The new 2009 TNM classification introduced important modifications in lung cancer staging. The aim of this study is to validate our series of patients with pathologic stage I non-small-cell lung cancer according to the 7th edition of the TNM classification of malignant tumors and to the factors related with prognosis.
Patients and methodsA multicenter retrospective study was performed. Survival rates were calculated by the Kaplan–Meier method, and for multivariate analyses, Cox proportional hazards regression model was used. The following variables were analyzed: age, sex, pathologic stage, T category, histology, type of resection and tumor size.
ResultsA total of 402 patients were included. Mean follow-up was 70.18 months. Overall 5-year survival was 68%. Males and patients over 70 had lower survival. Prognosis worsened with increasing pathologic stage, T category and tumor size. We found no statistically significant differences in prognosis for histology or type of resection. Multivariate analysis showed age, sex and pathologic stage to be independent prognostic factors.
ConclusionsSurvival results and the analysis of prognostic factors in our series are similar to those published in the new 2009 TNM classification. The most important prognostic factor is pathologic stage. Other adverse prognostic factors include male sex and age over 70.
La nueva clasificación TNM de 2009ha introducido importantes modificaciones en la estadificación del cáncer de pulmón. El objetivo de este trabajo es validar nuestra serie de pacientes con carcinoma no microcítico de pulmón en estadio I patológico según la séptima edición de la clasificación TNM de los tumores malignos y analizar los factores relacionados con el pronóstico.
Pacientes y métodosSe realizó un estudio retrospectivo y multicéntrico. Para el análisis de supervivencia se utilizó el método de Kaplan–Meier y para el análisis multivariable, la regresión de Cox. Se analizaron las siguientes variables: edad, sexo, estadio patológico, categoría T, tipo histológico, tipo de resección y tamaño tumoral.
ResultadosSe incluyó a 402 pacientes con un seguimiento medio de 70,18 meses. La supervivencia global a los 5 años fue del 68%. Los varones y los pacientes mayores de 70 años tenían una menor supervivencia. El pronóstico empeoraba a medida que aumentaba el estadio patológico, la categoría T y el tamaño tumoral. No encontramos diferencias pronósticas estadísticamente significativas en relación con el tipo histológico y el tipo de resección practicada. El análisis multivariable mostró que la edad, el sexo y el estadio patológico son factores pronósticos independientes.
ConclusionesLos resultados de supervivencia y el análisis de factores pronósticos de nuestra serie se ajustan a los publicados en la nueva clasificación TNM de 2009. El factor pronóstico más importante es el estadio patológico. Otros factores pronósticos desfavorables son el sexo masculino y la edad mayor de 70 años.
Lung cancer, due to its incidence and mortality, is a public health problem in developed Western countries.1,2
In 2009, the UICC and the AJCC published the seventh edition of the TNM classification for malignant tumors, in effect since January 2010. In this edition, the lung cancer classification, which has incorporated important modifications, was updated by the International Staging Committee of the IASLC, presided by Dr. P. Goldstraw, President.3,4
Approximately 80% of all lung cancers belong to the group of non-small-cell carcinomas. In this histologic type, complete surgical resection is the treatment of choice in the initial stages, although surgical approaches and techniques are evolving.5
Despite recent medical advances, survival of patients with lung cancer is low. If we center on non-small-cell carcinomas, which is the aim of this study, overall five-year survival in Europe does not surpass 15% in any of the European countries.6,7 Approximately 30% of patients with non-small-cell lung cancer in stage I who undergo complete resection relapse and die within 5 years, fundamentally due to the presence of micrometastasis at the time of resection.8 It is not known, however, what mechanisms produce these recurrences or in which patients they will occur.
