In recent years, pulmonary diseases (LD) such as pulmonary arterial hypertension (PAH), interstitial lung disease (ILD) and pulmonary alveolar proteinosis (PAP) have been reported as life-threatening complications of systemic juvenile idiopathic arthritis (sJIA). In sJIA-LD, a cytokine storm caused by interleukin (IL)-18 and interferon (IFN)-γ is considered to affect the differentiation of lung macrophages. Potential new therapeutic options have included janus kinase inhibitors effective on IFN-γ-induced pathways. We report a rare case of sJIA-LD and its treatment with januse kinase inhibitors.1
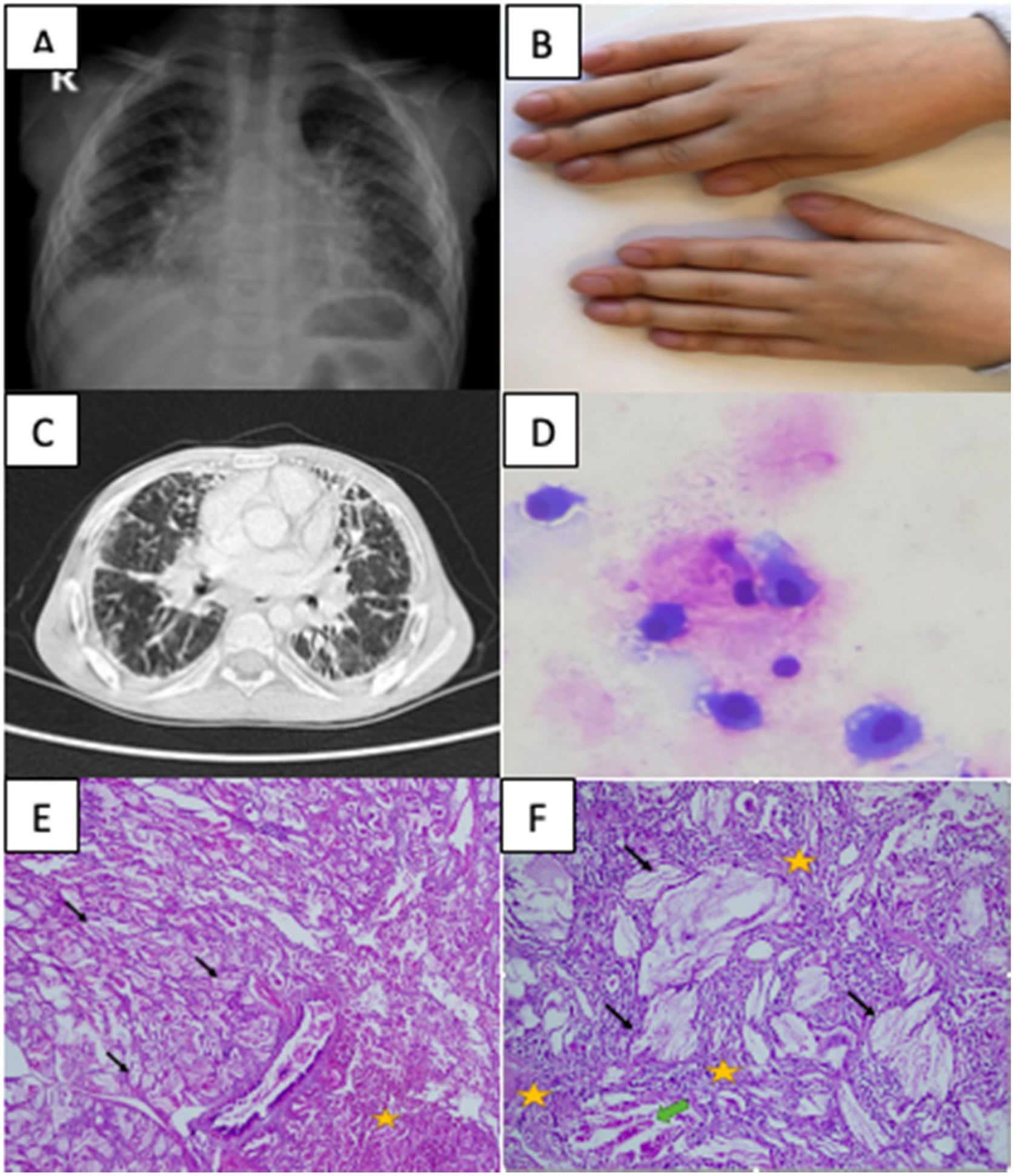
A 2-year-old male patient presented with fever for the last 15 days, maculopapular rashes and right knee swelling. Physical examination revealed right knee arthritis and splenomegaly. Laboratory tests showed leukocytosis, thrombocytosis, anemia and elevated acute phase reactants. Infections and malignancy were excluded. Based on persistent fever, maculopapular rash, arthritis, splenomegaly the patient was diagnosed with sJIA according to the International League of Associations for Rheumatology (ILAR) criteria.2 Steroid treatment was started. Due to the recurrence of fever and elevated ESR and CRP in the patient's clinical progression despite having initially responded to steroid, anakinra (1–2mg/kg/day) was incorporated into his treatment. Anakinra was switched to canakinumab (4–8mg/kg/month) because of the difficulties experienced with daily injections. In 1 year and 6 months the disease was clinically and laboratory activated three times. His follow-ups were interrupted by his parents during the COVID-19 pandemic. After 19 months, he was admitted with complaints of fever, rash, cough, swelling fingers. The patient had maculopapular rashes in the extremities, hepatosplenomegaly, reduced respiratory sounds in the lower zones of the lungs, widespread rales, and clubbing (Fig. 1). There was no need for respiratory support. Oxygen saturation measurement by pulse oximetry was 98%. His posteroanterior thorax radiography revealed diffuse bilateral reticular opacity increase (Fig. 1), and thoracic computed tomography (CT) showed diffuse interlobular septal thickening, fibroelectatic retractions, honeycomb pattern, peribronchovascular thickening and pleural effusion (Fig. 1). Bronchoalveolar lavage (BAL) infection screens were negative. BAL cytology showed lipid-laden macrophages with PAS staining, suggesting PAP. Lung biopsy showed interstitial fibrosis in the subpleural area and cholesterol clefts in the alveoli. Granuloma, lymphoid aggregates, follicular bronchiolitis-like morphology were not detected (Fig. 1). The findings were diagnosed as