Despite the administration of appropriate treatment, a high number of patients with asthma remain uncontrolled. This suggests the need for alternative treatments that are effective, safe and selective for the established asthma phenotypes, especially in patients with uncontrolled severe asthma. The most promising options among the new asthma treatments in development are biological therapies, particularly those monoclonal antibodies directed at selective targets.
It should be noted that the different drugs, and especially the new biologics, act on very specific pathogenic pathways. Therefore, determination of the individual profile of predominant pathophysiological alterations of each patient will be increasingly important for prescribing the most appropriate treatment in each case. The treatment of severe allergic asthma with anti-IgE monoclonal antibody (omalizumab) has been shown to be effective in a large number of patients, and new anti-IgE antibodies with improved pharmacodynamic properties are being investigated.
Among developing therapies, biologics designed to block certain pro-inflammatory cytokines, such as IL-5 (mepolizumab) and IL-13 (lebrikizumab), have a greater chance of being used in the clinic. Perhaps blocking more than one cytokine pathway (such as IL-4 and IL-13 with dulipumab) might confer increased efficacy of treatment, along with acceptable safety.
Stratification of asthma based on the predominant pathogenic mechanisms of each patient (phenoendotypes) is slowly, but probably irreversibly, emerging as a tailored medical approach to asthma, and is becoming a key factor in the development of drugs for this complex respiratory syndrome.
Un porcentaje elevado de pacientes con asma no está controlado, incluso a pesar de seguir un tratamiento adecuado. Esto indica que son necesarios tratamientos alternativos que sean eficaces, seguros y selectivos para los fenotipos de asma descritos, especialmente en pacientes con asma grave no controlada. De los nuevos tratamientos en desarrollo para el asma, las opciones más prometedoras son las terapias biológicas, en particular los anticuerpos monoclonales frente a dianas selectivas.
Es importante tener en cuenta que los diferentes fármacos, pero especialmente los nuevos tratamientos biológicos, actúan sobre vías patogénicas muy específicas, y por lo tanto cada vez va a ser más importante determinar el perfil individual de alteraciones fisiopatológicas predominante en cada paciente para prescribir el tratamiento más adecuado en cada caso. El tratamiento del asma grave alérgica con un anticuerpo monoclonal anti-IgE (omalizumab) ha mostrado ser eficaz en un número elevado de pacientes, y nuevos anticuerpos anti-IgE con mejores propiedades farmacodinámicas están siendo investigados.
Entre las terapias en desarrollo, los medicamentos biológicos dirigidos a bloquear ciertas citoquinas proinflamatorias, como IL-5 (mepolizumab) e IL-13 (lebrikizumab), son los que tienen más visos de ser utilizados clínicamente. Tal vez el bloqueo de más de una vía de citoquinas (como IL-4 e IL-13 con dulipumab) pueda ofrecer una mayor eficacia del tratamiento, junto con una seguridad aceptable.
La estratificación de asma en función de los mecanismos patogénicos predominantes en cada paciente (fenoendotipos) está abriendo paso, de forma lenta pero probablemente irreversible, a la medicina personalizada para el asma, y se está convirtiendo en un factor clave en el desarrollo de fármacos para este complejo síndrome respiratorio.
Drugs currently used for the treatment of asthma reduce inflammation of the respiratory tract and relieve bronchospasm, but do not offer a cure, so symptoms reappear when treatment is discontinued. International1 and national2 guidelines for the management of asthma underline the importance of effective treatment for achieving and maintaining control. Despite the wide availability of effective treatments, and uniform treatment guidelines,1,2 achieving control of their asthma remains a constant challenge for many patients. Recent studies indicate that over 50% of patients with asthma are not controlled,3,4 even on regular maintenance treatment with a combination of inhaled corticosteroids (IC) and a long-acting beta-2 agonist (LABA).5
These data suggest that there is a need for alternative treatments, particularly for patients with severe uncontrolled asthma. However, it is important to remember that different drugs, particularly biologics, act on specific pathogenic pathways, so the individual profile of the predominant physiopathological alterations of each patient must be determined in order to prescribe the most appropriate treatment in each case.6
Asthma management, both current and future, must include the stratification of patients into the recently defined phenotypes (clinical, inflammatory, molecular)7 and endotypes (allergic asthma, aspirin-sensitive asthma, late-onset hypereosinophilic asthma, etc.)8 that can be grouped under “phenoendotypes”. Moreover, in the last 10 years, significant efforts have been made to identify the characteristics that differentiate severe asthma from mild to moderate asthma, preparing the ground for the development of new selective treatments.
