The demand for resection of small lung nodules with video-assisted thoracic surgery (VATS) is growing, driven by the increasingly common indication of lung metastasectomy in selected patients and by the rise in detection rates of suspicious lung nodules on low-dose computed tomography (CT) of the chest in lung cancer screening programs.1–3 However, thoracoscopic resection of lung nodules can be difficult, since many of these small nodules are neither visible nor palpable during VATS.4 In recent years, several techniques have been described for the image-guided preoperative marking of lung nodules that can be used for the safe resection of small lung nodules with VATS techniques.5 We report the case of a patient with 2 contiguous pulmonary metastases that were marked preoperatively with a single marker released in an equidistant position between the 2 nodules.
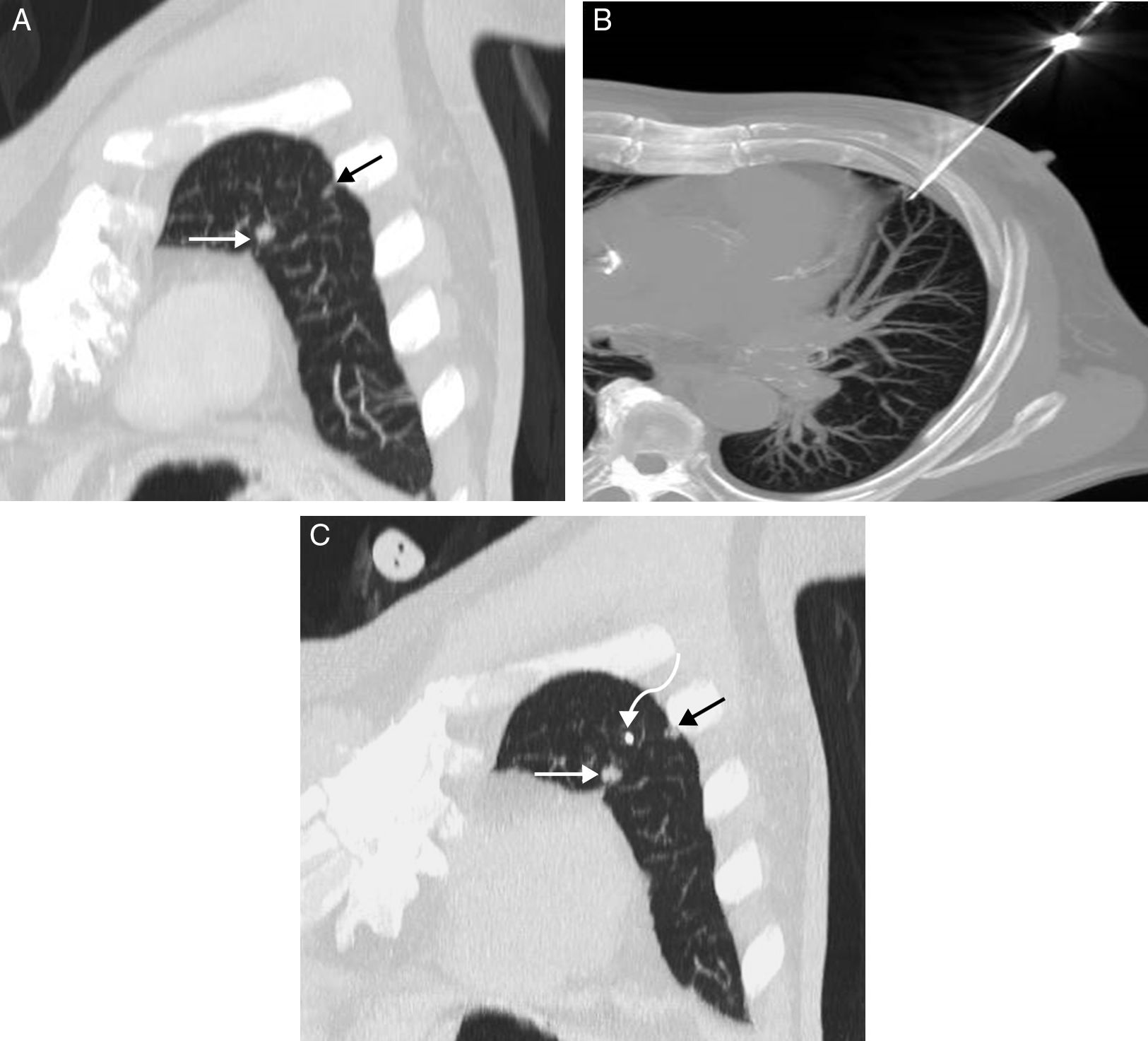
This was a 65-year-old patient with rectal cancer, in whom pulmonary metastases were detected on radiological monitoring of his disease. After adjuvant treatment with chemotherapy, the lung nodules disappeared, with the exception of 2 small pseudonodular opacities measuring less than 1cm in the left upper lobe, only 22mm apart (Fig. 1A). A multidisciplinary committee decided to perform image-guided percutaneous marking for subsequent resection by VATS. The initially agreed procedure was to place 2 markers (1 for each pseudonodular opacity) under CT guidance. However, given the relative proximity of the 2 pulmonary opacities and the possibility of causing pneumothorax after placement of the first marker that would prevent the release of the second, we decided to place a single marker (a low-radiation radioactive I-125 seed) equidistant between the 2 lesions. The percutaneous release of the marker was uneventful, and the seed was deposited at a distance of 11mm from each nodule (Fig. 1B and C). One week later, the patient underwent CT-guided VATS, and both lesions were successfully removed with a pulmonary wedge resection.
(A) MIP (maximum intensity projection) oblique coronal CT image of the chest in which 2 small opacities measuring <1cm are seen in the left upper lobe: a larger (white arrow) and another smaller lesion (black arrow). (B) MIP axial CT image of the chest showing the moment in which the seed was released from the 18G trocar needle. (C) MIP oblique coronal CT image of the chest confirming the correct equidistant placement of the I-125 seed (curved arrow) between the 2 lung lesions (straight arrows).
