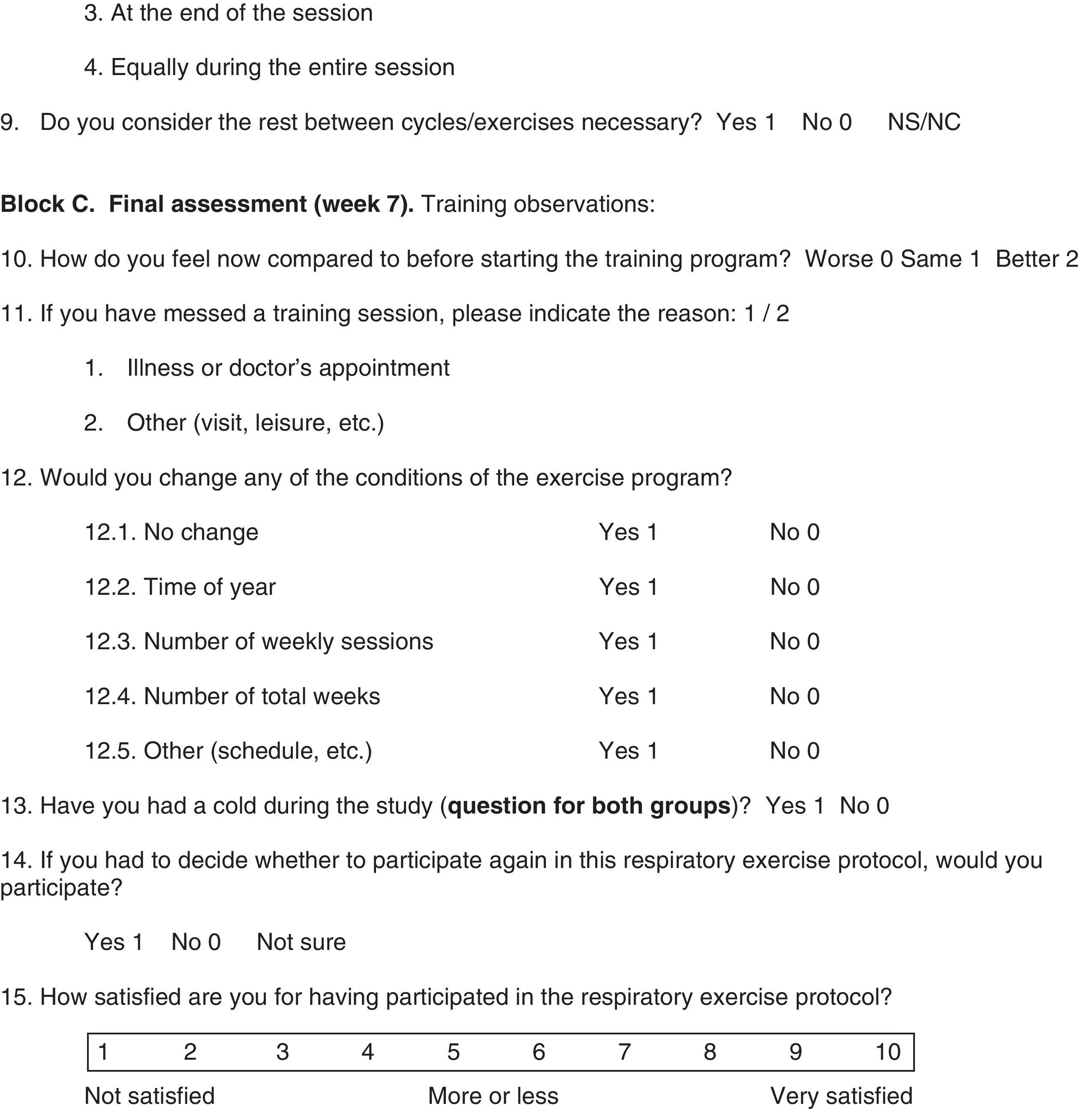
ResultsDescriptive VariablesBaseline CharacteristicsTable 1 shows the baseline characteristics and the homogeneity tests between groups. As for the anthropometric data, the results only show that the groups differ in height.
