Noninvasive ventilation (NIV) during hospitalization for acute hypercapnic exacerbations of chronic obstructive pulmonary disease (COPD) has been shown to be effective, but data on the prognosis of such patients is limited. The aim of this study was to investigate in-hospital and long-term outcome in patients with COPD exacerbations requiring NIV treatment during hospitalization.
MethodsBetween 2011 and 2013, hospitalized subjects with hypercapnic COPD exacerbations were included in this retrospective single-center cohort study. Subjects’ clinical and laboratory data and survival status after a median of 27 months were recorded. The predictive factors of in-hospital and long-term mortality were analyzed.
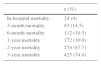
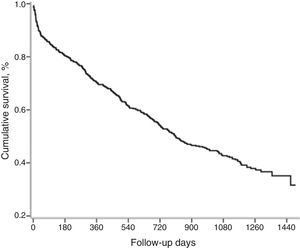
ResultsA total of 574 patients (357 men, mean age 68±11 years) were recorded. During hospitalization, 24 (4.1%) patients died. In-hospital mortality was negatively affected by lower baseline values of hematocrit, albumin, and pH, and by higher baseline leucocytes and higher 24h PaCO2. Median survival of the cohort was 27 months. Mortality at 3 and 6 months, and 1 year were 14.5%, 19.5%, and 30%, respectively. In the univariate analysis, reduction in long-term survival was found to be related to older age, higher Charlson score, lower baseline levels of hematocrit and albumin, and lower pH level after 24h. In the multivariate analysis, older age and lower albumin were identified as the strongest predictors of mortality.
ConclusionLife expectancy after a COPD exacerbation requiring NIV treatment is short. Baseline blood counts and day 2 arterial blood gases levels may predict in-hospital mortality. The strongest indicators of poorer long-term outcome were advanced age and lower albumin. Such patients may need closer follow-up.
La introducción de la ventilación no invasiva (VNI) durante las exacerbaciones agudas hipercápnicas de la enfermedad pulmonar obstructiva crónica (EPOC) en plantas de hospitalización general ha demostrado ser eficaz, pero hay escasos datos sobre el pronóstico de estos pacientes. El objetivo de este estudio fue investigar la evolución intrahospitalaria y a largo plazo de pacientes con exacerbaciones de la EPOC que requirieron terapia VNI durante su ingreso en plantas de hospitalización general.
MétodosEn este estudio de cohortes retrospectivo y unicéntrico se incluyó a pacientes con exacerbaciones hipercápnicas de la EPOC ingresados en planta entre los años 2011 y 2013. Se recabaron datos clínicos, analíticos y de supervivencia tras una mediana de 27 meses y se analizaron los factores predictivos de la mortalidad durante el ingreso y a largo plazo.
ResultadosSe registraron datos de un total de 574pacientes (357varones, edad media 68±11 años). Durante el periodo de hospitalización fallecieron 24pacientes (4,1%). Se observó que la mortalidad durante la hospitalización era mayor en los pacientes que presentaban concentraciones de hematocrito y albúmina más bajas y recuentos leucocitarios más altos en el momento del ingreso, y en aquellos con pH bajo y PaCO2 alta 24h más tarde. La mediana de tiempo de supervivencia de esta cohorte fue de 27meses. Las tasas de mortalidad a los 3 y 6meses y a un año fueron del 14,5, 19,5 y 30%, respectivamente. En el análisis univariante, se observó que la menor supervivencia a largo plazo estaba relacionada con la edad avanzada, un índice de Charlson alto y concentraciones de hematocrito y albúmina bajas en el momento del ingreso, y un pH bajo al cabo de 24h. En el análisis multivariante, los factores de predicción de la mortalidad más sólidos fueron la edad avanzada y las bajas concentraciones de albúmina.
ConclusiónTras una exacerbación de la EPOC que haya requerido VNI, la esperanza de vida es corta. El hemograma inicial y los resultados de la gasometría arterial del segundo día pueden pronosticar la mortalidad durante la hospitalización. Los indicadores más sólidos de mala evolución a largo plazo son la edad avanzada y las bajas concentraciones de albúmina. Es posible que estos pacientes requieran un seguimiento más estrecho.
