In recent decades, we have witnessed a boom in esthetic medicine, the greatest exponent of which is the silicone prosthesis. The most widely used silicone is a highly stable and non-immunogenic polydimethylsiloxane polymer. Even so, this material has been associated with complications that, while rare, can be life-threatening.
Most complications have been associated with the injection of liquid silicone, a substance that has been prohibited by national and international regulatory authorities. The US Food and Drug Administration, for example, issued a safety alert banning its use as of 2017.1 Complications caused by the rupture of silicone gel prostheses are extremely rare.
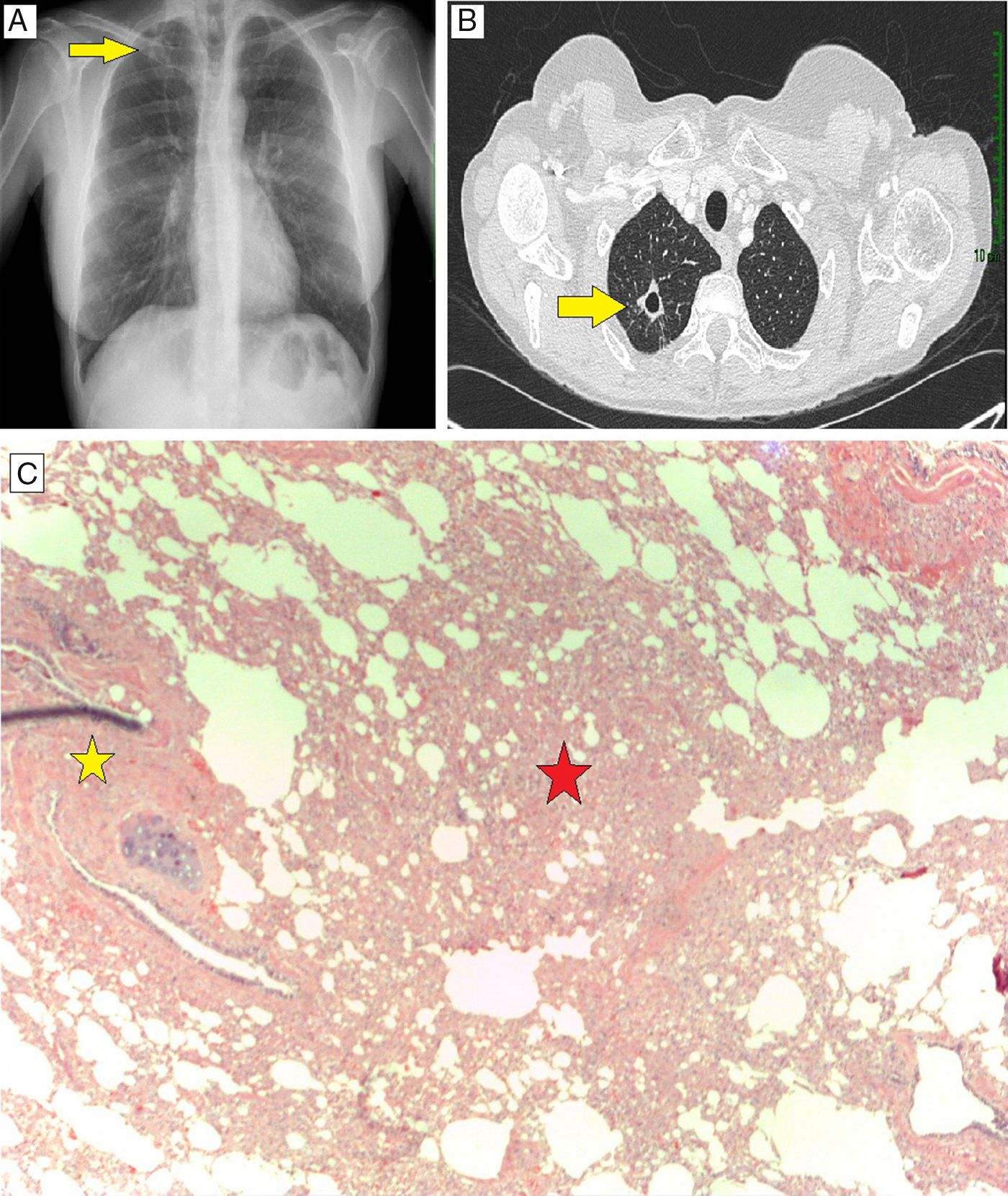
We report the case of a 47-year-old woman, never smoker, with symptoms of cough and bloody sputum lasting several weeks. She did not report fever or asthenia, anorexia or weight loss. Chest X-ray revealed a cavitary lesion in the right upper lobe (RUL) (Fig. 1A). No signs of infection were found on clinical laboratory tests. Chest computed tomography showed a cavitary lesion in the RUL measuring 15×16mm (Fig. 1B), with no other findings. Bronchoscopy was performed and revealed no signs of malignancy. Cultures were negative. PET/CT showed lesion uptake with a SUVmax of 1.08, which rose to 1.14 during the dual-time-point study, so low-grade tumor disease could not be ruled out.
Pulmonary siliconoma. (A) Chest X-ray, PA projection, showing cavitary lesion in RUL, superimposed on clavicle and arch of the second rib. (B) Chest CT axial slice showing cavitary lesion measuring 15×16mm in RUL. (C) Histological specimen of surgical lung biopsy, hematoxylin-eosin staining 40×. Lymphohistiocytic infiltrate with multinucleated cells (red star). Foreign body, remains of silicone polymers (yellow star).
We proceeded with segmental resection of the lesion by video-assisted thoracoscopy. The surgical specimen was found to be a chronic inflammatory infiltrate, predominantly lymphohistiocytic with multinucleated giant cells, with the presence of a foreign body consistent with silicone (Fig. 1C).
The patient was interviewed again, and reported that she was a devotee of esthetic surgery. In 2012, she received her first breast implants that were removed 6 months later after one ruptured.
The results of the pathology report and the patient's history suggested a diagnosis of secondary reaction to migration of material from the ruptured prosthesis, and a conservative approach was taken. No new lung lesions appeared in successive radiological follow-ups.
The interest in this case lies in its exceptional nature. Complications derived from the rupture of silicone breast implants are rare and mostly local. Lung involvement is unusual, and can occur as an embolism, pneumonitis, or siliconomas, which are lesions resulting from a foreign-body reaction to silicone remains that can appear around the prosthesis or in any part of the body due to migration of the material. Silicone is believed to reach the lung by the hematogenous or lymphatic route, where it then manifests in the forms described above.2
The first cases of silicone pneumonitis were described in 1975,3 and similar cases caused by subcutaneous injections of liquid silicone have appeared since then,4,5 all of which involved embolism or pneumonitis. No cases of pulmonary siliconoma such as ours have been described in the literature.
Please cite this article as: Muñiz González F, Hermoso Alarza F, Cano Aguirre MdP. Siliconoma pulmonar, una rara complicación de rotura de prótesis mamaria. Arch Bronconeumol. 2018;54:580–581.