The objective of this study was to assess the impact of weather phenomena on the occurrence of spontaneous pneumothorax (SP) in the Plzeň region (Czech Republic).
MethodsA retrospective analysis of 450 cases of SP in 394 patients between 1991 and 2013. We observed changes in average daily values of atmospheric pressure, air temperature and daily maximum wind gust for each day of that period and their effect on the development of SP.
ResultsThe risk of developing SP is 1.41 times higher (P=.0017) with air pressure changes of more than ±6.1hPa. When the absolute value of the air temperature changes by more than ±0.9°C, the risk of developing SP is 1.55 times higher (P=.0002). When the wind speed difference over the 5 days prior to onset of SP is less than 13m/s, then the risk of SP is 2.16 times higher (P=.0004). If the pressure difference is greater than ±6.1hPa and the temperature difference is greater than ±0.9°C or the wind speed difference during the 5 days prior to onset of SP is less than 10.7m/s, the risk of SP is 2.04 times higher (P≤.0001).
ConclusionChanges in atmospheric pressure, air temperature and wind speed are undoubtedly involved in the development of SP, but do not seem to be the only factors causing rupture of blebs or emphysematous bullae.
El objetivo de este estudio fue evaluar la influencia de los fenómenos meteorológicos en la aparición de neumotórax espontáneo (NE) en la región de Pilsen (República Checa).
MétodosAnálisis retrospectivo de 450 casos de NE en 394 pacientes durante los años 1991–2013. Se analizaron los valores diarios medios de presión atmosférica, temperatura ambiental y la velocidad máxima diaria del viento y sus cambios cada día en ese período, en relación con la aparición de NE.
ResultadosEl riesgo de desarrollar NE aumentó 1,41 veces (P=0,0017) en el caso de cambios mayores de ±6,1hPa en la presión atmosférica. Cuando el valor absoluto de los cambios de temperatura ambiental era mayor de ±0,9°C, el riesgo de aparición de NE aumentó 1,55 veces (P=0,0002). Cuando la diferencia en los cambios en la velocidad del viento en los 5 días previos al inicio de NE era menor de 13m/s, el riesgo de NE aumentaba 2,16 veces (P=0,0004). Si la diferencia de presión era mayor de ±6,1hPa y la diferencia de temperatura mayor de ±0,9°C o la diferencia en la velocidad del viento en los 5 días previos al inicio de NE era inferior a 10,7m/s, el riesgo de NE aumentaba 2,04 veces (P≤0,0001).
ConclusiónLos cambios en la presión atmosférica, la temperatura ambiental y la velocidad del viento están indudablemente involucrados en la aparición de NE. Sin embargo, no parecen ser los únicos factores causantes de la rotura de las vesículas o las ampollas enfisematosas.
Spontaneous pneumothorax (SP) develops as a result of the rupture of subpleural blebs, emphysematous bullae or other damage to the pleura or alveolar walls. The rupture may be caused, among other things, by an increase in transpulmonary pressure.1–5 Since cases of SP often occur in groups within a short timescale, some authors suggest that they can develop as a result of weather phenomena that cause changes in transpulmonary pressure. These theories have been discussed repeatedly in the literature, but the findings are inconsistent.1,2,6–12 The aim of this study was to evaluate the possible influence of certain weather phenomena (changes in air pressure and temperature, wind speed, storms) on the emergence of SP among patients in the Plzeň Region (Czech Republic).
Materials and MethodsThis is a retrospective analysis of 450 cases of spontaneous pneumothorax in 394 patients treated between 1991 and 2013 at the Surgery Department of the University Hospital in Plzeň. The patient population consisted of 318 men and 76 women with the mean age of 42 years; the youngest patient was 13 years old, while the oldest was 90 years old. Two hundred and eight (208) patients had so-called primary pneumothorax (52.8%), and 186 patients had secondary pneumothorax (47.2%). The population of the Plzeň region is over 573.000 inhabitants. Meteorological data for the region were obtained from the Plzeň office of the Czech Hydrometeorological Institute. The average sea-level pressure for the Plzeň area is 1013hPa, and the average daily pressure variation is 4hPa. The long-term average air temperature in this region is 8°C, while the average daily temperature deviation is 1.9°C. We observed changes in average daily values of atmospheric pressure in hPa, the average daily air temperature in degrees Celsius, the maximum daily wind gust in m/s, and occurrence of storms for each day of that period and their potential effect on the development of SP compared to the previous period.
Development of SP was described using clusters, where a cluster was defined as at least 2 cases of SP over 3 days. When such clusters were detected, we analyzed the first day of the cluster or the values of parameters over the previous 5 days. In addition to the defined clusters, we found an isolated SP rarely, where the decisive day was the day of SP development, or values of parameters investigated over the maximum of the previous 5 days. We examined the values of the parameters on the day of SP development compared to the previous day. We also examined the differences and quotients of the parameters between the onset date of SP (cluster) and the previous day, the differences and quotients of the values over the 5 days prior to development of SP, and the absolute value of these differences and quotients. Onset of SP was indicated as the first day of symptoms.