Baseline Characteristics of the Participants From Both Groups Studied: Percentages or Means±1 Standard Deviation.
| Variable | Control Group (n=21) | Training Group (n=19) | P |
| Anthropometric data | |||
| Age, years | 86.2±5.0 | 84.6±7.7 | .421 |
| Height, cm | 147.3±5.3 | 153.6±6.4 | .002 |
| Weight, kg | 63.5±11.6 | 66.6±15.3 | .478 |
| BMI, kg/m2 | 29.3±5.1 | 28.2±5.8 | .507 |
| Diagnosed diseases | |||
| Respiratory, % yes | 28.6 | 36.8 | .577 |
| Cardiovascular, % yes | 76.2 | 57.9 | .217 |
| Endocrine, % yes | 39.0 | 42.1 | .796 |
| Neurological, % yes | 28.6 | 36.8 | .577 |
| Muscular-skeletal, % yes | 76.2 | 63.2 | .369 |
| Other, % yes | 76.2 | 84.2 | .527 |
| Comorbidity, n | 3.24±1.0 | 3.21±1.1 | .935a |
| Pulmonary function | |||
| VC, l | 1.50±0.33 | 1.67±0.46 | .075 |
| VC, % pred. | 77.7±18.5 | 83.0±21.3 | .450 |
| FVC, l | 1.36±0.34 | 1.54±0.42 | .138 |
| FVC, % pred. | 72.9±20.6 | 76.1±20.0 | .656 |
| FEV1, l | 1.11±0.33 | 1.19±0.38 | .456 |
| FEV1, % pred. | 81.8±26.6 | 80.0±25.7 | .848 |
| FEV1/FVC, % | 80.6±10.8 | 77.1±12.2 | .347 |
| PEF, l/s | 2.58±1.0 | 2.75±1.12 | .618 |
| PIF, l/s | 1.78±0.54 | 1.64±0.48 | .404 |
| Respiratory muscle function | |||
| PEmax, cm H2O | 48.6±18.2 | 54.5±23.0 | .372 |
| PEmax, % pred.b | 53.7±21.1 | 58.3±26.8 | .549 |
| PImax, cm H2O | −28.1±13.8 | −29.5±11.4 | .734 |
| PImax, % pred.b | 66.4±30.4 | 67.9±26.2 | .873 |
| MVV, l/min | 28.9±13.2 | 31.1±10.7 | .574 |
| MVV, % pred.c | 33.5±9.9 | 40.1±14.5 | .604 |
FEV1, forced expiratory volume in one second; FVC, forced vital capacity; BMI, body mass index; MVV, maximum voluntary ventilation; PEF, peak expiratory flow; PEmax, maximum expiratory pressure; PIF, peak inspiratory flow; PImax, maximum inspiratory pressure; % pred., percentages of reference values; VC, vital capacity.
The section “diagnosed diseases (DD)” shows the percentages of DD presence and the mean number of DD (comorbidity).
Percentage according to the reference values of Neder et al.21; as for these reference values for MVV, it should be kept in mind that only 15% of the sample was analyzed (<80 years; for those with reference values). The Student's t and chi-squared tests were used to obtain the differences between the two groups.
No statistically significant differences were observed in the variables regarding inclusion criteria: the Lobo Mini Cognitive Test (23.0±3.5) and Barthel index (68.1±22.7). On an average, the participants had been institutionalized 4.1±5.2 years and only 12.5% were ex-smokers (CG, n=1; TG, n=4; P=.120).
As for questions 1–4 (Appendix A, block A) of the ad hoc questionnaire, there were no significant differences between the 2 groups (P>.05). In 37.5% of the cases, breathing affected in some measure (“a little” or “a lot”) the normal development of activities of daily living (ADL). Among these, walking and/or transference were mostly associated with the presence of dyspnea (47.5%), followed by self-care activities (27.5%). The main causes that impede walking were: amputation of a lower limb or limbs, the effects of a cerebrovascular accident, osteoarthritis and a history of fractures caused by falls.