sJIA-LD. The limitations of our report include the fact that IFN signature, IL-18 levels and lymphocyte subgroups in BAL cytology were could not be measured. Pulse methylprednisolone was started and treatment was continued with 2mg/kg/day prednisolone. Canakinumab was discontinued and tofacitinib (5mg/day) was started. At 1 month of tofacitinib treatment, there were significant improvements in effort dyspnea and cough. In the fifth month of tofacitinib treatment despite thoracic tomography showing no significant regression in pathologic findings except pleural effusion, the patient was asymptomatic and respiratory sounds were normal. The patient's follow-up continues with tofacitinib and steroids.
(A) Chest X-ray image showing diffuse bilateral reticular opacity increase. (B) Clubbing image of sJIA-LD patient. (C) High resolution computed tomography image showing diffuse interlobular septal thickening, fibroelectatic retractions, honeycomb pattern, peribronchovascular thickening. (D) Bronchoalveolar lavage cytology image showing lipid-laden macrophages with PAS staining. (E) Lung biopsy pathology image showing cholesterol clefts (black arrows), interstitial fibrosis, and chronic inflammation (yellow stars) in lung parenchyma (hematoxylin and eosin stain, 40×). (F) Lung biopsy pathology image showing cholesterol clefts (black arrows), interstitial fibrosis, and chronic inflammation (yellow stars), and multinucleated giant cells (green arrow) with higher magnification (hematoxylin and eosin stain, 100×).
In conclusion, sJIA-LD is a life-threatening complication with unclear treatment options and a poor prognosis. Our patient had multiple risk factors that may lead to sJIA-LD, including early age, recurrent macrophage activation syndrome attacks, IL-1 inhibitor usage, and uncontrolled systemic inflammation.3,4 It is very important to keep in mind that LD may develop in patients with sJIA who have similar risk factors. Potential new treatment options are janus kinase inhibitors acting on IFN-γ-induced pathways.
Informed ConsentWritten informed consent was obtained from the parents for publication of this case report and any accompanying images.
FundingAn honorarium, grant, or other form of payment was not given to any author to produce the manuscript.
Authors’ ContributionsAll authors made substantial contributions to the conception or design of the work, have approved the final manuscript, and takes full responsibility for the manuscript. MMK, EC reviewed and revised the manuscript, MMK, EC and GC contributed to the writing of the manuscript.
Conflict of InterestNone declared.
We would like to thank Banu Çelikel Acar, Diclehan Orhan and Salih Uytun for their valuable contributions.