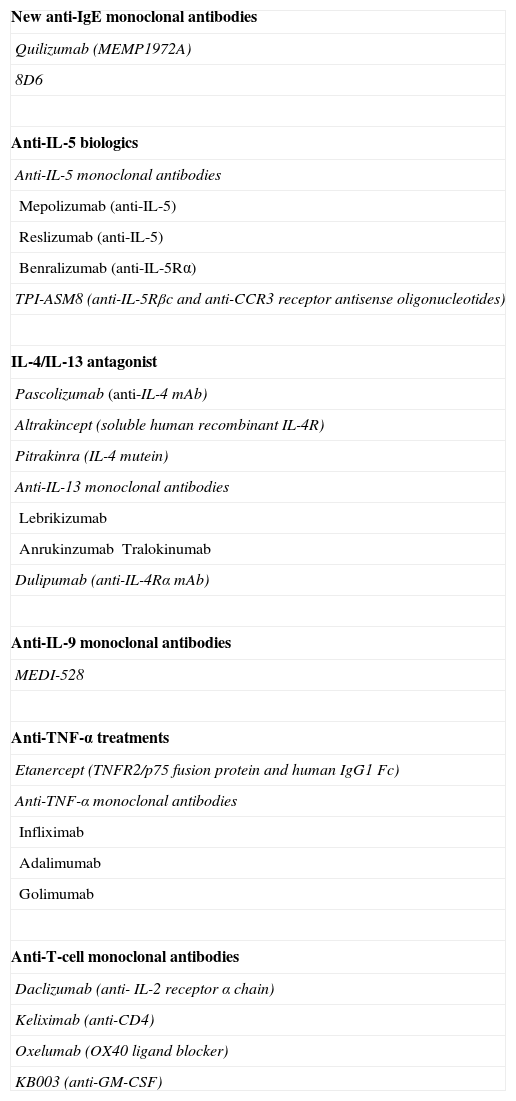
Among the new asthma treatments the most promising are biological therapies, and in particular, selectively targeted monoclonal antibodies (mAb).9 Biologics at a more advanced stage of development are reviewed below (Table 1), some of which, such as the new anti-IgE, anti-IL-5 and anti-IL-13 mAbs, may find their place in clinical practice in the not too distant future.
Biologics Currently Under Development for the Treatment of Asthma.
| New anti-IgE monoclonal antibodies |
| Quilizumab (MEMP1972A) |
| 8D6 |
| Anti-IL-5 biologics |
| Anti-IL-5 monoclonal antibodies |
| Mepolizumab (anti-IL-5) |
| Reslizumab (anti-IL-5) |
| Benralizumab (anti-IL-5Rα) |
| TPI-ASM8 (anti-IL-5Rβc and anti-CCR3 receptor antisense oligonucleotides) |
| IL-4/IL-13 antagonist |
| Pascolizumab (anti-IL-4 mAb) |
| Altrakincept (soluble human recombinant IL-4R) |
| Pitrakinra (IL-4 mutein) |
| Anti-IL-13 monoclonal antibodies |
| Lebrikizumab |
| AnrukinzumabTralokinumab |
| Dulipumab (anti-IL-4Rα mAb) |
| Anti-IL-9 monoclonal antibodies |
| MEDI-528 |
| Anti-TNF-α treatments |
| Etanercept (TNFR2/p75 fusion protein and human IgG1 Fc) |
| Anti-TNF-α monoclonal antibodies |
| Infliximab |
| Adalimumab |
| Golimumab |
| Anti-T-cell monoclonal antibodies |
| Daclizumab (anti- IL-2 receptor α chain) |
| Keliximab (anti-CD4) |
| Oxelumab (OX40 ligand blocker) |
| KB003 (anti-GM-CSF) |
mAb: monoclonal antibody; GM-CSF: granulocyte and macrophage colony stimulating factor; IL: interleukin; TNF-α: tumor necrosis factor α.