Chronic obstructive pulmonary disease (COPD) is the fourth leading cause of mortality in the world and is expected to become the third leading cause of death by 2020.1,2 Acute exacerbations of COPD worsen the quality of life of sufferers and increase hospital admissions and mortality.3 One fifth of patients with exacerbations have acute hypercapnic respiratory failure (AHRF) on admission.4 In AHRF, noninvasive ventilation (NIV) has been shown to decrease complications, shorten hospital stay and reduce mortality. NIV is therefore proposed as the first line therapy in eligible patients.5–7 To date, there is no consensus as to whether it is safe to use NIV in non-intensive care units (non-ICU). Although there is no agreement on the proper location for managing these patients, NIV implementation in respiratory and general wards has proved safe and effective.8–11
There have been a number of studies on the outcome of COPD exacerbations and the prognostic factors for survival.12–17 Fewer studies have focused on the outcome of AHRF, and those that are published were mostly conducted in intensive care unit (ICU).18–21 NIV is becoming more widespread and the number of experienced staff is increasing every day.8 Only a few studies have investigated the prognosis of such patients treated specifically in non-ICU clinics,10,22,23 but prognosis has been reported to be poor with a 5-year mortality rate of 70%.22,23
This study investigated COPD patients with AHRF, hospitalized in general wards. The objective of the study was to determine predictors for in-hospital mortality, long-term outcome, and long-term survival.
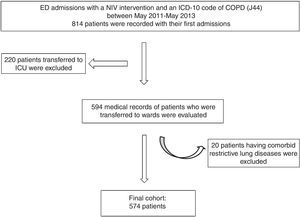
MethodsThis was a retrospective, single-center observational cohort study. Between May 2011 and May 2013, all COPD exacerbations requiring NIV treatment in the emergency department (ED) were recorded. Subjects were selected from the hospital electronic database using the ED intervention code for NIV implementation. Of those, individuals with an ICD-10 code of COPD (J44) were included. Subjects with an ICD-10 code of pneumonia (J15), interstitial lung disease (J84), and restrictive lung disease (M41) were excluded. Patients who were transferred directly to the intensive care unit (ICU) were also excluded. Cases who were admitted more than once in the study period were included only in terms of their first intervention (Fig. 1). All patients had been diagnosed with COPD by a pulmonologist who evaluated spirometry, forced expiratory volume in 1s (FEV1) of 70% predicted or less, and an FEV1 and forced vital capacity (FVC) ratio≤70%.24 Spirometry test results were not available from the patient charts.
The study was conducted in a teaching and research hospital, which is a reference center for chest diseases with the largest bed capacity (628 beds) in the country. Facilities include a third level respiratory ICU (34 beds). In the ED, pulmonologists (one chest disease specialist and two chest disease fellows) are available 24h a day. The number of patients attended in ED differs depending on the month, but an average of 100 and 250 patients are seen every day. At the time of starting the study, the department had 10 years’ experience of using NIV. All pulmonologists, chest disease fellows, ED and ward nurses attend intermittent theoretical and practical sessions on the implementation of NIV imparted by the respiratory ICU team.
In ED, the decision to implement NIV is made by the chest disease specialists, according to the clinical status and arterial blood gas levels of the subject at admission, using the following criteria: moderate or severe dyspnea, tachypnea, accessory muscle use, abdominal paradoxical respiration, arterial blood gas (ABG) pH<7.35, and partial arterial carbon dioxide pressure (PaCO2)>45mmHg.25 When the need has been determined, NIV is initiated along with oxygen supplementation, corticosteroid and bronchodilator treatment. The acute response to the treatment is evaluated within the first 2h. If clinical and ABG parameters improve, patients are transferred to general wards. Patients with worsening clinical condition or inadequate improvement are transferred to the ICU. The decision regarding ICU transfer decision is taken by pulmonologists, in consultation with ICU specialists.
In the hospital wards, in addition to their NIV, all patients receive nebulized bronchodilators, IV corticosteroids (0.5mg/kg), parenteral antibiotics (most frequently β-lactam/β-lactamase inhibitors), and supplemental oxygen. ABG levels are evaluated, and the decision on whether to continue NIV or not is made according to patients’ clinical status and laboratory test results. In the ED and wards, the modality used is BiPAP S/T-D Ventilatory Support System (Respironics, Inc. Murrysville, PA).
Data CollectionPatient demographic and clinical data were collected. Comorbidities were retrieved from medical charts and the Charlson comorbidity index was calculated for each patient.26 Current use of long-term oxygen treatment or home NIV was noted.