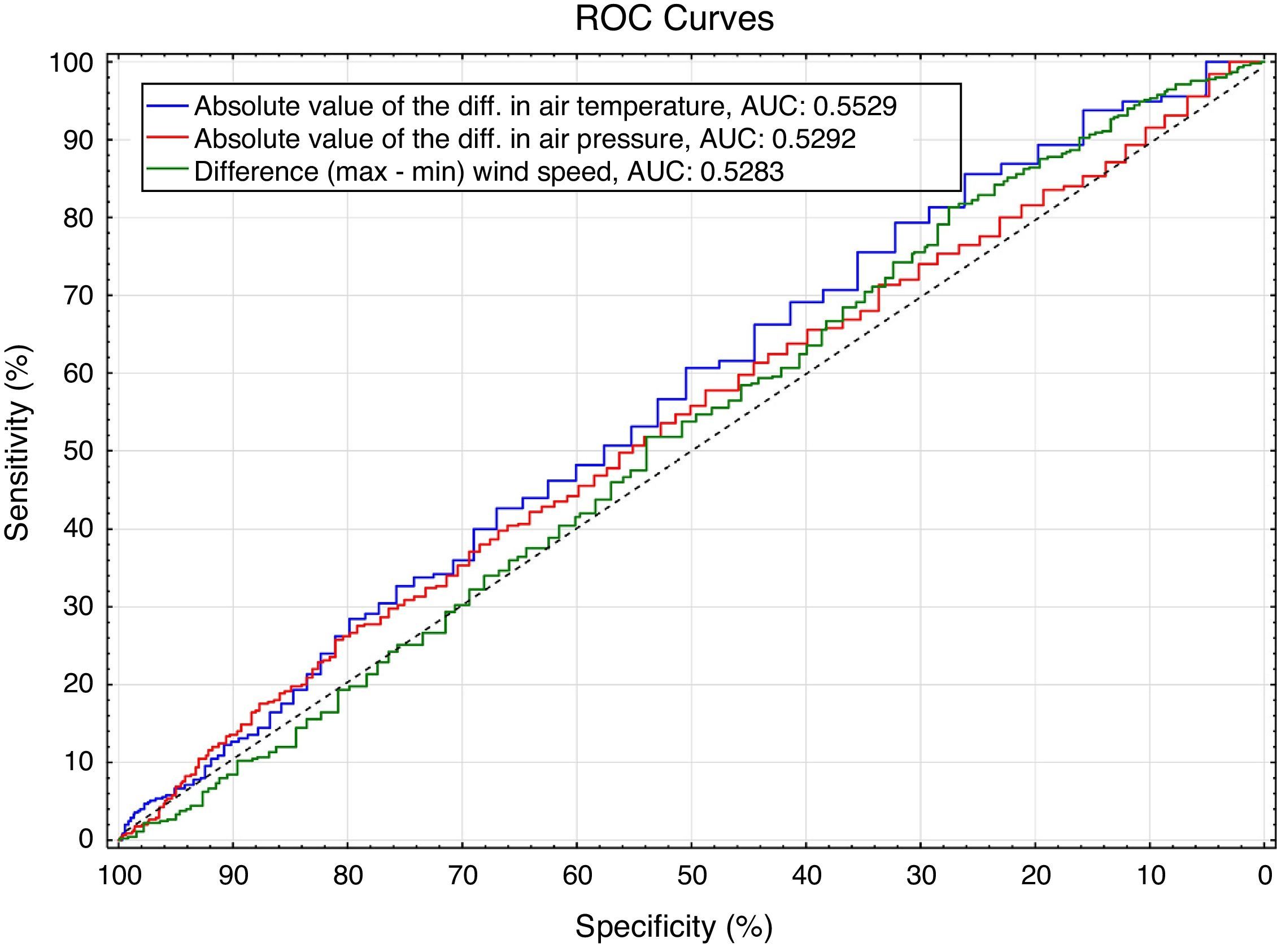
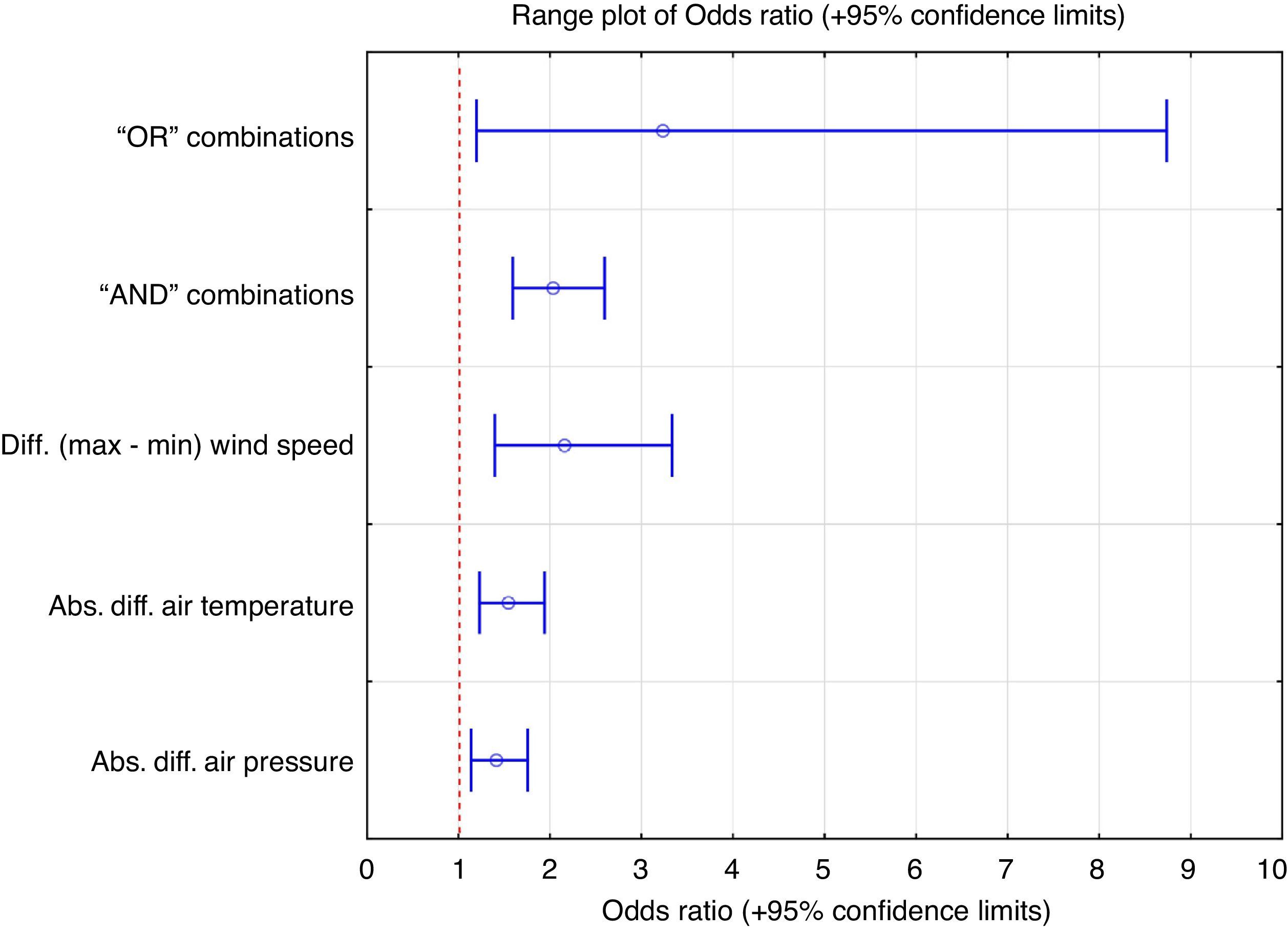
Statistical analysis was performed using SAS (SAS Institute Inc., Cary, NC, USA). Basic statistical data were calculated for the parameters measured in the entire population and in the respective groups. Distribution of the individual parameters in different groups and subgroups was compared using a Wilcoxon two-sample test. Cut-off values of changes in the study parameters were identified using ROC curves and maximizing the Chi-square test criterion. Multivariate analysis of the impact of various factors on the development of SP was performed using logistic regression. The individual factors, and various combinations of cut-off values of the examined factors were combined using “OR” and “AND” statistics (criteria for presumed development of SP). The risk of SP development at different values of the examined variables, and “OR” and “AND” combinations, were expressed using the Odds Ratio (plus 95% confidence interval). Statistical significance was set at alpha=5%.
ResultsMen were significantly more affected than women in the study population, while the elderly were more affected in the female cohort. Development of SP occurred in 450 (5.35%) of the total of 8401 monitored days. A total of 54 clusters were identified, which resulted in 105 cases of SP (23.3%). Outside the clusters, we recorded 345 cases of SP (76.7%).
In cases of SP, statistically significantly increases in the absolute values of changes in air pressure were recorded between the date of onset of SP and the day preceding the day of SP occurrence (Wilcoxon test: P-value=.0360). Using multivariate analysis (logistic regression), this factor was designated as the only statistically significant air pressure factor influencing development of SP. Air pressure changes of more than ±6.1hPa increased risk for SP by 1.41 times (Chi-square test: P-value=.0017; 95% confidence interval of the risk: 1.14–1.76) (statistically the strongest cut-off).