Protein–protein interaction between IgE and its high-affinity receptor (Fc¿RI) is a key component in the allergic response. At present, omalizumab is the only mAb approved for the treatment of asthma. Clinical studies in omalizumab have further defined the role of IgE in allergic asthma. Moreover, it is important to take into consideration certain entities in which IgE may also play a part even if allergic etiology is not well established, such as nasal polyposis or non-allergic asthma. Nasal polyposis may be present in asthma with or without concomitant atopy, but it is particularly associated with non-allergic aspirin-sensitive asthma, and is one of the most common comorbid conditions in patients with severe asthma. Most studies on the pathogenesis of nasal polyposis show inflammatory eosinophilic proliferation and elevated local IgE, in addition to elevated degranulated mast cells. Omalizumab has shown clinical efficacy in the treatment of polyposis in patients with asthma, suggesting that local production of IgE in the respiratory tract may be important in these patients.10,11
In non-allergic asthma, the bronchial inflammatory process, while not fully clarified, appears to resemble that of allergic asthma, with an increase in Th2 lymphocytes, mast cell activation and eosinophil infiltration. The lack of therapeutic alternatives in these patients occasionally means that omalizumab for “compassionate use” is prescribed. Two preliminary studies12,13 have shown that omalizumab is effective in the treatment of non-allergic asthma.
New anti-IgE molecules, discussed below, are being developed that will probably be superior to the currently available agent. A new human anti-IgE mAb (8D6) possesses a unique set of binding specificities. This mAb binds to a conformational epitope on the CH3 domain of human IgE and can compete with omalizumab for IgE binding.14 Like omalizumab, 8D6 does not bind to IgE already bound to the high-affinity IgE receptor (Fc¿RI) on basophils and mast cells, but unlike omalizumab, it can bind to IgE already bound to the low-affinity receptors (Fc¿RII or CD23).14 Since previous studies have shown that anti-CD23 mAb can inhibit IgE synthesis in in vitro lymphocyte cultures and inhibit IgE production, 8D6 may offer pharmacological mechanisms in addition to those mediated by omalizumab for the neutralization of IgE.
Quilizumab (MEMP1972A, Genentech/Roche) is another anti-IgE mAb currently under study in a phase IIb, randomized, double-blind, placebo-controlled clinical trial to evaluate the efficacy and safety of 3 doses (150, 300 and 450mg subcutaneously) in adults with allergic asthma not controlled with IC and a second maintenance medication (NCT01582503).
Using small molecules to inhibit the IgE–Fc¿RI receptor interaction is an attractive strategy in the treatment of allergic diseases. Cyclic peptides and small proteins that interfere with the IgE–Fc¿RI system are under development and may be effective in this area.15
Anti-IL-5 BiologicsInterleukin (IL)-5 is a hematopoietic cytokine produced by various cells such as Th2 lymphocytes, eosinophils, basophils, mast cells and natural killer T-cells, and is the main eosinophil modulator cytokine.16 IL-5 enhances eosinophil chemotaxis, activation and degranulation, while reducing apoptosis and prolonging survival. The IL-5 receptor (IL-5R) is expressed on both basophils and eosinophils and is made up of 2 subunits: an α-subunit (IL-5Rα) that is IL-5-specific and a βc-subunit (IL-5Rβc) that is responsible for signal transduction and is shared with the specific α-receptor subunits of IL-3 receptors and granulocyte and macrophage colony stimulating factor (GM-CSF).16
Two mAbs (mepolizumab and relizumab) that neutralize IL-5 and another mAb (benralizumab) that blocks the IL-5Rα17 have been developed and are still under evaluation.