Baseline laboratory data included complete blood count, biochemical analysis, and ABG at admission, after 24 and 48h, and before discharge.
Patients’ survival status was extracted from government death records according to national citizenship number. Data were censored on June 10, 2015. All patients were eligible for survival analyses. In-hospital and long-term survival rates were assessed from the date of the first ED visit. The study was approved by the local Institutional Ethics Committee and the study complied with the ethical principles of the Declaration of Helsinki.
Statistical AnalysisQuantitative data are expressed as mean±standard deviation (SD) and qualitative data are expressed as frequencies. Student's t-test and chi-square tests were used to assess in-hospital mortality. All-cause mortality was reported for in-hospital and long-term ranges. Survival curves were drawn using the Kaplan–Meier method. Cox's proportional hazards model was used to determine potential predictors of mortality. Independent variables associated with respiratory mortality with a P value <.05 in the univariate analysis were then incorporated into a multivariate analysis, also based on Cox's proportional model.
All statistical analyses were carried out using a statistical software package (SPSS for Windows, version 16.0; SPSS Inc.; Chicago, IL, USA). A P value of <.05 was considered significant.
ResultsA total of 574 patients were eligible for the study, 357 (62.4%) men, mean age 68±11 years (range: 36–98). Six percent of the patients had never smoked and did not report biomass exposure, whereas 15% reported biomass exposure only. Twenty-seven percent of the patients were using neither oxygen nor NIV treatment at home and 23% were using both of those treatments at the time. The mean Charlson comorbidity index score was 2.2. Malignancy of any type was recorded in 31 (5.4%) patients.
Mean ABG values at NIV application were as follows: pH: 7.306±0.04, PaCO2: 66.5±10.5mmHg, partial arterial oxygen pressure (PaO2): 2.4±31.6mmHg; and hydrogen bicarbonate (HCO3). ABG values within 2h of NIV implementation in the ED were evaluated to decide to which unit the patient would be transferred. No patient with indications for ICU admission was transferred to the ward. Patients were transferred to the wards if they had mean ABG values of pH 7.358±0.04 and PaCO2 57.6±10.2mmHg. In the ED, mean inspiratory and expiratory positive airway pressure levels were 20.5±2.0 and 5.1±0.4, respectively. In the wards, mean inspiratory and expiratory positive airway pressure levels were 21.2±2.3; 5.3±0.5 cmH2O, respectively.
Mean length of stay in the wards was 9.2±5.2 days. During hospitalization, 25 (4%) patients were discharged voluntarily, 5 (1%) patients were transferred to other units for non-COPD indications (acute renal failure in 4 patients, gastrointestinal bleeding in 1 patient). Forty-three (7.5%) patients were transferred to the ICU and 24 (4.1%) patients died in the hospital, of whom 5 died in ICU. The remaining 477 patients were discharged to home. Seven percent (n=42) of all patients were discharged with a new indication of chronic NIV.
The mean in-hospital mortality time was 8.5±6 (1–22, median 5.5) days. Lower hematocrit level (P=.003), higher white blood cell count (P=.017), lower albumin level (P<.001), lower pH, and higher PaCO2 level after 24h of the treatment (P<.001) were related with in-hospital mortality. Age, gender, Charlson score, smoking status did not significantly vary between survivors and non-survivors. Baseline ABG levels, home oxygen and NIV treatment did not affect in-hospital death (Table 1).
Association of Predictive Factors with In-Hospital Mortality.