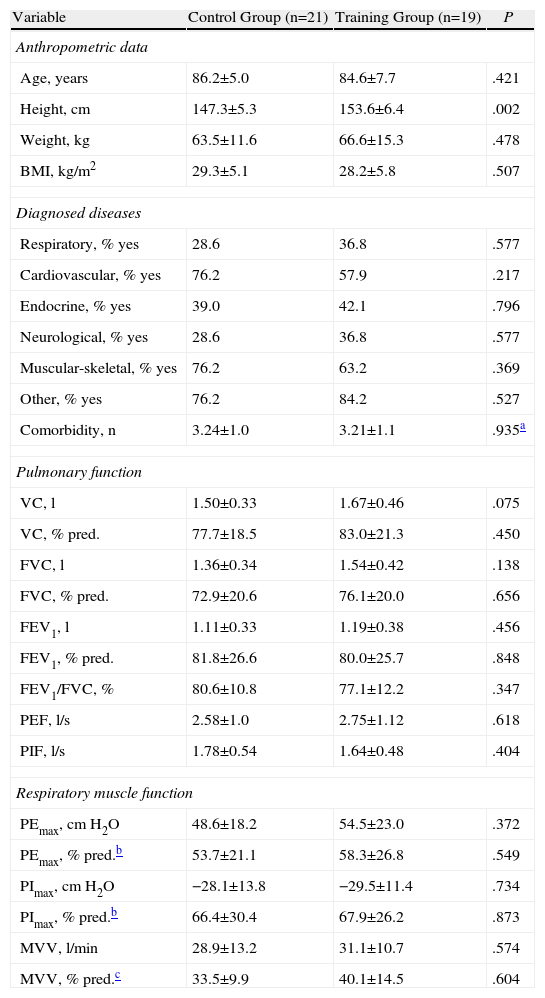
Assessment of the Training ProtocolThe descriptive analysis corresponding with questions 5–9 (Appendix A, block B) of the ad hoc questionnaire for the TG shows that close to 42.7% of the participants reported difficulty in breathing during the session, especially for the first few days (47.4%) and when the workload was increased (15.8%). They also considered the 1-min rest intervals (84.2%) necessary. After the conclusion of the training protocol (questions 10–15, Appendix A, block C), 63% of the participants perceived an improvement over their previous state, and 57.9% considered it necessary to make some type of change in the protocol (for example, 47.4% period of one year; 21.1%, weekly sessions; 22%, total number of weeks). As for the number of colds, there were no significant differences (CG 33.3% and TG 52.6%; P=.218). 84.2% of the people with training answered that they would participate again, while 5.3% did not know what to answer. In addition, they scored an average perceived satisfaction of 8.4±2.1 on a scale from 1 (“not at all satisfied”) to 10 (“very satisfied”). Finally, the subjective perception of exertion (Borg CR10 scale)23 for the TG showed no significant differences between the weekly averages (Table 2), and a score of 3 was “moderate” exertion.
Subjective Perception of Exertion for the Participants of the Training Group: Mean±1 Standard Deviation.