MepolizumabMepolizumab in a fully humanized anti-IL-5 IgG1 mAb that binds to free IL-5 with high affinity and specificity for preventing this IL from binding with the α chain of the IL-5 receptor on the eosinophil cell surface.
It was the first IL-5 antagonist used in randomized, controlled trials in patients with mild asthma18,19 and moderate uncontrolled persistent asthma.20 A reduced eosinophil count was observed in both sputum and peripheral blood,18,19 in bronchial biopsies and in bone marrow,19 but with no effect on bronchial hyperresponsiveness (BHR),18,19 late asthmatic response,18 lung function,19,20 symptoms or use of rescue medication20 was reported. There was a reduction in the percentage of exacerbations,20 but statistical significance was not reached.
These studies were criticized because patients were not selected according to the presence of eosinophilic airway inflammation, and the number of exacerbations, a parameter directly and causally related with eosinophilic airway inflammation, which was not evaluated as the principal variable of treatment response.16 Two new trials were subsequently performed in patients with refractory severe persistent asthma with recurrent exacerbations who had bronchial eosinophilic inflammation.21,22 Both trials reported a very significant reduction in the number of exacerbations and in the dose of oral corticosteroids used by treated patients compared to those in the placebo group, as well as a major improvement in asthma control questionnaire (ACQ) scores. This clinical response was accompanied by a significant reduction in eosinophil numbers in blood and sputum. The degree of methacoline HRB was not affected and there was little21 or no22 improvement in FEV1.
A phase IIb multicenter study (GlaxoSmithKline) has recently been performed to determine the optimal dose of mepolizumab and to confirm its efficacy and safety in patients with severe eosinophilic asthma (DREAM study).23 A total of 621 patients were randomized to placebo or 1 of 3 mepolizumab doses (75, 250 or 750mg) in parallel groups for 1 year. Mepolizumab reduced the number of severe exacerbations by around 50% in all mepolizumab groups compared to placebo, irrespective of the dose, and no dose–response effect was reported. The eosinophil count in blood and sputum was also reduced, and a dose–response effect was observed for eosinophil counts in sputum. There were no changes in asthma symptoms, quality of life, FeNO or lung function. The drug was safe and effective. A multivariate analysis established that only the level of blood eosinophilia and the number of exacerbations in the 12 months prior to the study were associated with response to mepolizumab.
Finally, a meta-analysis performed on published clinical trials with mepolizumab, including a total of 1131 patients, confirmed that in cases of eosinophilic asthma, mepolizumab reduced the number of exacerbations and improved asthma-related quality of life.24
ReslizumabReslizumab, a humanized IgG2, is another IL-5 inhibitor that, like mepolizumab, is administered intravenously, although it has not been studied in such depth. In the only published clinical trial in patients with poorly controlled eosinophilic asthma, patients treated with reslizumab showed a significant improvement in FEV1 and patients with concomitant polyposis showed better asthma control compared to the placebo group.25
BenralizumabBenralizumab is a humanized IgG1 mAb targeting the IL-5Rα that reduces eosinophilia by antibody-dependent cell-mediated cytotoxicity. Intravenous benralizumab has shown acceptable safety and tolerability in a phase I, dose-escalating study, with a marked reduction in circulating eosinophils, reaching lowest levels after 24h with a response of up to 8–12 weeks.26
In a recent phase I multicenter, double-blind, placebo-controlled study, 13 patients were randomized to receive a single intravenous dose of placebo or 1mg/kg benralizumab and 14 patients were randomized to receive a monthly subcutaneous dose of placebo, or 100 or 200mg benralizumab for 3 months. The study concluded that both the single intravenous dose and the multiple subcutaneous doses of benralizumab reduced the percentage of eosinophils in the airway mucosa and submucosa and in sputum and suppressed eosinophil levels in the bone marrow and peripheral blood.27
The safety profile of this study supports the development of this molecule, but additional studies are required for evaluating its clinical benefit in asthmatic patients.
