The aim of this study is analysing the impact of the systematic versus occasional videoconferencing discussion of patients with two respiratory referral units along 6 years of time over the efficiency of the in-person outpatient clinics of a thoracic surgery service.
MethodRetrospective and comparative study of the evaluated patients through videoconferencing and in-person first visits during two equivalents periods of time: Group A (occasional discussion of cases) between 2008 and 2010 and Group B (weekly regular discussion) 2011 and 2013. Data were obtained from two prospective and electronic data bases. The number of cases discussed using e-consultation, in-person outpatient clinics evaluation and finally operated on under general anesthesia in each period of time are presented. For efficiency criteria, the index: number of operated on cases/number of first visit outpatient clinic patients is created. Non-parametric Wilcoxon test is used for comparison.
ResultsThe mean number of patients evaluated at the outpatient clinics/year on group A was 563 versus 464 on group B. The median number of cases discussed using videoconferencing/year was 42 for group A versus 136 for group B. The mean number of operated cases/first visit at the outpatient clinics was 0.7 versus 0.87 in group B (P=.04).
ConclusionsThe systematic regular discussion of cases using videoconferencing has a positive impact on the efficacy of the outpatient clinics of a Thoracic Surgery Service measured in terms of operated cases/first outpatient clinics visit.
El objetivo de este estudio es analizar si la discusión sistemática de casos frente a la ocasional de casos dudosos, mediante videoconferencia, se relaciona con una mejora en la eficiencia de la consulta externa presencial de un servicio de cirugía torácica.
MétodoEstudio retrospectivo y comparativo de los pacientes valorados por videoconferencia y consulta externa presencial en 2 periodos de tiempo equivalentes: grupo A (discusión ocasional de casos) entre 2008 y 2010, y grupo B (discusión sistemática semanal) entre 2011 y 2013. Los datos se han extraído de 2 bases de datos prospectivas e informatizadas. Se analizaron el número de pacientes evaluados por videoconferencia y en consulta presencial como primera consulta, y el número de pacientes intervenidos no urgentes bajo anestesia general en cada año y por cada periodo. Se creó el índice casos operados/casos nuevos vistos en consulta externa para cada año y cada periodo. Los datos se compararon usando el test no paramétrico de Wilcoxon.
ResultadosEn el grupo A se vieron una media de 563 pacientes en consulta externa frente a 464 en el segundo periodo. La mediana de casos discutidos por videoconferencia/año fue de 42 en el primer periodo frente a 136 en el segundo. La media del índice de casos operados/casos vistos en consulta externa pasó de 0,7 a 0,87 (p=0,04) del primer al segundo periodo.
ConclusionesLa discusión sistemática de casos mediante videoconferencia sí tiene una repercusión positiva sobre la eficiencia de la consulta externa medida en términos de casos operados/casos nuevos valorados al mejorar dicho índice.
The use of e-consultation as an alternative to in-person medical consultations, or as a means of assessing the referral of patients from primary care to specialized care has been studied from various points of view. At first glance, e-consultation, which is more economical than in-person interviews, appears to reduce outpatient clinic costs,1 although not all authors have found this to be true2; moreover, e-consultations may facilitate and simplify faster access to a specialist,3 and allow medical care to be provided in areas where the population is widely dispersed,4 without compromising quality of care.5 However, the impact of e-consultation on efficacy in specialist outpatient clinics has not been studied to date.
In May 2006, we began to occasionally use clinician–clinician e-consultation to discuss NSCLC cases with different hospitals within our referral area. Our sporadic experience over a 5-year period was positive, so in 2011 we initiated a program of weekly clinician–clinician e-consultations with 2 hospitals within the referral area. In these multidisciplinary e-consultations,6 members of the departments of respiratory medicine, medical oncology and radiotherapy, radiology, and pathology presented the clinical features and radiological images of certain patients to the group and discussed the most suitable treatment.
The aim of this study was to evaluate if systematic clinician–clinician e-consultation versus occasional e-consultation for complicated cases improved efficiency (see definition below in the methods section) in the outpatient clinics of the thoracic surgery department.