Resection of small pulmonary nodules by VATS can be difficult if the nodules are not visible or palpable.4 The most common CT-guided marking techniques or preoperative localization procedures of small lung nodules include the use of hook wires (the most widely used), and localization with the release of metal coils and fiducials.5 Other marking techniques consist of the intrapulmonary injection of various dyes, such as methylene blue or indocyanine green (pulmonary “tattoos”), the use of intraoperative ultrasound, or the intrapulmonary injection of radio-opaque substances (such as barium sulfate or lipiodol).6 Another, less explored technique involves marking the pulmonary lesion with low-radiation radio-labelled I-125 seeds, which can be detected intraoperatively with the use of gamma probes.7 The gamma probe inserted into the chest cavity detects the radioactivity emitted by the seed, which can then be located during the surgical procedure, and the adjacent pulmonary nodules can be resected. The main advantages of this technique over other forms of pulmonary marking are that the seed does not dislocate after placement in the lung, and the VATS can be planned days or weeks after the marking procedure: surgery does not have to be perform hours afterwards, as is the case with hook wires.7 An additional advantage of this marking technique is that the seeds used in our hospital are sourced from the surplus of seeds used for brachytherapy treatment in prostate cancer, so the cost of this marking material is practically zero; once the radioactivity of these seeds falls to less than 150 microcuries, they are used for the percutaneous marking of malignant lesions. In our case, given the proximity of the 2 lung nodules (22mm), we decided to release a single seed at a point equidistant between both lesions instead of placing 2 seeds. The sequential placement of 2 seeds would have significantly increased not only the time of the invasive procedure but, in particular, the risk of pneumothorax; indeed, the development of pneumothorax after marking the first lesion would have ruled out the release of the second seed. Moreover, in the case of our patient, the sequential resection of 2 pulmonary wedges would have been less beneficial (from the point of view of the volume of healthy lung tissue removed) than a single wedge that included both small nodules.
We found no mention in the literature of the percutaneous marking of 2 contiguous pulmonary metastases using this “equidistant” approach with a single seed. We believe that this approach in patients with contiguous pulmonary nodules not only speeds up the process of preoperative localization, but also minimizes the risk of pneumothorax and limits the volume of healthy lung tissue removed.
Please cite this article as: Gorospe-Sarasúa L, Eugenia-Rioja M, Ajuria-Illarramendi O, Cabañero-Sánchez A. Marcaje percutáneo de 2 metástasis pulmonares con una única semilla equidistante. Arch Bronconeumol. 2019;55:50–51.