The identification of prognostic factors in lung cancer is very useful for assessing the individual patient prognosis, selecting the best treatment, defining new criteria to classify patients according to risk groups and helping design and direct future research.9
In recent years, more than 150 variables have been identified that have been described as prognostic factors in lung cancer and may implicate the tumor, the patient or the setting.10
Therefore, the objectives of this study are to validate our surgical series of patients with pathologic stage I non-small-cell pulmonary carcinoma according to the seventh edition of the TNM classification for malignant tumors and to identify the factors that may be related with prognosis.
Patients and MethodsPatientsPatients who underwent surgical treatment for pathologic stage I non-small-cell lung cancer by the Thoracic Surgery Departments at the Hospital General Universitario Gregorio Marañón (between 1991 and 2005), the Complejo Hospitalario Xeral-Cies in Vigo (between 2000 and 2004) and the Complejo Hospitalario Universitario in Albacete (between 2001 and 2006) with complete lung resection. The patients had not received either adjuvant or induction treatment.
MethodsWe performed a multi-center, retrospective study, analyzing survival and determining prognostic factors.
The clinical data of the patients were compiled in a protocol that was common for the three health centers that participated in the study and were later introduced into a Microsoft Access® database designed for their analysis.
This database included clinical variables as well as those from imaging studies, surgical intervention protocol and pathological anatomy reports, as well as data from the outpatient consultation follow-up (Table 1).
Variables Collected for the Study.
| Clinical |
| Age |
| Sex |
| Tobacco habit |
| Date of lung cancer diagnosis |
| Imaging studies |
| Laterality |
| Anatomical location |
| Surgical intervention protocol and pathological anatomy report |
| Date of surgical intervention |
| Type of lung resection |
| Tumor size |
| Histological type |
| Degree of differentiation |
| Surgical-pathological stage |
| Post-op follow-up |
| Date of last examination |
| Disease state |
| Date and location of relapse |
| Date and cause of death |
In all patients, complete surgical resection was performed. Lobectomy was considered the standard lung resection. Pneumonectomy was carried out when required due to technical or oncological reasons. Atypical lung resection was done in patient with high surgical risk or poor cardiorespiratory reserve. Usually, lymphadenectomy was performed systematically after lung resection, including the nodes of the hilar and mediastinal regions.
For the survival analysis and prognostic factors, the following variables were selected: age, sex, pathologic stage, T category (TNM), histologic type, resection type and tumor size.
The statistical analysis was done with SPSS 15.0 software package for Windows. In order to compare the independent quantitative variables, we used the Student's t test, the Kruskal–Wallis test and the Mann–Whitney U test. Correlations between two categorical variables were studied with the χ2 test. The survival analysis was calculated with the Kaplan–Meier product-limit method. Log-rank was used to evaluate whether the differences observed on two survival curves could be explained by chance. For the multivariable analysis, we constructed a Cox proportional hazard model (“enter” method) including the following variables: age, sex, histologic type, type of surgical resection and stage. A P value <.05 was considered statistically significant.
ResultsThe sample selected for the study was composed of 402 patients: 180 from the Hospital General Universitario Gregorio Marañón, 49 of which had been included in the SEPAR study by the Bronchogenic Carcinoma Workgroup (in Spanish, GCCB-S); 135 from the Complejo Hospitalario Xeral-Cies; and 87 from the Complejo Hospitalario Universitario in Albacete.
At the time of the surgical intervention, the patients were between 35 and 83 years of age, with a mean age of 64 (SD 9). 87% were males and the right hemithorax was the most frequently affected. As for tobacco habit, 51% were active smokers at the time of the diagnosis, 40% were ex-smokers and only 9% had never smoked. The most frequent histologic type was epidermoid carcinoma, which is being a predominantly poorly and moderately defined tumor. The average tumor size was 2.5cm and 38% of the tumors were stage IA. The most relevant clinical surgical data are shown in Table 2 and the pathological data are shown in Table 3.