| Characteristics | All Patients | Survivors (n=550) | Non-survivors (n=24) | P value |
|---|---|---|---|---|
| Male (n; %) | 357 (62%) | 343 (62%) | 14 (58%) | .674 |
| Age (years) | 68.1±10.9 | 67.9±10.9 | 71.7±10.4 | .106 |
| Charlson index | 2.2±1.8 | 2.15±1.7 | 2.87±2.3 | .059 |
| Smoking status yes/ex/never (n, %) | 59/394/121 (10/69/21%) | 56/380/114 (10/69/21%) | 3/14/7 (13/58/29%) | 0.783 |
| LTOT before admission (n; %) | 325 (57%) | 314 (57%) | 11 (46%) | .298 |
| Long-term NIV before admission (n; %) | 124 (22%) | 120 (22%) | 4 (17%) | .800 |
| White blood cell count (×109/L) | 10.8±4.6 | 10.7±4.5 | 13.1±5.8 | .017 |
| Hematocrit (%) | 44.6±7.6 | 44.9±7.6 | 40.1±5.7 | .003 |
| Albumin (g/dL) | 3.1±0.5 | 3.2±0.5 | 2.5±0.5 | <0.001 |
| Initial pH | 7.306±0.04 | 7.307±0.04 | 7.294±0.06 | .214 |
| Initial PaCO2 (mmHg) | 66.5±11.4 | 66.4±10.4 | 68.0±12.1 | .484 |
| NIV IPAP (cmH2O) (in ED) | 20.5±2.0 | 20.5±1.8 | 21.1±2.1 | .294 |
| NIV EPAP (cmH2O) (in ED) | 5.1±0.4 | 5.2±0.1 | 5.1±0.2 | .585 |
| 2nd hour pH of NIV (ED) | 7.358±0.04 | 7.359±0.04 | 7.342±0.05 | .094 |
| 2nd hour PaCO2 of NIV | 57.7±10.2 | 57.5±10.1 | 61.2±10.6 | .126 |
| NIV IPAP (cmH2O) (ward) | 21.2±2.3 | 21.1±2.3 | 21.5±1.8 | .967 |
| NIV EPAP (cmH2O) (ward) | 5.3±0.5 | 5.3±0.5 | 5.2±0.4 | .480 |
| pH after 24h | 7.371±0.06 | 7.375±0.05 | 7.292±0.12 | <0.001 |
| PaCO2 after 24h (mmHg) | 60.6±13.9 | 60.0±12.6 | 71.7±27.9 | <0.001 |
ED: emergency department; EPAP: expiratory positive airway pressure; IPAP: inspiratory positive airway pressure; LTOT: long-term oxygen therapy; NIV: non-invasive ventilation; PaCO2: partial arterial carbon dioxide pressure
After the first admission, the median follow-up of the entire cohort was 27 months (range, 0–49 months). Median follow-up of patients who survived and died was 38 and 12 months, respectively. A total of 337 (58.7%) patients died, and median survival was 27 months (810 days) (Fig. 2). Mortality at 3 months, 6 months, and 1 year were 14.5%, 19.5%, and 30% respectively (Table 2).
In the univariate analysis, long-term mortality was related to older age, higher Charlson index score, lower hematocrit, lower albumin levels, and lower pH levels at the end of first day (Table 3). Multivariate analysis of survival, with inclusion of the significant factors in univariate analysis showed that older age and lower albumin levels were the strongest predictors of mortality (Table 4).
Predictive Results of the Parameters in the Cox's Univariate Analysis of All-Cause Long-term Mortality.
| Variables | Univariate Analysis | ||
|---|---|---|---|
| HR | 95% CI | P-value | |
| Male (n; %) | 0.931 | 0.746–1.163 | .531 |
| Age (years) | 1.029 | 1.019–1.040 | <.001 |
| Charlson index score | 1.130 | 1.069–1.194 | <.001 |
| Smoking status yes/ex/never | 1.118 | 0.683–1.831 | .904 |
| LTOT before admission | 0.929 | 0.747–1.155 | .506 |
| NIV at home before admission | 0.910 | 0.707–1.172 | .467 |
| Leukocytosis | 1.012 | 0.988–1.037 | .324 |
| Hematocrit | 0.972 | 0.957–0.987 | <.001 |
| Albumin | 0.535 | 0.415–0.690 | <.001 |
| Initial pH | 0.367 | 0.040–3.298 | .367 |
| Initial PaCO2 | 0.999 | 0.988–1.011 | .890 |
| 2nd hour pH on NIV | 0.380 | 0.021–6.731 | .509 |
| 2nd hour PaCO2 on NIV | 1.011 | 0.988–1.023 | .104 |
| pH after 24h | 0.133 | 0.015–1.209 | .048 |
| PaCO2 after 24h | 1.006 | 0.995–1.016 | .283 |
CI: confidence interval; HR: hazard ratio; LTOT: Long-term oxygen treatment; NIV: non-invasive ventilation; PaCO2: partial arterial carbon dioxide pressure.
Multivariate Analysis of All-cause Mortality (Cox REGRESSION analysis).
| HR | CI (95%) | P | |
|---|---|---|---|
| Age | 1.026 | 1.008–1.044 | .004 |
| Charlson score | 0.951 | 0.855–1.059 | .359 |
| Hematocrit | 0.982 | 0.962–1.003 | .097 |
| Albumin | 0.491 | 0.365–0.661 | <.001 |
| pH after 24h | 0.207 | 0.016–2.636 | .225 |
CI: confidence interval; HR: hazard ratio.