Materials and methodsThe study was designed as a retrospective, comparative analysis of newly-evaluated NSCLC patients in the outpatient clinics of the department of thoracic surgery over the 6-year study period. Between 2008 and 2010, the department held e-consultations with any departments that requested our opinion on complicated cases. In 2011, we systematized procedures by setting up weekly e-consultations with the respiratory medicine departments of the Hospital Nuestra Señora de Sonsoles de Ávila and the Healthcare Complex of the University of León. These units were selected because they had reliable access to the necessary technical equipment.
Two study groups were established, according to the frequency of the discussions, each comprising a 3-year period: Group A, 2008–2010, years during which occasional discussions were held, and Group B, 2011–2013, years during which regular weekly discussions were held.
Study populationAll patients evaluated by e-consultation and first-time in-person interviews in the outpatient clinic during the study period were included. The number of patients operated per year and per study period were also computed; operated cases were defined as all those who underwent scheduled surgery with general anesthesia.
Data were obtained from 2 prospective databases maintained in the department computer system. The first of these lists and classifies all healthcare activity in the unit from the first visit to all subsequent procedures performed in the patient. The second database was created specifically to monitor clinician–clinician e-consultations. This database recorded all cases evaluated by e-consultation, including the date of the discussion, the referring hospital, the number of cases evaluated, the reasons why the decision for the patient was pending, and any reasons for ruling out surgery.
E-consultation equipmentThe equipment required for e-consultations included a computer with microphone and webcam together with a corporate application provided by the regional healthcare system (Sacyl) that gave all clinicians participating in the e-consultations access to each others’ computer desktop.
Outpatient consultation efficiency parameters. Statistical analysisThe number of patients evaluated by e-consultation and in person, and the number of patients operated by year and by period was calculated.