Clinical and Surgical Data (n=402).
| Patients, n (%) | |
| Age | |
| <70 | 290 (72) |
| >70 | 122 (28) |
| Sex | |
| Male | 350 (87) |
| Female | 52 (13) |
| Affected hemithorax | |
| Right | 245 (61) |
| Left | 157 (39) |
| Tobacco habit | |
| Active smoker | 205 (51) |
| Ex-smoker | 161 (40) |
| Never smoker | 36 (9) |
| Pre-op diagnosis | |
| Yes | 173 (43) |
| Tumor location | |
| Upper lobe | 277 (69) |
| Middle lobe | 20 (5) |
| Lower lobe | 105 (26) |
| Type of resection | |
| Atypical resection | 71 (18) |
| Lobectomy | 269 (67) |
| Bi-lobectomy | 18 (4) |
| Pneumonectomy | 44 (11) |
Pathological Data (n=402).
| Patients, n (%) | |
| Histology | |
| Epidermoid carcinoma | 196 (49) |
| Adenocarcinoma | 186 (46) |
| Large-cell carcinoma | 18 (4.5) |
| Adenosquamous carcinoma | 2 (0.5) |
| Degree of differentiation | |
| Good | 64 (16) |
| Moderate | 185 (46) |
| Poor | 153 (38) |
| T, TNM | |
| T1a | 93 (23) |
| T1b | 62 (15) |
| T2a | 247 (62) |
| Size, cm | |
| 0–2 | 144 (36) |
| 2.1–3 | 126 (31) |
| 3.1–5 | 132 (33) |
After a mean patient follow-up time of 70.18 months with a standard deviation of 45.15 months (range, 1.8–218.07), 186 patients (46%) were alive and disease-free, 18 (4%) were alive but with metastatic disease, 135 (34%) had died as a direct consequence of the relapse of the tumor disease and 63 (16%) had died due to causes other than lung cancer.
Overall survival was analyzed, as were the different variables described in “Patients and Methods” section that could affect survival. The two adenosquamous carcinomas were grouped together with the large-cell carcinomas for the survival analysis depending on the histological type. The 18 bi-lobectomies were grouped with the 269 lobectomies when survival was analyzed according to type of resection. Survival was also analyzed solely depending on tumor size, grouping the tumors into 3 groups: tumors between 0 and 2cm, tumors between 2.1 and 3cm and tumors between 3.1 and 5cm.
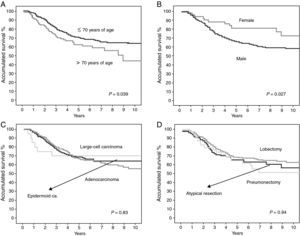
Table 4 summarizes the findings of the statistical analysis for total survival depending on the variables described. The overall 5-year survival rate of the series was 68%. Being male and being over the age of 70 were factors that both had a negative prognostic influence. In addition, the prognosis worsened as the stage, T category and tumor size increased. We found no statistically significant differences when comparing survival according to histologic type or resection type.
Five-Year Survival Analysis According to the Kaplan–Meier Method (n=402).
| Patients, n (%) | P | |
| Global Sv | – (68) | – |
| Sv/age | .039 | |
| <70 | 290 (71) | |
| >70 | 122 (62) | |
| Sv/sex | .027 | |
| Male | 350 (66) | |
| Female | 52 (72) | |
| Sv/histology | .83 | |
| Epidermoid carcinoma | 196 (69) | |
| Adenocarcinoma | 186 (66) | |
| Large-cell carcinoma | 20 (70) | |
| Sv/type of resection | .94 | |
| Atypical resection | 71 (65) | |
| Lobectomy | 287 (68) | |
| Pneumonectomy | 44 (68) | |
| Sv/stage | .001 | |
| IA | 155 (76) | |
| IB | 247 (62) | |
| Sv/T category | .005 | |
| T1a | 93 (73) | |
| T1b | 62 (69) | |
| T2a | 247 (62) | |
| Sv/tumor size | .027 | |
| 0–2cm | 144 (73) | |
| 2.1–3cm | 126 (70) | |
| 3.1–5cm | 132 (59) | |
Sv, survival.