| Borg scale CR10 | Training Group (n=19) |
| Week 1 (max. 10) | 3.45±1.18 |
| Week 2 (max. 10) | 3.32±0.79 |
| Week 3 (max. 10) | 3.18±1.06 |
| Week 4 (max. 10) | 3.57±3.14 |
| Week 5 (max. 10) | 3.10±0.98 |
| Week 6 (max. 10) | 3.00±0.86 |
| Week 1–6 (max. 10) | 3.17±0.86 |
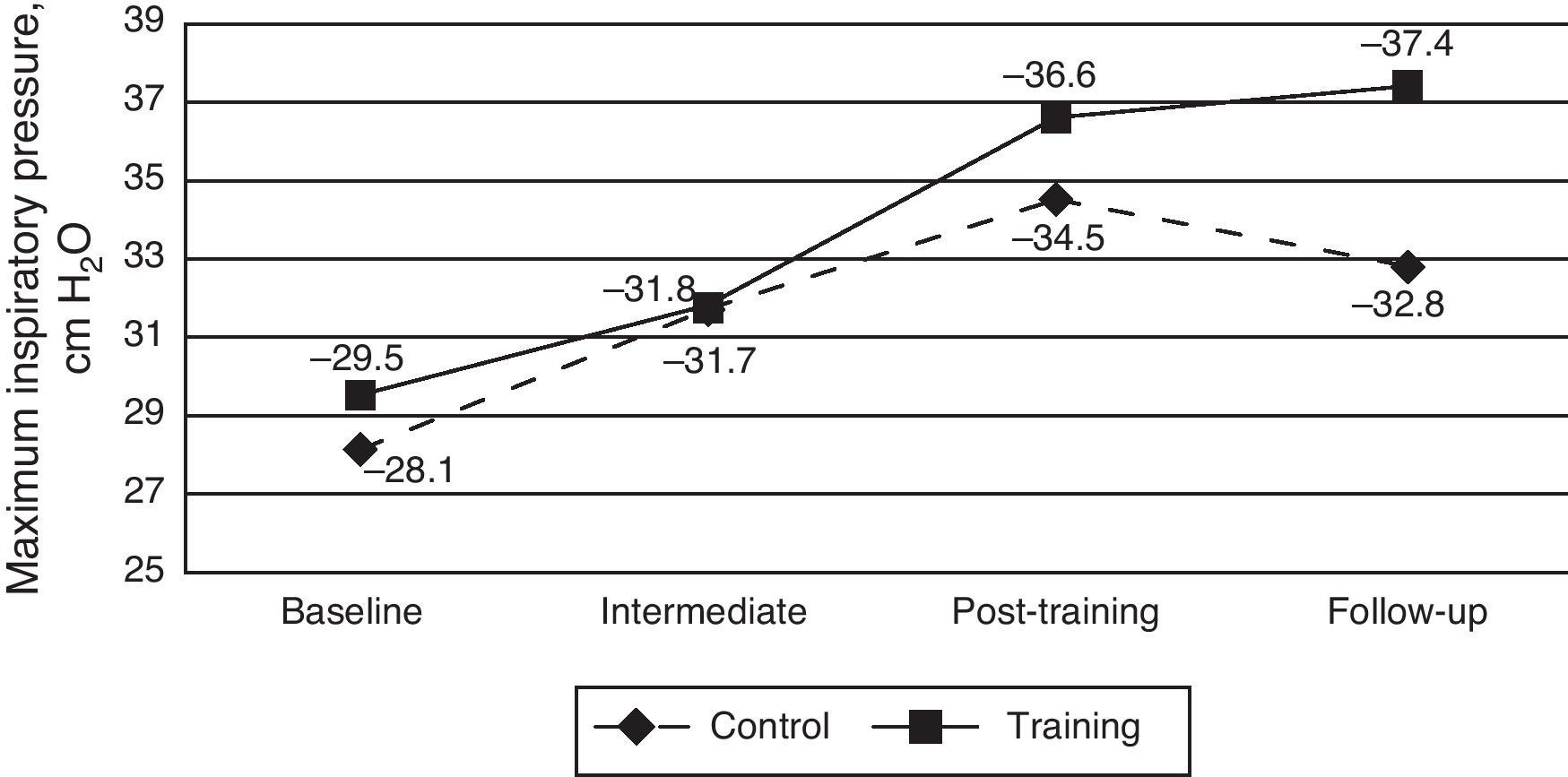
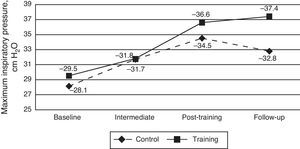
The estimated ANOVA evaluating the effect of the intervention on the absolute PImax values did not find statistically significant differences among the groups (F1,38=0.22, P=.637; R2=0.006). Time did show differences and in both groups there was an increase over time (F3,114=12.51, P<.001, R2=0.248). However, the interaction effect, which shows if the treatment is effective, was not statistically significant (F3,114=1.04, P=.368; R2=0.027) (Fig. 2). Although the interaction was not statistically significant, simple effects analyses of the interaction were used to better understand within each group what moments in time differed. The CG showed differences between the baseline and the final measurement (time period 3 or post-training, P<.05). Contrarily, the TG presented differences at all time periods with baseline (P<.05). There were no differences between time periods 3 and 4 (follow-up) (P>.05). This result indicates that the change over time in the TG was more stable, as CG is lower in the follow-up, which does not happen in the TG.
