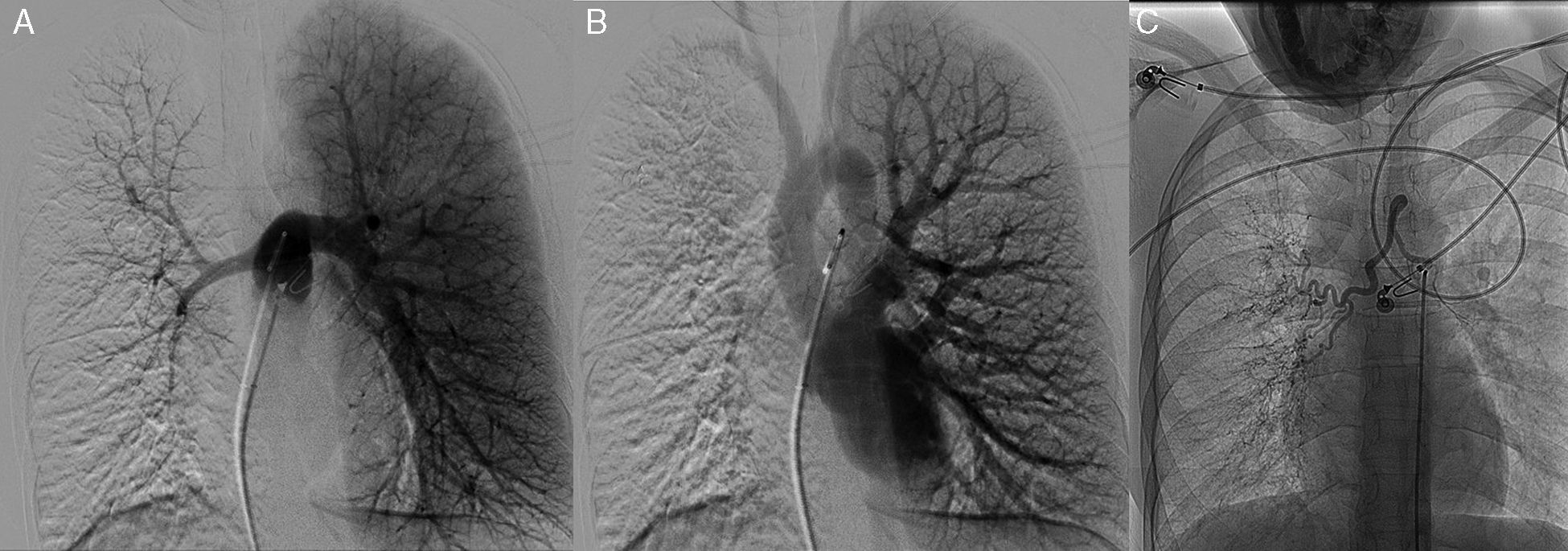
We present the case of a 19-year-old woman, smoker (8 pack-years), and regular cannabis user, with a history of severe bronchitis in childhood and frequent respiratory infections. She presented for episodes of coughing with hemoptoic expectoration since she was 15-years-old. The episodes were initially sporadic, but had become more frequent in recent months, sometimes occurring every 48h. On examination, she had decreased breath sounds in the right hemithorax, and acropachy. The chest radiograph showed loss of volume in the right lung and attenuation of the right hilum. The right pulmonary veins could not be identified on computed tomography (CT), and a diffuse increase in density was observed in the affected lung. Cardiac magnetic resonance imaging (MRI) ruled out associated heart disease, and the echocardiography ruled out pulmonary hypertension. Pulmonary arteriography was performed (Fig. 1A and B), in which hypoplasia of the right pulmonary artery and absence of right pulmonary venous return were observed. Arteriography of the thoracic artery (Fig. 1C) showed right bronchial artery hypertrophy originating in the descending aorta. Lung function test results were: FEV1: 2.040 (75.5%), FVC: 2.800 (90.1%) and DLCOc SB: 69.3%. Varices were observed in the distal trachea and start of the right main bronchus on fiber optic bronchoscopy. Considering the previous findings, we opted for surgical treatment, specifically, right pneumonectomy. The immediate post-operative period was uneventful, and the patient is currently asymptomatic.
Pulmonary arteriography showing hypoplasia of the right pulmonary artery, providing little perfusion, almost entirely limited to the upper lobe (A), in which right venous drainage cannot be seen (B). Arteriography of the thoracic aorta showing an irregular, winding bronchial artery with origin in the anterior superior side of the descending thoracic aorta (C).
Unilateral pulmonary vein atresia is a rare condition that is associated with congenital cardiac malformations in 32% of cases.1 It is usually diagnosed in childhood and, if untreated, can be fatal in as many as 50% of cases.2 Recurrent lung infection and dyspnea on exertion are the most common manifestations. Rupture of bronchial varices can sometimes cause hemoptysis, and therefore bronchoscopic findings may be of interest when this condition is suspected. CT and MRI are useful diagnostic tools, although definitive diagnosis is provided by pulmonary arteriography. Arteriography of the thoracic aorta and selective arteriography of the bronchial arteries enable the origin and anatomical distribution of collateral branches to be identified. Pneumonectomy is considered the treatment of choice in cases that present with pulmonary hypertension, recurrent infections or significant hemoptysis. This eliminates the focus of the infections, the left-right shunt and the dead space that contributes to exercise intolerance.3 Reparatory surgery can be considered in cases detected at a young age. Embolization of the bronchial artery has been described in an adult patient whose only symptom was hemoptysis.4 Conservative treatment and follow-up may be the management of choice in asymptomatic patients without pulmonary hypertension.5 In our case, repeated hemoptysis, the history of frequent respiratory infections and prevention of pulmonary hypertension prompted us to choose resection of the affected lung in this patient.
FundingNone.
Conflict of InterestsThe authors state that they do not have any conflicts of interest directly or indirectly related with the contents of the manuscript.
Please cite this article as: Gómez Hernández MT, Rodríguez Pérez M, Jiménez MF. Atresia aislada unilateral de venas pulmonares en el adulto. Arch Bronconeumol. 2015;51:424–425.