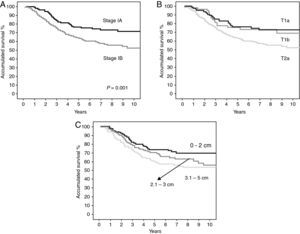
Figs. 1 and 2 show the survival curves of the patients depending on the variables previously analyzed and show the statistical differences found.
(A) survival curves of the patients by the Kaplan–Meier method according to pathologic stage and the statistical difference found. (B) Survival curves of the patients by the Kaplan–Meier method according to T category; statistically significant differences were found between the survival curves for T1a and T2a (P=.005), and between the survival curves of T1b and T2a (P=.049); statistical significance was not met between the curves of T1a and T1b (P=.68). C) Survival curves of the patients by the Kaplan–Meier method according to tumor size; statistically significant differences were found between the survival curves for 0–2cm and 3.1–5cm (P=.01); statistical significance was not reached between the survival curves for 0–2cm and 2.1–3cm (P=.13), or between the survival curves for 2.1–3cm and 3.1–5cm (P=.28).
The multivariable analysis done with the Cox proportional hazards model (Table 5) showed that age, sex and tumor stage are independent prognostic factors. The analysis, adjusted for the rest of the variables that were entered into the model, showed that the patients in stage IB have a risk for death that is 1.81 greater than the patients in stage IA. The analysis also showed that males are 2.15 times more likely to die than women, while patients over the age of 70 have a risk for death 1.02 times greater than younger patients.
Multivariable Survival Analysis Using the Cox Proportional Hazards Model.
| P | HR | 95% CI of HR | |
| Age (>70 vs <70) | .036 | 1.023 | 1.001–1.044 |
| Sex (male vs female) | .018 | 2.154 | 1.14–4.069 |
| Histologic type | .228 | – | – |
| Epidermoid ca. vs adenocarcinoma | .506 | 1.331 | 0.573–3.093 |
| Epidermoid ca. vs large-cell | .939 | 0.968 | 0.416–2.254 |
| Type of resection | .561 | – | – |
| Atypical resection vs lobectomy | .693 | 0.876 | 0.454–1.69 |
| Atypical resection vs pneumonectomy | .331 | 0.767 | 0.449–1.31 |
| Stage (IB vs IA) | .002 | 1.814 | 1.238–2.658 |
HR, hazard ratio: CI, confidence interval.
The main modifications that have been introduced by the 2009 TNM classification in stage I lung cancer refer to tumor size, currently being restricted to tumors of up to 5cm in diameter.3,11,12 This has meant that we have had to exclude quite a few patients by re-staging them according to the seventh edition of the TNM classification for malignant tumors, as they had been treated before its publication and the pathological stage had been determined with the previous staging system from 1997.13 However, as our research was centered on patients in pathological stage I, none presented lymphadenopathy involvement, which allowed us to re-stage the patients correctly and avoid the possible discrepancies derived from the modifications made in the new lymph node map.14
We excluded the patients who received either adjuvant or induction chemotherapy as they can alter evolution and survival. Various randomized studies have confirmed the improvement in survival provided by adjuvant chemotherapy based on platinum in the initial stages of completely resected lung cancer. However, in stage IA chemotherapy has had deleterious results, basically due to the alteration in the immune system and the accompanying infectious complications.8,15–18
In the new TNM staging system, the most important factor used for the classification according to the categories T, N and M and the grouping by stages has been overall survival.3,4 In our series, we have also used overall survival as a method to statistically analyze prognostic factors as we believe that it is a much more objective factor to identify (using date of death) than the disease-free interval because it is often difficult to determine the exact time of relapse.