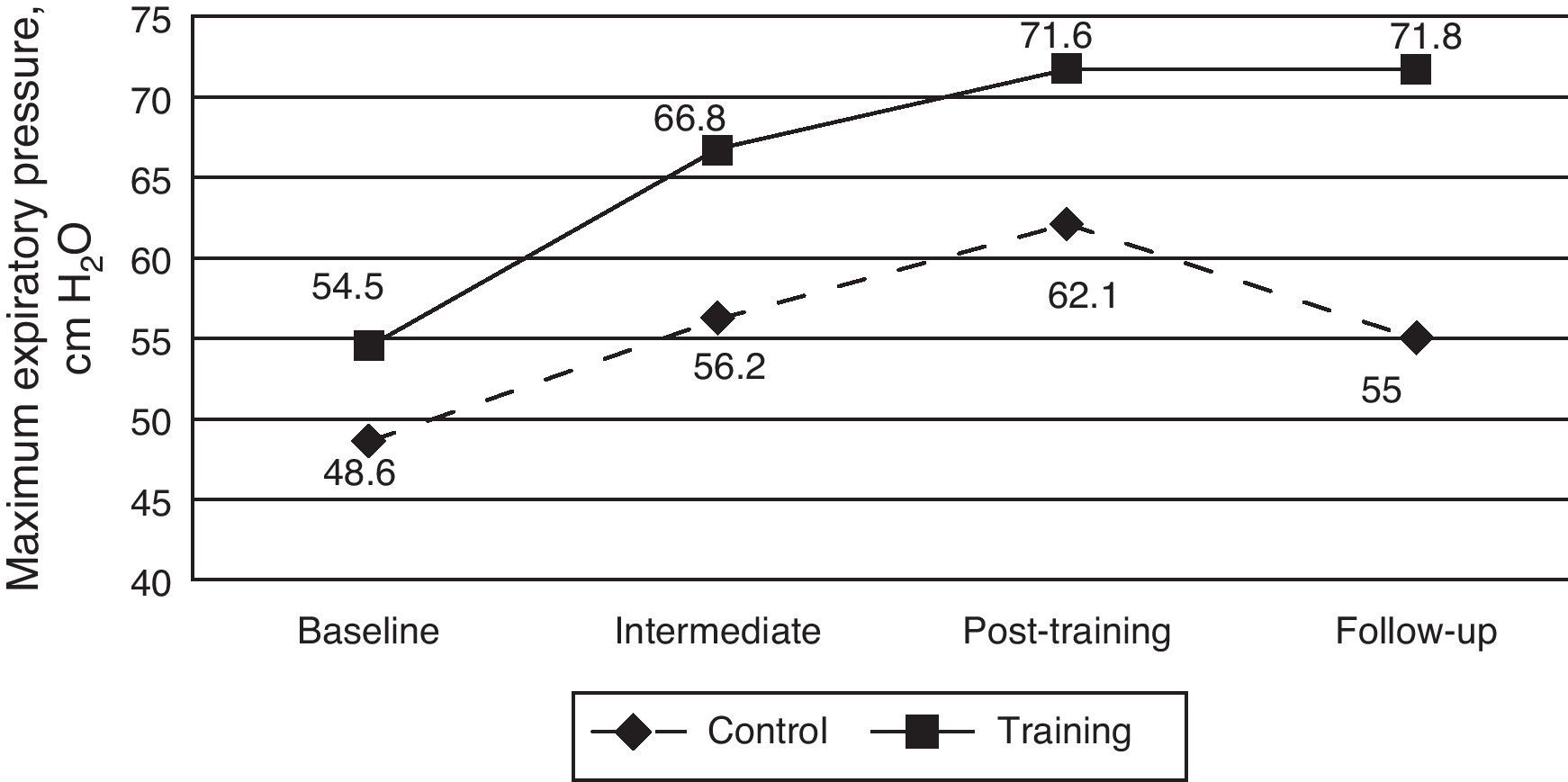
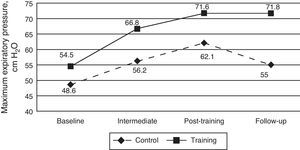
Expiratory Muscle StrengthThe estimated ANOVA assessing the effect of the intervention on the absolute PEmax values also found no significant differences between the groups (F1,38=2.57, P=.117; R2=0.063). Time did show significant differences and in both groups there was an increase over time (F3,114=15.55, P<.001, R2=0.29). However, the interaction effect was not statistically significant in the case of PEmax (F3,114=1.86, P=.14; R2=0.047) (Fig. 3). Although the interaction was not statistically significant, simple effects were done as in the former variable. In the case of CG, there was only a gain between the baseline and the post-training and, however the follow-up did not differ significantly from baseline (P>.05). In the case of TG, baseline differed from all the other time periods (P>.05), which indicated a stable change, even in follow-up.
