Home oxygen therapy has been classically based on the use of compressed oxygen cylinders and portable oxygen (O2) concentrators. In the past few years, we have witnessed the advent of portable oxygen therapy equipment and liquid oxygen systems and even more recently portable O2 concentrators. This equipment allows for greater patient mobility, which generates new issues that we must understand and approach adequately. One of these is selecting the best oxygen source for each patient. In doing so, it is necessary to compare the patient mobility profile with the mobility allowed by the O2 sources in order to determine the degree of correlation between the two. Proper indication for home oxygen therapy, the selection of the right source and the titration of the oxygen flow are three components which we must face when deciding to prescribe home oxygen therapy. The patient must also cooperate with correct O2 use.
La oxigenoterapia crónica domiciliaria (OCD) se ha realizado clásicamente con botellas de oxígeno comprimido y concentradores portátiles de oxígeno (O2). En los últimos años hemos asistido a la incorporación de equipos de oxigenoterapia portátil, como los sistemas de oxígeno líquido y, más recientemente, los concentradores portátiles de O2. Estos equipos permiten una mayor movilidad de los pacientes, lo cual genera nuevos problemas que debemos conocer y abordar adecuadamente. Uno de ellos es la selección de la fuente de oxígeno más apropiada para cada paciente. Para ello es necesario tener en cuenta la movilidad permitida por las fuentes de O2 para contrastarla con el perfil de movilidad del paciente y ver el grado de correlación entre ambos. La correcta indicación de OCD, la selección de la fuente adecuada y la titulación del O2 necesario para ese paciente son los tres componentes a los que debemos enfrentarnos en estos momentos cuando decidimos prescribir oxigenoterapia domiciliaria. El paciente debe colaborar con una utilización correcta del O2.
At the beginning of the 1980s, two studies were published that set the foundation for home oxygen therapy (HOT) as we know it today. We are referring to the MRC1 and NOTT2 studies. What we learned from them was that the administration of oxygen (O2) during a minimum of 16h daily in COPD patients with severe hypoxemia improved survival and quality of life. From then until now, few changes have taken place in the indications for home oxygen therapy. Advances have been made, however, from a technological standpoint. Competing with compressed oxygen bottles and traditional O2 concentrators, at the beginning of the 1990s portable liquid oxygen systems appeared, which favored the development of ambulatory oxygen therapy.3–6 Later, the development and diffusion of oxygen-saving systems provided the devices with increased autonomy and gave patients a higher degree of freedom.7 That latest achievement in the field of home oxygen therapy has been the incorporation of portable oxygen concentrators (POCs), which increase the possibilities for these patients to interact with their surroundings.8–11 The image of the chronic respiratory disease patient unable to lead an active life has come to an end, and it is a challenge that society needs to take on.12,13
Nevertheless, the greater mobility of our patients generates new problems that we should understand and handle adequately. One is the selection of an appropriate oxygen source for each case. The current contractual agreements between supply companies and the Spanish Health Care Administration establish that one single oxygen therapy system should be provided to patients who are prescribed home oxygen therapy (HOT).8,14–17 Therefore, proper selection is important. When stationary sources are prescribed, these are usually gaseous oxygen bottles or oxygen concentrators. In this latter case, the patients are usually also provided with a bottle of medicinal O2 for use in case of power outages. For patients who are prescribed HOT with liquid oxygen, the supplier provides a reservoir and a portable pack that is re-filled from the reservoir, and the patient is also given an O2 tank for use in case of loss of liquid O2. Recently, HOT has begun to be prescribed with portable concentrators although there is still no clear indication of which conditions should favor its prescription. The duplicity of systems is not contemplated under the current regulation; therefore, a patient cannot have at home a concentrator and a liquid O2 system. Nevertheless, the incorporation of portable concentrators is being done while maintaining the stationary concentrator of the patient and the reserve tank of gaseous O2.7 To complicate the situation more, there is also the concept of deliveryless technology,18 which could be explained as the search for oxygen therapy equipment that satisfies all the needs of the patient: wide-spectrum equipment that would guarantee the O2 supply both at home as well as away from home with one single oxygen source, providing greater convenience for the patient. Portable concentrators would be one of the main elements to consider if steps are to be made in the field of deliveryless technology. These POCs, which work in pulses although some of them incorporate the possibility of supplying continuous flow, have opened a new work field in HOT in addition to new problems, such as titrating oxygen therapy. The traditional prescription of “oxygen therapy with nasal tubes at 2l per minute, a minimum of 16h a day” no longer makes sense in this new scenario in which some devices do not even work by liters per minute.19,20
We thus find ourselves in a situation where, in addition to establishing the indication for HOT, it is essential to first select the best O2 source for each patient. Secondly, the proper O2 flow provided should be based on either home or ambulatory use, and whether the flow used is continuous or pulsating.21,22 In doing so, it is necessary to evaluate the mobility profile of our patients to better understand their habits of movement as, social and work commitments, whether they attend a day center, take care of grandchildren or periodically alternate between homes. Only with this knowledge will we be able to select the best oxygen source, while being aware of the fact that there is no single, perfect oxygen-therapy system that covers all the needs of a specific patient. We will try to develop the scenario of home oxygen therapy depending on the mobility profile of the patients, analyzing which O2 source would better adapt to each situation. In the evaluation of the prescription of HOT, these aspects of mobility must be kept in mind in order to decide which is the best device or what combination of devices would be the best in each case. To begin, we will comment on the patterns of mobility provided by current O2 sources, and then the different mobility profiles of our patients.