Other Anti-IL-5 BiologicsTPI-ASM8 is a new anti-IL-5 treatment. It consists of 2 antisense oligonuclueotides that target IL-5Rβc and the CCR3 chemokine receptor expressed by various leukocytes, including eosinophils, basophils and Th1 and Th2 lymphocytes.28
In patients with allergic asthma, TPI-ASM8 reduced allergen-induced eosinophilic inflammation29 and eosinophil progenitor levels in sputum,30 and has been shown to be safe and well-tolerated at various doses.31
By inhibiting the intracellular portion of the IL-5R, benralizumab would block the signal transduction of IL-5, IL-3 and also GM-GSF. TPI-ASM8, by inhibiting a wider range of inflammatory cells, could in theory have a greater immune impact than anti-IL-5 mAb in the treatment of asthma, although this remains to be confirmed.
Finally, a small interfering RNA (siRNA), a class of bicatenary RNA that interferes in the expression of specific genes, has been used in animal models to inhibit IL-5 but no studies in humans have been developed to date.32
Anti-IL-4 and Anti-IL-13 TreatmentsIL-4 and IL-13 are important therapeutic targets in asthma due to their significant role in Th2 lymphocyte responses and in B lymphocyte isotype switching for IgE synthesis, and also for their intervention in mast cell selection. Given the diverse actions of this pathogenic pathway in asthma, with strong evidence of its involvement from genetic studies and the convincing data regarding its involvement from animal studies, a wide range of biological agents aimed at these targets has been developed, including anti-IL-13, anti-IL-4Rα and anti-IL-13Rα1 mAbs, IL-4Rα/IL-13Rα1 fusion protein, IL-4/IL-13 vaccines, anti-IL-4Rα antisense oligonucleotides and double mutein IL-4.33 However, although many of these drugs are under development, to date only a few have been evaluated in asthmatic patients.
Anti-IL-4 Monoclonal AntibodiesDespite its safety and efficacy in non-human primates,34 the anti-IL-4 antibody pascolizumab (Biopharma) did not show any clinical benefit in a 6-month clinical trial in steroid-naïve patients with uncontrolled asthma.35
Human Soluble IL-4RSoluble IL-4R (sIL-4R) is a naturally secreted form of IL-4R that contains the extracellular portion of the IL-4Rα chain, allowing it to bind to IL-4 and neutralize its action. An inhaled human recombinant sIL-4R, altrakincept, designed to block the interaction between IL-4 and its cellular receptors, has been tested in phase I–II trials. In patients with moderate persistent asthma, administration of altrakincept by nebulation was initially shown to inhibit any increase in asthma symptoms and reductions in FEV1, allowing IC doses to be decreased.36,37 However, its efficacy could not be confirmed in a subsequent phase II study in moderate persistent asthma,38 perhaps due to biodegradation and poor bioavailability in the respiratory tract.
Anti-IL-13 Monoclonal AntibodiesSeveral anti-IL-13 mAb have entered clinical trials in humans, including IMA-026, IMA-638 (anrukinzumab), QAX576, 354-CAT (tralokinumab) and MILR 1444A (lebrikizumab).
Anrukinzumab has been tested in patients with mild allergic asthma in studies including allergen-induced challenge, in which a small but significant reduction in both immediate and late asthmatic responses was found at 14 days but not at 35 days after administration.39 In a 12-week study in patients with uncontrolled persistent asthma, anrukinzumab did not show any efficacy,40 and its development for the treatment of asthma was discontinued.