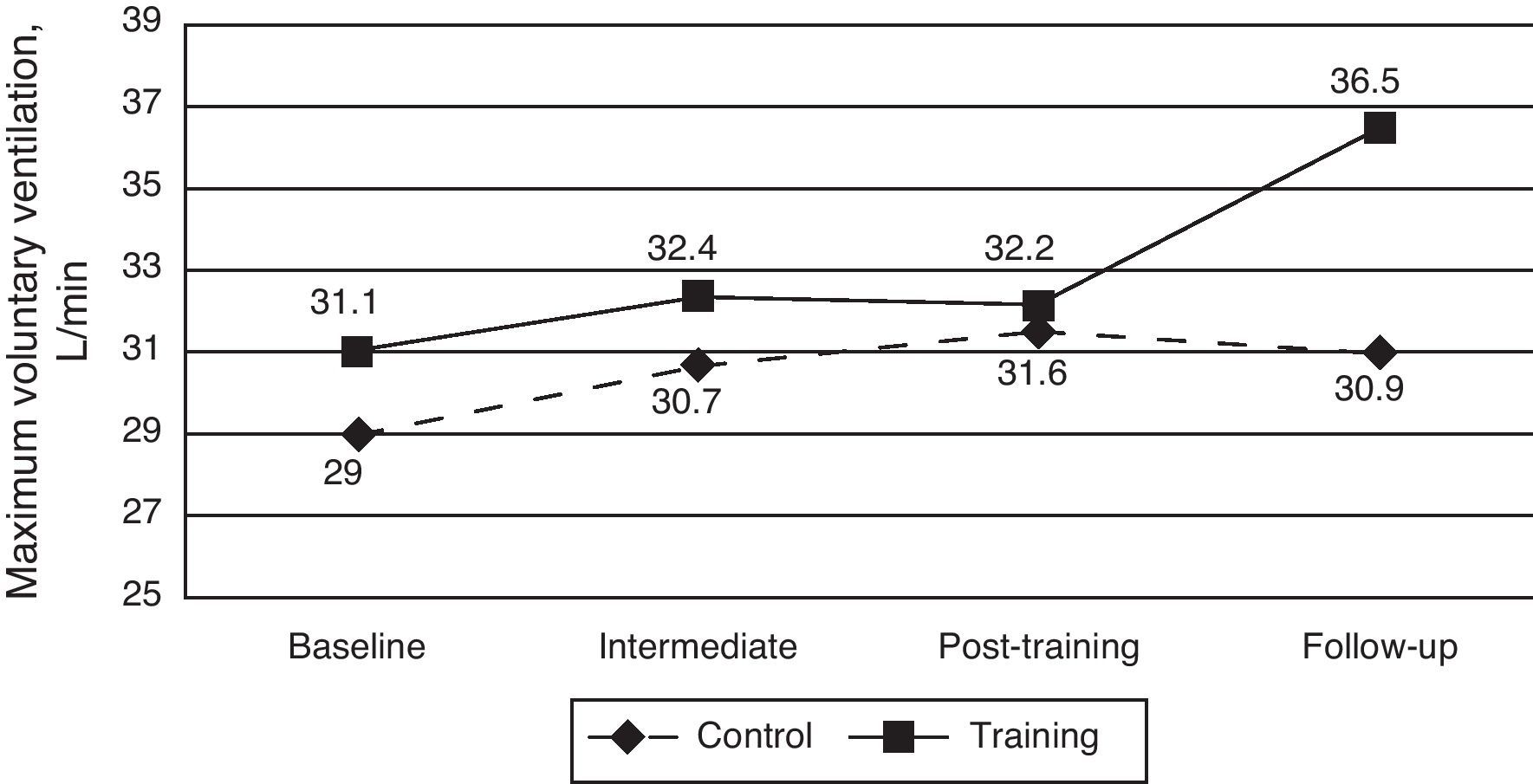
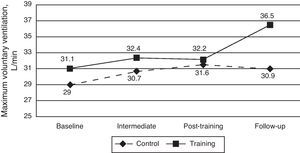
Respiratory Muscle ResistanceA third ANOVA evaluated the effect of the intervention on the absolute MVV values and, once again, did not show significant differences between the groups (F1,38=0.47, P=.49; R2=0.012). There was a significant increase in MVV over time (F3,114=3.39, P=.02; R2=0.082), despite the fact that the interaction was not significant (F3,114=1.74, P=.162; R2=0.044) (Fig. 4). Once again, and although the interaction was not statistically significant, simple effects were done. In the case of CG, there were no differences between any of the time periods (P>.05), which indicate stability in the resistance of RM. In the case of TG, the baseline differed only from the follow-up (P<.05), which indicates that, if there were potential effects of training with Threshold® IT on muscle resistance, these tended to appear at later time periods.