Mobility Patterns of the Oxygen Therapy SourcesStationary O2 sources, tanks and concentrators, provide the patient with a certain degree of mobility with the use of extension tubing. This pattern of mobility could be represented by a circle with the oxygen source in the center and the radius representing the length of the extension tubing (Fig. 1).
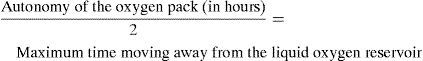
The mobility of the patient who receives HOT using a liquid O2 system depends on the autonomy of the pack. This is re-filled from the reservoir, and the autonomy of the patient is therefore limited by the duration of the pack supply. This pattern of movement could also be represented by a circle, with the re-fill point in the center. The patient may use half of the O2 fill to move away from the reservoir, reserving the other half to return to the re-fill point (Fig. 2). The furthest point which the patient could reach while receiving O2 could be represented by the equation:
Mobility pattern of patients receiving oxygen therapy with liquid O2 equipment. The circle shows the maximum distance that the patient can move away from the point to re-fill the liquid O2 pack, and the reservoir is situated in the center. The duration of the pack determines the diameter of the circle.
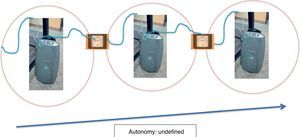
Portable oxygen concentrators (POCs) depend on their electrical supply. Their autonomy with batteries can be higher or lower, but, as long as there are electrical outlets or replacement batteries, the equipment will work and the batteries can be recharged. This mobility profile could be represented by a line joining recharge points (outlets, batteries) (Fig. 3), therefore the autonomy in this instance could be considered undefined. In fact, mobility with this equipment is only conditioned by its own technical characteristics. The smaller models that have fewer features, like the FreeStyle™ by AirSep®, heat up if used during long periods of time and have few options for flow regulation, and they therefore have many limitations. The higher-end POC, such as Evergo® (Respironics) or InogenOne® (Inogen, Goleta, California), allow for continuous use and their flow range is more extensive, although they have the disadvantage of only working in pulses. Last of all, there are other POCs, such as the Eclipse™ (SeQual Technologies) that incorporate the possibility of working either in pulses or in continuous flow. This equipment, therefore, guarantees the oxygen needs of more demanding patients.23
It is important to emphasize that when prescribing HOT with a portable source, not only is it necessary to evaluate whether patients would do better with liquid O2 or a POC, but it is also fundamental to determine which specific POC is better adapted to the needs of our patients depending on the mobility afforded.
Patient Mobility ProfilesAs we have seen, it is important to know the mobility that each oxygen source provides in order to compare this with patient mobility profiles and find the degree of correlation between them. Let us take a look at the different patient scenarios.