Corren et al.41 studied the effects of lebrikizumab in 219 adults with moderate to severe persistent uncontrolled asthma despite IC, 80% of whom were also treated with LABA. Lebrikizumab was administered subcutaneously every month for 6 months. A significant improvement of 5.5% in prebronchodilator FEV1 was recorded at 12 weeks in patients treated with lebrikizumab compared to the placebo group. The effect was significantly greater in patients with pre-treatment circulating periostin levels above the median and also in those with Th2-high phenotype (total IgE>100IU/ml and eosinophilia>140/mm3), compared to those with Th2-low phenotype. Exacerbations were not significantly reduced in the active group compared to placebo, but in the Th2-high subgroup, the rate of exacerbations was 60% lower in patients receiving lebrikizumab compared to placebo.41 These data suggest that therapy with anti-IL-13 antibodies may be more effective when directed at a selected subgroup of patients (Th2-high phenotype).
IL-4Rα Activity InhibitionDue to the partial overlap in the functions of IL-4 and IL-13, it appears logical to develop drugs that can inhibit the activity of both. A bioengineered IL-4 mutein has been generated that acts as an antagonist by inhibiting the binding of IL-4 and IL-13 to the shared IL-4Rα/IL-13Rα1 complex.42 After testing the safety and bioavailability of subcutaneous and inhalation administration, this mutein (pitrakinra, AER 001, BAY-16-9996) was found to be effective via both routes for immediate and late asthmatic allergen-induced responses, but not for the subsequent increase in HRB.43
A phase IIb, double-blind, randomized, placebo-controlled, parallel-group study has been performed with repeated doses of inhaled pitrakinra (Aerovant™ AER 001 powder for inhalation) in adult patients with moderate to severe asthma.44 The hypothesis was that Aerovant™ would improve asthma symptom control and would reduce the need for IC and LABA, reducing exacerbations compared to placebo. In 534 patients with asthma not controlled with IC no benefit was found in the overall population of asthma patients, but in a subgroup of 125 patients with eosinophilic asthma the rate of exacerbations fell by 37% with the highest of the 3 doses used in the study (10mg twice a day).44 One factor influencing the response to this IL-4R antagonist is the mutation in the IL-4Rα chain.
Dupilumab (Sanofi) is a humanized mAb that targets the α-subunit of the IL-4 receptor that is shared with IL-13. In a phase IIA, randomized, double-blind, placebo-controlled study, the efficacy and safety of dupilumab in the treatment of patients with persistent eosinophilic asthma were evaluated.45 This study included 105 patients with moderate to severe persistent asthma and eosinophilia≥300/mm3 in blood or ≥3% in sputum. All patients were taking moderate to high doses of IC and LABA. They were randomized to receive dupilumab 300mg (n=52) or placebo (n=52) subcutaneously once a week. Treatment lasted 12 weeks or until development of a moderate or severe exacerbation (primary endpoint) on discontinuation of LABA or reduction or discontinuation of IC. Effects on biomarkers associated with Th2 lymphocyte activity were also evaluated.
An 87% reduction in asthma exacerbations was found in the active group (6% with dupilumab vs 44% with placebo); this difference was statistically significant.45 A significant difference in favor of dupilumab in the time until the first exacerbation and the risk of exacerbations was also recorded. There was a significant association between dupilumab and a >200ml increase in FEV1 compared to baseline after the second week. This association was maintained until the end of the study, even during the period of IC and LABA withdrawal. In dupilumab patients, an improvement in morning peak expiratory flow (PEF) and a clinically significant reduction in asthma symptoms evaluated using the ACQ5 were recorded. Nocturnal awakening and the use of short-acting beta-2 agonists were also reduced. The biological activity of dupilumab was reflected in a marked reduction of FeNO and thymus and activation-regulated chemokine (TARC), eotaxin-3 and IgE levels in serum.