Threshold® IT: Workload and Subjective Perception of ExertionThe workload that the TG group was subjected to significantly improved both absolute values (F5,100=72.031, P<.001; R2=0.791) as well as percentage of baseline PImax (F5,100=67.225, P<.001; R2=0.810). In absolute values, the load increased from −9.7 to −20.7cm H2O over the course of the 6-week training period. This increase was considerably less during the first half of the RM training (difference of means between the first and third weeks, 3.39cm H2O) than during the second half (difference of means between the fourth and sixth weeks, 5.84cm H2O), a result that may be due to the period of familiarization of the first week. Likewise, the relative workload rose from 36% to 78% PImax measured at baseline. The difference of percentages for the first half of the training period was 11%, while for the second half it was 23.3%, an aspect possibly related with familiarization, as previously commented. Last of all, the subjective perception of exertion (Borg scale) did not change (P>.05) during the training period (Table 2).
DiscussionIn this present study, training with the Threshold® IT device did not reveal a significant improvement in RM strength or resistance between the two groups. These results were unexpected because the majority of previous studies in other populations demonstrate the positive experimental effect of the use of the IT device,10 especially in patients with RM weakness.9 In the elderly population, previous controlled clinical assays show that RM strength and resistance,8,13 as well as functional autonomy,15 improve with specific RM training. Nonetheless, our study differs from the previously mentioned studies in several aspects, making a strict comparison difficult: (a) the mean age of the sample was younger (67–70 vs 85)8,13,15; (b) the specific RM training modality did not include the Threshold® IT device (isocapnic hyperventilation,13 Powerlung® inspiratory and expiratory threshold load device8), except for the study by Fonseca et al.15; and (c) the capacity for exercise was normal and/or community lifestyle,8,14 except for the institutionalized population in the Fonseca et al. study.15 In our study, the elderly subjects presented inability to walk and accentuated RM weakness (age range 80–97; PImax baseline −28.8cm H2O and PEmax baseline 51.4cm H2O), particularities that could explain the difference in our results compared with those of Watsford and Murphy8 (age range 60–69; PImax baseline between −70 and 80cm H2O and PEmax between 80 and 90cm H2O).
Although there was no statistical significance between the groups for the main variables, there was an observed increase of 30% in the PImax for the TG between the start and end of the intervention. Although there was also an observed gain in PImax (18%) in the CG, this was substantially lower when we analyze the progression of the PImax values between the start and the end of the intervention, which indicates that the improvement observed in the CG was not due to physiological factors, since this group had not been training. In line with these results, O’Kroy and Coast24 found a significant increase in PImax in the CG. Hill et al.22 also found an increase of 8% in PImax in the CG, although this increase was lower than that found in the TG (29%), in spite of which the difference was statistically significant. Analyzing these studies in greater detail, we observed that the intervention by O’Kroy and Coast24 consisted of a continuous training protocol in healthy persons and in the case of Hill et al.22 the training protocol was interval-based, but in patients with chronic obstructive pulmonary disease. Once again, the anthropometric characteristics and health of our sample can offer a plausible explanation to the lack of effectiveness of the IT device: institutionalization, presence of comorbidity, inability to walk and RM weakness (according to Simões et al.,25 maximum respiratory pressures are considerably low in institutionalized seniors, PImax from −44.5 and 33.06cm H2O and PEmax between 41.94 and 34.78cm H2O). Another possible explanation for the increase in PImax and PEmax in the CG could be the learning effect of the maneuvers for measuring maximum respiratory pressures described by Larson et al.11
As for the non-significant improvement observed in PEmax, we can mention that, although the threshold device (Threshold® IT) was designed for training inspiratory muscles, it is possible that the expiratory muscles are also involved, as argued by Breslin.26 In the recent study by Barbalho-Moulim et al.27 there was also an observed non-significant increase in PEmax (26%) after a training protocol with Threshold® IT (15min per session, 6 sessions per week, for 2–4 weeks). In this study, the population studied was different from the present study, especially concerning RM weakness and the mean age of the population. Therefore, we did not have available any similar studies with which to compare our results.