The ratio of operated cases to new cases seen in the outpatient clinic per year over each time period (2008–2010 and 2011–2013) was calculated. The mean for each 3-year period was compared using Wilcoxon non-parametric statistics. Data analysis was performed using the Stata SE 12.1 statistical package (StataCorp, Texas, USA).
ResultsBetween 2008 and 2013, a total of 3027 patients were evaluated in a preliminary in-person visit to the outpatient clinic of our department. During this same period, 553 cases were discussed using the clinician–clinician e-consultation system.
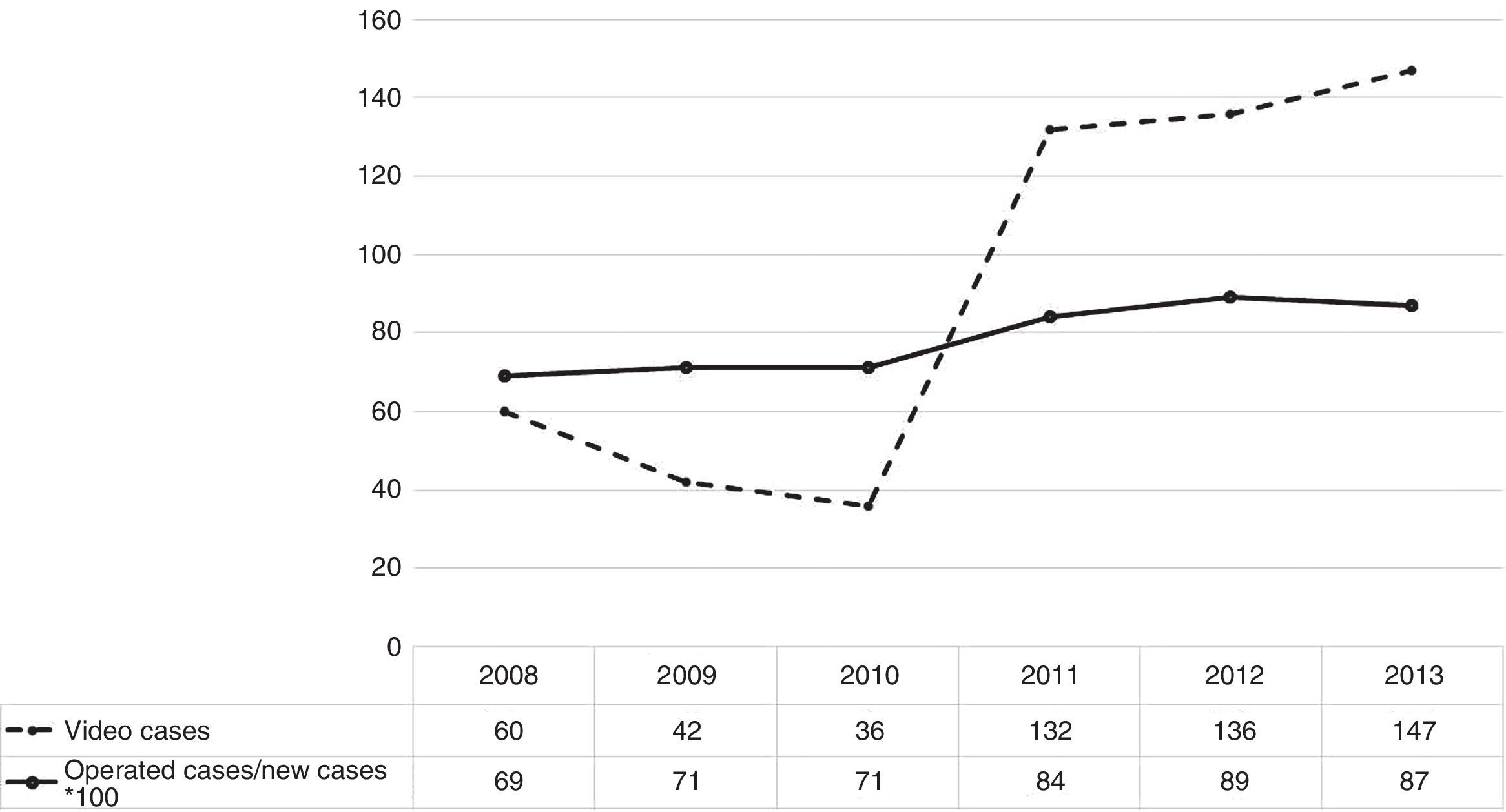
The mean number of cases seen in a first visit between 2008 and 2010 was 563/year (range: 518–565). During this period, the ratio of operated cases to new cases/year seen in the outpatient clinic was 0.69, 0.71, and 0.71, respectively (mean: 0.70). The mean number of cases discussed by e-consultation was 42/year (range: 36–60) during these 3 years.
In the period 2011–2013, the mean number of new cases seen in the outpatient clinic was 464/year (range: 442–475). The ratio of operated cases to new cases/year seen in the outpatient clinic during this period was 0.84, 0.89, and 0.87 respectively (mean: 0.87). The mean number of cases evaluated by e-consultation was 136/year (range: 132–147) during these 3 years.
Differences in the mean ratio of operated cases to new cases seen in the outpatient clinic in each period were statistically significant (Wilcoxon P=0.04). Fig. 1 shows the number of cases evaluated by e-consultation and the ratio of operated cases to new cases/year seen in the outpatient clinic multiplied by 100 for the purposes of obtaining data that can be reproduced on the same graph.
DiscussionOur results indicate that regular clinician–clinician e-consultation had a significant impact on the management of the in-person outpatient clinic. Our results show that e-consultation improves the yield of thoracic surgery outpatient clinics, increasing the ratio of operated cases to new cases seen in this setting from 0.70 to 0.87. As the overall number of patients evaluated in first visits fell, the yield increased: 87% of patients seen in first visits during the second study period (2011–2013) underwent scheduled surgery, and possibly of more interest, the percentage of patients in whom surgery was not advised after the first visit fell from 30% to 13%.