With regard to adverse effects, more local reactions at the injection site, nasopharyngitis, nausea and headache were reported in patients on active treatment, and there was one case of angioedema. The authors of this study conclude that the contribution of IL-4 and IL-13 airway inflammation in patients with persistent asthma despite IC treatment is confirmed, and they emphasize the effect of dupilumab on the reduced frequency of exacerbations, even after withdrawal of IC and LABA. Nevertheless, they admit that the definition of exacerbation used in their protocol does not coincide with that used in clinical practice, and accordingly recommend that larger studies should be performed. Other positive findings included improved lung function and the reduction of inflammatory markers.45
Anti-IL-9 Monoclonal AntibodiesIL-9 is a multifunctional cytokine produced by Th2 lymphocytes and mast cells. Expression of IL-9 and its receptor in the respiratory tract has been seen to be greater in asthmatics than in healthy subjects. MEDI-528 is an IgG1 mAb that binds to IL-9, and preliminary studies in healthy subjects and patients with mild and moderate asthma suggest that subcutaneous administration of the drug has an acceptable safety profile and reduces exacerbations and FEV1 after exercise.46 The results of a double-blind study with this mAb in 329 adult asthmatic patients not controlled with medium to high doses of IC were published recently.47 Patients were randomized to four groups–3 active (30, 100 and 300mg) and 1 placebo–and treated every 2 weeks for a period of 24 weeks together with their usual asthma medication. No significant change was found in the asthma control questionnaire scores, exacerbations, lung function or quality of life. Adverse effects were few and generally mild or moderate, occurring at a similar rate in the active and placebo groups.47
Anti-TNF-α for Refractory Asthma and Neutrophilic AsthmaEtanerceptEtanercept is a dimeric protein genetically constructed by fusion of the soluble extracellular domain of the human tumor necrosis factor receptor-2 (TNFR2/p75), bound to the Fc domain of the human IgG1. This fusion protein binds to free TNF-α, thus neutralizing it. In a large randomized, controlled, multicenter study to evaluate the efficacy and safety of this product (25mg twice a week) in patients with moderate to severe persistent asthma, no improvement was reported in any of the asthma parameters.48
Anti TNF-α Monoclonal AntibodiesInfliximab, a humanized mAb, improves PEF circadian variation and reduces asthma exacerbations in patients with moderate persistent asthma,49 but to date the efficacy and safety of infliximab, or of adalimumab, have not been studied in severe chronic asthma. Clinical improvement has been reported in asthmatic patients receiving infliximab for rheumatoid arthritis.50 Recently, a series of seven patients with severe asthma and severe and frequent exacerbations despite treatment with oral corticosteroids and a poor previous response to omalizumab was published. After 3 months of infliximab treatment, patients showed an improvement in the number of exacerbations, oral corticosteroid dose reductions, including total withdrawal in 5 patients, and improved ACT.51 However, 2 patients had allergic reactions to the drug, which was replaced with adalimumab, but 1 had to be withdrawn due to severe pneumonia and another because of dissemination of melanoma. This increased rate of serious adverse effects was also observed in a study with infliximab in chronic obstructive lung disease in which 9 cases of malignant disease were found in the 157 patients on active treatment, and only 1 in the placebo group.52
Only 1 study has looked at long-term treatment with golimumab, an anti-TNF-α mAb for severe asthma, using the exacerbation rate as the primary outcome measure.53 In 309 patients with severe persistent asthma, randomized to receive placebo or 3 different doses of golimumab (50, 100 and 200mg), no significant improvement in any of the efficacy variables was observed. Moreover, the trial had to be prematurely discontinued due to serious adverse events, particularly infections and malignant disease, in the golimumab group. However, a post hoc analysis suggested that patients with a pre-study history of sinusitis and FEV1 reversibility (≥12%) who received golimumab (100 and 200mg) had fewer severe asthma exacerbations, apparently associated with a dose–response effect.
It seems possible that if markers were developed for predicting response to anti-TNF-α agents, they could be used for subgroups of patients with severe asthma, but the contradictory efficacy results and the potential safety concerns have prevented the performance of additional clinical trials.