Furthermore, the workload that the TG was subjected to increased over time and can partially explain the values and the improvement observed for PImax, PEmax and MVV between the post-training and follow-up measurements (Figs. 2–4). The increase in workload seen in the TG from post-training to follow-up can be explained as a maintained effect of the training, which did not appear in the CG. In addition, the perception of the exertion did not change during the 6-week period. In this regard, it is interesting to mention that, although there was not a significant increase in PImax compared with CG, the effect of the intervention was perceived by the trained participants as they were able to train at significantly greater loads with a similar level of exertion.
Study Limitations and StrengthsBased on the low values of the maximum respiratory pressures, 6 weeks of training may be too short of a time to observe a substantial effect of training in elderly women with important functional limitations. The Respiratory Rehabilitation Guidelines28 recommend longer training periods (between 6 and 12 weeks) and indicate that 12 or more weeks of intervention tend to produce a greater maintained benefit. Although the training protocol that has been used in this study is similar to that proposed by Hill et al.,9 several circumstances motivated the change in the duration and frequency of sessions of the protocol developed: (a) the presence of comorbidity and high rate of mortality; and (b) the passivity of institutionalized elderly subjects.
The limitations mentioned indicate the need for future research that demonstrates the effectiveness of the Threshold® IT in the weakest elderly populations. Future studies should include longer training periods, other possible modalities for specific RM training, as well as the placebo group, in order to be able to measure the effects of training and avoid the possible influence of learning. Therefore we believe it is convenient to include other measures that are potentially relevant, like the effect on capacity for exertion and improved dyspnea and quality of life, through questionnaires that have been validated for this population.
To our knowledge, this is the first study in an elderly institutionalized population, with functional deterioration and muscle weakness, that has applied a specific RM training protocol. The novelty and importance of this clinical assay lies in certain aspects, such as: (a) mean age (85±6), which is 10–15 years older than the mean age of previous studies; (b) the use of Threshold® IT; (c) the measurement of PImax, PEmax and MVV at 4 time intervals, unlike previous research measuring only at pre- and post-intervention11,13; and (d) the sample size larger than that used in previous studies (n=5–17), both in adults and the elderly, in healthy persons as well as ill patients. Last of all, this study indicates the importance of respiratory intervention and points out the difficulties for studying such a population.
Clinical RelevanceStudies of this type offer health-care professionals the opportunity to widen their understanding through an intervention in a growing collective that to date has not been extensively studied: the elderly. Furthermore, the results found in this collective in particular could be generalized to other collectives with different ages but similar health conditions. Therefore, we are promoting a greater understanding of non-invasive treatments that could be applied in populations with comorbidity and an important degree of dependence.
In conclusion, we can state that the use of the Threshold® IT device in an interval-based 6-week training program does not produce a significant improvement in the parameters related with RM strength and resistance in elderly women with muscle weakness and important functional limitation.
FundingThis study has been partially funded by research grant PSI2010-21334.
Conflict of InterestsThe authors declare having no conflict of interests.
The authors would like to thank all the participating seniors for their collaboration. We would also like to show our most sincere thanks to all the physiotherapists who have supervised the training protocol, especially José Moret Vilar. Last of all, we would like to thank the socio-sanitary personnel from the participating nursing homes for their availability and advice: Ballesol-Valencia and El Amparo de Quart de Poblet (Valencia) nursing homes.
Please cite this article as: Cebrià i Iranzo MÀ, et al. Intervención fisioterápica preventiva del deterioro de la musculatura respiratoria en ancianas institucionalizadas con limitación funcional. Arch Bronconeumol. 2012;49:1–9.