A novel aspect of this study was the creation of a ratio to measure efficiency in the management of a specialized surgical clinic. In our opinion, a surgery department should dedicate all or most of its time to managing patients who require a surgical procedure. Time in the outpatient clinic should be spent preparing patients for surgery and taking definitive decisions on difficult cases, for example, patients with borderline lung function in previous evaluations, such as those discussed in the multidisciplinary e-consultation setting. The novelty of this ratio is that it provides a calculable, objective quality criterion to evaluate the work carried out in the outpatient clinic of a surgery department. Outpatient clinics are mainly managed in terms of numbers: the number of patients seen in first or subsequent visits, waiting times to receive an appointment, etc. Other quality parameters can also be obtained, for example the extent to which the portfolio of specialty services offered meets demand, or the extent to which cases are resolved in the outpatient clinics of each department, but none of these parameters measure the efficiency of experts in the specialized outpatient clinic in terms of time management. The ratio of operated cases to new cases seen in the outpatient clinic clearly reflects this aspect of outpatient clinic activity.
A comprehensive search of the literature leads us to conclude that this is the first time such a ratio has been presented and discussed. Other studies have shown how the use of e-consultation changes and improves the selection of patients seen in nursing outpatient clinics.7 The impact of prospective patient–clinician e-consultation on the time spent on each in-person visit has also been analyzed, showing that this can be significantly reduced8 without compromising quality of care. In this respect, in our department, prospective e-consultations reduced the number of overall clinic visits (from 563 to 464 cases/year), leaving more time available for each patient eventually seen, although this parameter was not measured. The time thus gained was used to gather more detailed, better quality information, prepare surgical cases, and improve the evaluation of the cases that had previously been classified as difficult.
Since it was introduced in the 1970s,9 the utility of e-consultation has been widely demonstrated. The use of technological resources has optimized healthcare by saving both time and money and has also overcome geographical barriers to healthcare,10 an aspect of great importance in our autonomous community. Clinician–clinician e-consultation has been shown to maximize the use of healthcare resources, improve inter-departmental and inter-hospital communications, and reduce patients’ transport costs.11 Moreover, most e-consultation applications have been shown to provide clinicians with the same clinical data as that obtained during an in-person consultation, enabling them to reach accurate diagnoses that can be used to design effective treatment plans.12 We believe, then, that this project has significant socioeconomic advantages for patients, families, healthcare professionals, and the healthcare system.
Very little investment is needed to set up an e-consultation system, since the communication tools are already included in the applications created by the health agencies of the different autonomous communities (e.g., eSalud in Catalonia, cges in the Andalusian Health Service, etc.). The advantages, moreover, far outweigh the cost, since these multidisciplinary meetings give patients faster and more accurate diagnoses and treatments, and reduce the number of duplicate tests and the expense of traveling to see the specialist.3,11 According to a study conducted by Freeman et al.,13 prospective multidisciplinary meetings benefit non-small cell lung cancer patients by promoting adherence to clinical practice guidelines, increasing the percentage of patients who receive full staging and a multidisciplinary evaluation, and significantly reducing the period of time between diagnosis and starting treatment. Stevenson et al.14 analyzed the use of this tool in the evaluation of complex lung cancer patients and suggested that these meetings are easily incorporated into routine practice and do not require any substantial timetable modification. In our case, we opted for a real-time system with both sound and image in which the same group of specialists met to discuss cases.6 Dedicating 1–2h a week to these regular e-consultations did not affect our surgery timetable.
This study has the limitations of retrospective studies, although our data were extracted from prospective databases with 2 consecutive quality control procedures. The main limitation, however, is the absence of evidence to show that all candidates for thoracic interventions seen in outpatient clinic were discussed by e-consultation methods.
In conclusion, in our experience, the implementation of a systematic clinician–clinician e-consultation program improved the overall efficiency of the chest surgery outpatient clinic in our hospital.
FundingThis project was funded in part by a SOCALPAR grant.
Conflict of interestsNone of the authors has any conflict of interests to disclose associated with this study.
The thoracic surgery department thanks Drs. F. Masa and C. Disdier for their collaboration in the initial e-consultations performed before those included in this series.
Please cite this article as: Novoa NM, Gómez MT, Rodríguez M, Jiménez López MF, Aranda JL, Bollo de Miguel E, et al. La discusión de casos por videoconferencia mejora la eficiencia de la consulta externa de cirugía torácica. Arch Bronconeumol. 2016;52:549–552.