The overall five-year survival of our series is 68%. In stage IA, the 5-year survival rate is 76% and in IB it is 62%. The 5-year survivals after the analysis of the data with the new TNM classification for pathological stages IA and IB are 73% and 58%, respectively.4,11 Given these findings, we can conclude that our survival results are similar to those published in the seventh edition of the TNM lung cancer classification; therefore it can be validated with the new 2009 staging system.
The data of the 49 patients of the Hospital General Universitario Gregorio Marañón who had participated in the GCCB-S study were included in the database that the IASLC used to update the new 2009 TNM classification. Therefore, this study can be considered the first external Spanish validation (not GCCB-S) of the innovations introduced by the IASLC.
Chansky et al.19 analyzed the prognostic factors of the patients with non-small-cell lung cancer treated surgically that were used to create the new TNM classification and they found that the most important prognostic factor is the TNM pathologic stage. This finding is also seen in our series, where we have found statistically significant differences both in the analysis by stages (IA against IB) as well as in the overall survival analysis for the T categories (T1a, T1b and T2a). However, in analyzing the statistical differences between the survival curves of the T category, comparing the curves two by two, statistical significance was only reached between curves T1a and T2a, and T1b with T2a. Statistical significance was not reached when comparing the survival curves between T1a and T1b that supports these two T categories being included in the same IA stage.
Some authors have published the prognostic value of the tumor size itself.3,4,12,20 We therefore also analyzed the survival of the patients in our series, classifying them by size alone (without contemplating invasion of the visceral pleura, involvement of the main bronchus at more than 2cm from the carina or obstructive pneumonitis that does not affect the entire lung) and we found that there were also statistically significant differences in the global analysis of this descriptor (P=.027). However, in the comparative analysis between the different curves, we only found statistically significant differences between the survival curves for 0–2cm and 3.1–5cm (P=.01); although statistical significance was not reached, a relevant clinical influence was observed between the survival curves for 0–2cm and 2.1–3cm (P=.13), and between the survival curves for 2.1–3cm and 3.1–5cm (P=.28). The differences between the survival curves of the T category and the size descriptor are due to the influence on survival of the other descriptors of the T category mentioned previously, which were not able to be validated in the current TNM classification,21 and therefore have not been aims of this study.
Chansky et al.19 also found that sex and age are important prognostic factors in surgically resected non-small-cell lung cancer. Likewise, our series confirms that male sex and age over 70 are unfavorable prognostic factors.
In the survival study according to histologic type, we found no statistically significant differences. Chansky et al.19 obtained better survival of patients with bronchioloalveolar carcinoma, as already published by other authors.19,22,23 In our series, however, this relationship was not studied as the few cases of bronchioloalveolar carcinoma were included in the adenocarcinoma group for the statistical analysis.
Currently, lobectomy is considered the best oncological resection for the treatment of lung cancer as there is a greater percentage of relapse in atypical resections and segmentectomies.24 Nevertheless, recent studies have reported results comparable to those of lobectomy in small-sized peripheral tumors, basically bronchioloalveolar carcinomas.25–28 Thus, in the current recommendations, minor resections of a lobe are reserved only for this type of tumors under the right conditions.29 In our series, we also did not find differences in survival according to surgical resection type.
In conclusion, the analysis of the survival and prognostic factors in our series conforms to the results of the new TNM lung cancer classification. The most important prognostic factor is pathological stage. Other unfavorable prognostic factors are being male and being over the age of 70.
Conflict of InterestWe, the authors, declare having no relationship with either people or entities, either public or private, susceptible to generating a potential conflict of interests, either in relationship with specific economic interests or personal or professional implications, such as hiring, consulting, investing, research funding, and family relations, either past or present, according to the regulations of the International Committee of Medical Journal Editors.
Please cite this article as: León-Atance P, et al. Análisis multicéntrico de supervivencia y factores pronósticos en el carcinoma no microcítico de pulmón en estadio I patológico según la nueva clasificación TNM de 2009. Arch Bronconeumol. 2011;47:441–6.