The current study revealed a median survival of 27 months after a COPD exacerbation treated with in-hospital NIV. To our knowledge, this is the largest series evaluating long-term mortality in COPD patients with AHRF receiving NIV in hospital wards. The predictors of in-hospital mortality were higher leucocytes, lower hematocrit, and lower serum albumin at admission, and lower pH and higher PaCO2 levels on ABG after 24h of treatment. Interestingly, ABG levels at the end of the first day of treatment appear to predict in-hospital mortality, irrespective of values at admission and at the second hour of treatment. For long-term mortality, older age and lower baseline albumin levels were the most relevant parameters. The findings of this study could help clinicians assess the clinical outcome of COPD exacerbations.
In-hospital mortality of a COPD exacerbation ranges widely, depending on the patient population and the unit where the patient was managed. In-hospital mortality of any COPD exacerbation has been reported to be between 2.5% and 8.3%.12,14,15,17 In patients with a PaCO2 level of 50mmHg or more, the rate increases to 11%.27 In ICU management of AHRF, the mortality rate has been reported to be as high as 53% in patients managed with mechanical ventilation. When invasive ventilation is not required and NIV treatment is sufficient, this rate decreases to 8%.21 In addition to the ventilation type, the type of management unit is important in AHRF. Dave et al. compared the AHRF of COPD patients in terms of ICU and non-ICU management. They reported that in-hospital mortality is significantly lower in patients managed in the ward compared to patients who required ICU attention.10 Overall in-hospital mortality of patients treated with NIV has decreased over time. Before 2000, reported rates were greater than 10%, whereas in 2008 the rate had decreased to 5%.8 In this study, in-hospital mortality was 4%, a little lower than other reported series. The first reason for this situation may be that our hospital is a reference center and patients are more homogenous. Secondly, all our nurses and medical caregivers are trained in NIV procedures. Significant factors for in-hospital mortality after any COPD exacerbation have been reported to be longer hospital stay, lower PaO2, higher PaCO2 at presentation, and lower FEV1/FVC.12 In another study, predictive factors were identified as older age, male gender, higher income, unscheduled admission, and the number of comorbid diseases.15 In this study, the following were identified as significant predictors of in-hospital mortality: higher white blood cell count, lower hematocrit, lower albumin levels at admission, lower pH, and higher PaCO2 level after 24h. Similarly, other authors have reported leukocytosis, anemia and hypoalbuminemia as indices of in-hospital mortality.28,29 Hypoalbuminemia has also been found to predict in-hospital mortality. ABG levels after 24h also correlated with in-hospital mortality.
Long-term survival of COPD exacerbations also differs with respect to the management unit and NIV requirement. Gunen et al. reported 33% mortality 1 year after any COPD exacerbation.12 Groenwegen et al. found 6-month and 1-year mortality rates after exacerbation of 18% and 23%, respectively. They also found that in patients transferred to the ICU, the mortality rate increased significantly (21% of non-ICU patients and 35% of ICU patients died within 1 year).14 Titlesad et al. also investigated the long-term survival of patients presenting in the ED, who were subsequently transferred to the wards, where they received NIV for the first time. Five-year mortality was reported as 76.3%.22 Connors et al. studied a cohort of patients with COPD exacerbation who had PaCO2 levels of more than 50mmHg. Six-month, 1-year and 2-year mortality was 33%, 43% and 49%, respectively.27 Chung et al. have investigated the outcome of COPD exacerbation requiring NIV. Mortality at 1, 2 and 5 years was reported as 28%, 48%, and 24%, respectively. Overall mean survival was 25 months.23 Among COPD patients with acute exacerbation who received NIV, 1-year mortality has been reported as 39% with a median survival of 16.8 months.30 In our study, median patient survival was 27 months. Six-months, 1- and 2-year mortality were 19.5%, 30%, and 47.7%, respectively.