Oxygen Therapy at HomeIn recent years, we have seen a clear improvement in the living conditions of Spanish society in general and of housing in particular. Many of our patients have been able to afford larger homes, with a significant increase in single-family homes with more than one story. Therefore, when we talk about home oxygen therapy, it is necessary to know the type of home where the patient lives. Those who live in apartments may use HOT with stationary or portable sources, as we have previously commented. Extension tubing guarantees that the patient can move around the home while receiving O2. The problem arises in large-size homes, distributed over one or more stories, or in homes with yards. In this case, stationary concentrators or O2 tanks would not be recommendable. Liquid O2 could be used, installing the reservoir tank in a central area of the home, and using a pack to move around. It must be kept in mind that the pack will need to be re-filled every 4–6h. If there are stairs, this would condition the location of the reservoir tank in order to not have to go up or down stairs periodically to re-fill. The portable concentrator could be a valid alternative as electrical outlets are easily available in the home. It is important to remember that there should be no smoking in the presence of O2, regardless of the home source that is used.24
HOT and TransportationPatients are traveling more and more. Regardless of the destination, some things must be taken into consideration depending on the type of transportation involved. As a rule, if there is no HOT system available at the destination point, POC should be the equipment of choice.
- •
Automobile: POC is the best choice for long trips as it can be plugged into the cigarette lighter. Nevertheless, for short distances within the autonomy time limit of the pack, liquid O2 can be used.
- •
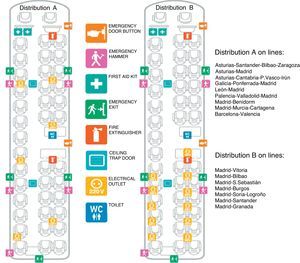
Bus: For short distances, liquid O2 or POC may be used. For long trips, POC has more advantages. The patient may ask to sit near the driver and ask permission to plug into the cigarette lighter of the vehicle. Certain bus lines have seats with electrical outlets that may be requested preferentially by patients with oxygen therapy (Fig. 4).
Fig. 4.Distribution of electrical outlets in the fleet of buses of a Spanish bus company with service to important cities in Spain. The company has two different distributions of outlets available for passenger use: distribution A has 6 outlets and distribution B has 11 outlets. These seats should be requested by patients with oxygen therapy.
- •
Train: On short trips, liquid O2 or POC may be used. For longer distances, POC has advantages. There are usually electrical outlets in the bathrooms and in the dining car, and in new-age train the seats have outlets available, if not throughout the train then at least in first class (Fig. 5). It is important to ask about this possibility when making the reservation.
- •
Boats: Here, once again, POC is the portable oxygen therapy system of choice. There are outlets distributed in cabins and common areas where POC may be used.
- •
Cruises: These are longer voyages by boat, which generally last a week. In this case, different considerations are needed because this situation entails characteristics of home oxygen therapy (cabin) with an important degree of activities (movement around the ship, activities and day trips on shore). Installing a liquid O2 reservoir in the patient's cabin while using the pack for movement around the ship and trips, within the autonomy limits of the HOT equipment, can be an option (Fig. 6). The use of a POC on the ship poses no problems, and on trips ashore, as these are usually done by bus, the use of the lighter socket, in combination with external batteries, can guarantee the supply of O2 for a greater number of hours than with liquid O2.
- •
Airplane: Liquid O2 cannot be used aboard an airplane. Until a few years ago, the only possibility to travel by plane with O2 was with the use of bottles of gaseous O2. Recently, the American Department of Transportation has approved the use of portable oxygen concentrators and their use during takeoff, landing and for movement around the cabin. At the same time, they help the patient move to/from the plane and through terminal. The Federal Aviation Administration (FAA) approved this regulation in 2005. It is important to mention that the air transportation of a POC is an exception to the technical instructions of the International Civil Aviation Organization (ICAO) and the regulations of dangerous products by the International Air Transport Association (IATA). Granting permission to travel with a POC is the responsibility of the airline, respecting any governmental variation that may be established by the authorities. The ICAO has remained on the sidelines, as one of the factors that forced the FAA to authorize the use of POCs was the request made by associations of passengers with reduced mobility based on the argument that there should not be discrimination against these passengers. Various POC models available on the market have become approved for this use. One requirement is that the patients provide their own POC accepted for use aboard, although there are airlines that offer this service.