Anti-T-Lymphocyte Monoclonal AntibodiesRespiratory tract inflammation involves the activation of T-lymphocytes, with an increase in CD25+T-cells and raised IL-2 and soluble (sCD25) IL-2 receptor (IL-2R) α-chain levels.
Daclizumab is a humanized mAb that targets this receptor, impeding it from binding to IL-2 and thus inhibiting its biological activity. It was approved in the United States for preventing rejection in renal transplantation patients. A single study is available of 115 patients with moderate or severe asthma not controlled despite treatment with high dose ICs.54 There were 88 patients in the active group and treatment was administered every 2 weeks for a period of 12 weeks, while 27 received placebo (3:1). During the subsequent 16-week follow-up, discrete but significant improvements were found in lung function parameters (FEV1), daytime asthma symptoms, use of rescue medication and time to first exacerbation. A total of 6 patients had serious adverse effects during the study, 3 of which were directly related to the drug, according to the investigators, including an anaphylactic reaction during the first treatment dose that required adrenaline and intubation, a case of Varicella zoster virus meningitis and a case of breast cancer 4 months after the last dose. The authors remarked that experience with the drug in transplanted patients does not reveal any tendency to increase the risk of severe viral infections, and that anaphylactic reactions with daclizumab are rare, although data supporting the safety of the drug in the treatment of asthma are required.
Prior to this, a randomized, double-blind, placebo-controlled study of keliximab in a small group of 22 patients with corticodependent asthma had been published. Keliximab is an anti-CD4 mAb that has been used in the treatment of rheumatoid arthritis.55 A single dose was administered, but at various concentrations. After 4 weeks of follow-up, the group that received the highest doses showed a significant improvement in maximum PEF, in the reduction of CD4+lymphocytes and in the modulation of the CD4 surface expression, but not in other clinical parameters or in IL-4, IL-5 and IFN-γ. There are no further studies investigating the role of keliximab in asthmatic patients.
A more recent alternative consists of targeting treatment to interfere in the co-stimulation between the dendritic cell and the T-lymphocyte mediated by OX40 and its ligand. A phase II, randomized, double-blind study with oxelumab, a humanized mAb that blocks the OX40 ligand in patients with controlled mild allergic asthma has been designed to evaluate late asthmatic response 16 weeks after administration of the first dose of study drug, although no data have been published to date.56
A phase II study (NCT01603277) expected to conclude in March 2014 is also underway with KB003, an anti-GM-CSF mAb, in patients with moderate to severe asthma not adequately controlled with IC, evaluating changes in FEV1 and the exacerbation rate.
Conclusions and PerspectivesSince therapeutic options in patients with poorly controlled asthma, particularly severe asthma, are limited, it would be desirable to have new selective and clinically effective treatments for the various asthma phenoendotypes. Over the past 10 years, different therapeutic strategies with cytokine-neutralizing drugs have been explored, but to date none has found its way into the therapeutic arsenal. The redundancy and overlapping of many of the pathogenic pathways in asthma could be responsible for the limited efficacy of these treatments. Potential side effects and high production costs are other obstacles in the development of these novel treatments.
However, experience with the anti-IgE mAb omalizumab has been generally positive in patients with severe allergic asthma. It is hoped that blocking or neutralizing other important therapeutic targets in asthma (such as IL-5, IL-4 or IL-13) with selective treatments will achieve positive results, at least in certain patient subgroups (phenoendotypes) and/or some important variables of the asthmatic syndrome (exacerbations, eosinophilic inflammation, lung function, etc.) that will lead to their implementation in clinical practice, notwithstanding other treatment modalities, such as bronchial thermoplasty, that may have a role in some patients with severe asthma.
Conflict of InterestNone.
Please cite this article as: Quirce S, Bobolea I, Domínguez-Ortega J, Barranco P. Futuras terapias biológicas en el asma. Arch Bronconeumol. 2014;50:355–361.