In our univariate analysis, long-term survival was found to be related to age, Charlson index, hematocrit and albumin levels at admission and pH levels 24h after admission. In multivariate analysis, age and albumin levels were the strongest predictors of mortality. Gunen et al. found disease duration, albumin level, PaO2, and body mass index (BMI) to be significantly related to mortality. On the other hand, PaCO2, comorbidity index, duration of hospital stay, smoking status, and smoking pack-years index did not correlate significantly with mortality.12 Long-term use of oral corticosteroids, higher PaCO2, older age, and prior NIV usage were associated with poorer survival after COPD exacerbations requiring hospitalization.14,31 Titlesad et al. reported that advanced age and do-not-intubate statement were predictors of long-term survival, whereas gender, baseline pH, PaCO2 and comorbidities were not significant.22 Connors et al. have reported factors determining poorer survival to be BMI, age, prior functional status, PaO2/FiO2, congestive heart failure, serum albumin level, and cor pulmonale.27 Chung et al. described long-term mortality predictors as older age, lower BMI and long-term oxygen treatment (LTOT). Hospital stay, gender, and ABG levels recorded at presentation, 2h and discharge were not correlated with life expectancy.23
Since FEV1 decreases each year, mortality is expected to increase with advanced age.32 In line with the literature, we found advanced age to be an independent predictor of mortality.16,22,32 Although male gender is reported as a predictor of in-hospital mortality,15 long-term survival is not correlated with gender.12,23 Neither in-hospital nor long-term mortality yielded a relationship with gender in our study.
Charlson index has been shown to be related with all-cause mortality in stable COPD patients receiving LTOT.33 However, no significant correlation between Charlson index and in-hospital or long-term mortality following an exacerbation is reported.15,34 Chung et al. did not find any correlation between the number of comorbidities and in-hospital or long-term mortality.23 In this study, we also did not find any relationship between in-hospital mortality and Charlson index. In line with the literature, we did not find the Charlson score to be an independent factor.
Both smoking status and pack-year index are generally reported to be irrelevant in long-term mortality and our study confirms this trend.12,34 Long-term oxygen therapy has not been shown to be related to in-hospital or long-term mortality.16,23 In line with the literature, mortality did not increase significantly in patients receiving LTOT in our study. In contrast, lower levels of serum albumin were found to be a strong predictor of poorer life expectancy. Serum albumin is thought to be an acute phase protein response and it is often associated in chronic diseases with negative outcome.12,21 Anemia and higher white blood cell levels have been shown to increase mortality,21,28 also observed in our study.
Baseline ABG levels have been reported to be related with in-hospital mortality after the COPD exacerbations treated in the ICU.12,14,21 However, when patients treated with or without NIV in wards were compared, hypercapnia levels were not found to influence in-hospital mortality.30 Chung et al., in a similar patient population to ours, did not find any significant relationship between baseline ABG levels and mortality. In this study, we also found that baseline ABG values did not have a significant effect on in-hospital and long-term mortality. Interestingly, we found that the lower pH and higher PaCO2 values after 24h predicted in-hospital mortality. Although long-term mortality correlated in the univariate analyses with a lower level of pH after 24h of treatment, no significant association was detected in the multivariate analyses. In our opinion, ABG values, particularly pH values after 24h of NIV, could give some indication to the clinician regarding the patient's prognosis.
There were some limitations to this study. Firstly, it was a retrospective, single-center study. Secondly, spirometric data and body mass indices could not be recorded since they were not available from medical charts. The strength of the study is the large sample size, which provides valuable clinical information for assessing the outcome of hypercapnic COPD exacerbations. The other strength of the study is that chest disease specialists and chest disease fellows attended patients both in the ED and in the wards.
In conclusion, life expectancy after a COPD exacerbation requiring NIV treatment is short. In-hospital mortality predictors are lower hematocrit, higher white blood cell count, lower albumin and ABG levels at the end of the first day of the treatment. The strongest factors for predicting a poorer outcome are old age and low albumin levels. Such patients need closer follow-up and treatment.
AuthorshipFTA, HG, and MCA designed the study. FTA, MY, MA, PS, and SG collected data. FTA, HG, and MY analyzed the data. FTA, MCA, SG, MY, MA, and PS reviewed medical charts. FTA, HG, and SG wrote the paper. HG, SG, MY, and TS reviewed the paper.
Conflict of interestThe authors declare that there is no conflict of interest.
Gunen H is the guarantor of the content of the manuscript, including the data and the analysis.
Please cite this article as: Akyil FT, Gunen H, Agca M, Gungor S, Yalcinsoy M, Sucu P, et al. Supervivencia en exacerbaciones de la EPOC que requirieron ventilación no invasiva en planta. Arch Bronconeumol. 2016;52:470–476.