POCs are considered assistance articles and they are not affected by carry-on luggage limits. They should be able to fit under the seat or in the overhead bin. Some seat restrictions may apply in order to meet certain FAA security regulations and those of other competent authorities. As a general rule, there is no electrical supply to the seats on planes for portable oxygen concentrators. Therefore, patients should have an appropriate supply of fully charged batteries for the flight plus an additional 3h of battery time. It is necessary to not that batteries with a lithium content of up to 8g can be transported without restrictions with regards to quantity, but only 2 units with 8–25g of lithium are allowed (with individual protection against short-circuiting).25,26
Nevertheless, depending on the airlines and on the type of plane, there may be electrical outlets in the bathrooms. There are also usually outlets for the cleaning personnel to plug in the vacuums, but they are not always in places that are accessible to passengers. If they are located in the galley, they may or may not be available for passenger use. On larger airplanes, the outlets are usually more accessible to passengers and newer planes have outlets in the seats in business or first class (Fig. 7). An important factor to keep in mind is the type of socket, which may be incompatible with the European system, or vice versa. In the terminals, there are usually outlets which passengers may use to top off the battery charge of the POC before boarding the aircraft.
Oxygen Therapy Outside the HomeDay Outings- •
Oxygen therapy at work: Patients who use HOT and are still actively working need to have O2 sources that meet their needs at home, during their commute to work and during the work day. With the lack of duplicity of the systems, liquid O2 is not a valid alternative, given the autonomy of the carry packs. In this situation, POC stands out as having the advantage of there being electrical outlets available at work.
- •
Oxygen therapy at day centers: A growing number of patients with HOT participate in activities at day centers. Many of these centers request a stationary O2 concentrator for the patient in their installations, but others do not provide that possibility and the patient should carry their own oxygen therapy equipment. As in the previous section, liquid O2 shows its limitations and POC has the advantage of being able to use the outlets at the center. The alternative for certain patients of having a stationary concentrator at home and another at the day center may be considered, although this would mean duplicating the O2 sources of that patient.
- •
Activities away from home: Activities such as shopping, cinema, theater, and eating out with a duration of no more than 4h may be done with liquid O2 and POC. Currently, outings that surpass the autonomy of the liquid O2 systems can only be done with POC. It is easy to find outlets in restaurants, cinemas and shopping centers to recharge the POC.
In this situation, it is necessary to differentiate between outings with a final destination and outings with itinerant destinations.
- ∘
Trips with a final destination: In this situation, the destination becomes our residence during a certain period of time (one week, one month). The standard practice is to continue with the same HOT in the new home with the same criteria with which the HOT source was selected originally, i.e. with stationary or portable sources.
- ∘
Trips with itinerant destinations: In this case, the situation is different, as the stationary sources are ruled out. Except for the exception of a cruise, where it is the hotel itself that moves, the other possibilities for traveling (by car, bus, train or plane) are a serious obstacle for liquid O2. In these situations, POC provides clear advantages over liquid O2.
A frequent situation is that of patients who alternate between two homes. This model of alternance can mean being at the primary residence during the week and spending the weekends at the home of a relative, country home, village or other secondary residence. This situation may also be reversed: helping a child during the week to take care of the grandchildren, for instance, and returning to the primary home on the weekend. These circumstances have usually been dealt with by installing two HOT systems, one at each of the residences, even though this possibility is not contemplated by the administration. Some patients opt to have a stationary concentrator that they themselves or their families move each week from one house to the other, despite the opposition of the medical supply companies. Having family members move liquid O2 is more complicated, and it therefore is not a recommended source for oxygen therapy under these circumstances. POC seems to have a clear advantage in this situation as it can be moved without any problems from one residence to another.
Final CommentsTo summarize, the vertiginous advances in technology give us the possibility to guarantee patients an adequate O2 supply in practically any scenario possible. But, this entails new problems for selecting the O2 source. The mobility allowed by the source should be compatible with the patient mobility profile. The correct indication of HOT, the selection of an adequate source and O2 titration necessary for the patient are the three components that we should contemplate when prescribing home oxygen therapy. As a general rule, liquid oxygen equipment could be useful for activities that take less than 4h, while POC is the choice for activities that take longer. Finally, the patient should have the last word and should commit to using O2 properly.27
Conflict of InterestsThe authors declare having no conflict of interests.
Please cite this article as: Díaz Lobato S, Mayoralas Alises S. Perfiles de movilidad de los pacientes con oxigenoterapia crónica domiciliaria. Arch Bronconeumol. 2011;48:55–60.