Similar statistically significant differences were found in air temperature on the day of occurrence of SP compared to the days without SP (Wilcoxon test: P-value=.0002). When the absolute value of the air temperature changed by more than ±0.9°C, the risk of SP was 1.55 times higher (Chi-square test: P-value=.0002; 95% confidence interval of risk: 1.23–1.94) (statistically the strongest cut-off).
We found statistically significant differences in wind speed on the day of development of SP, where the wind speed was higher in the SP group (Wilcoxon test: P-value=.0163). However, some of the wind speed changes were less clear. After further statistical analysis, we concluded that the difference between the minimum and maximum value of the wind speed over the 5 days prior to development of SP was significantly lower in the SP group (Wilcoxon test: P-value=.0438). Multivariate analysis (logistic regression) identified the difference between the minimum and maximum wind speed as the most statistically significant factor. When the wind speed differed by less than 13m/s over the 5 days prior to onset of SP, the risk of SP was 2.16 times higher (Chi-square test: P-value=.0004; 95% confidence interval of the risk: 1.40–3.34) (statistically the strongest cut-off). (Fig. 1).
We also examined different combinations of the factors studied (wind temperature, pressure, speed) and their possible cut-offs at the development of SP. If the difference between temperatures was greater than ±0.9°C or that of wind speed over the 5 days prior to onset of SP less than 13m/s (the “OR” combination), the risk of SP was 3.24 times higher (Chi-square test: P-value=.0143; 95% confidence interval of the risk: 1.20–8.74). This condition was met in 99.11% of all SP studied. Other variants of the “OR” combinations have not yielded similarly good results. When the pressure difference was greater than ±6.1hPa and the temperature difference greater than ±0.9°C or the difference in wind speed over the 5 days prior to onset of SP was less than 10.7m/s (“AND” combination), the risk of SP was 2.04 times higher (Chi-square test: P value=<.0001; 95% confidence interval of the risk: 1.59–2.60). Other variants of the “AND” combinations have not yielded such good results. (Fig. 2)
Storms had no effect on the development of SP. Similarly, there was no significant difference in the occurrence of SP between the individual months of the year or seasons.
DiscussionSpontaneous pneumothorax develops from rupture of emphysematous bullae, subpleural blebs, or from other pleural anomalies. These ruptures may be caused, among other reasons, by an increase in the transpulmonary pressure under the influence of certain weather changes.1–5 In the last 2 decades, several studies addressing this phenomenon have been published, but their findings are inconclusive.1,2,6–12 These studies most often monitored the effects of changes in atmospheric pressure and air temperature, but also studied the effects of phenomena such as air humidity, sunshine duration, amount of precipitation, and storms among others.7,9–13 The values of these parameters are usually examined on the day of onset of SP and compared to the days preceding the onset of SP, or to the period between the days, or to days without SP.4,7,9,11,12
A significant number of SP cases, according to the experience of some authors, are found in clusters, i.e. multiple cases of SP may develop in a short time. Therefore, they defined clusters of occurrence involving at least 2 cases of SP in an interval of 3 days. In their respective patient populations, Alifano reported 84% of SP in 76 clusters; Smit 73%, Bertolaccini 81%, and Özpolat 70.5% occurrence of SP cases in 188 clusters.1,3,14,15 Our occurrence of 23.3% of cases in 54 clusters is lower, but in our opinion, this was caused by a relatively small number of SP cases examined over a relatively long period of time (22 years).
Zhang found significant differences in the average daily values of air pressure between days with and without SP, but not between the onset date of SP and the preceding day.12 In contrast, Alifano found a difference in the atmospheric pressure between the day before the onset and the day of onset of SP; the occurrence date in this case was also designated as the first cluster day.1 This is consistent with our results; we found significantly higher differences in the absolute values of changes in air pressure between the onset date of SP and the day prior to the day of onset of SP. Bense concluded that a decrease in atmospheric pressure by at least 10hPa in 24h is associated with a statistically significant increase in the number of cases of SP in the following 2 days.6 The influence of a drop in air pressure on the development of SP was also reported by Haga, Özpolat and Schieman.2,3,5 In contrast, Diaz considers an increase in atmospheric pressure to be a risk factor for SP, finding that it increases the likelihood of SP 1.15-fold with each 1hPa increase in atmospheric pressure.9 In our patient group, changes in air pressure of more than ±6.1hPa increased the risk of SP by 1.41-fold, i.e. both a marked increase and decrease in air pressure are associated with risk for development of SP. Morales, Bertolaccini and Scott accepted the effects of changes in air pressure on the development of SP.4,14,16 In contrast, Obuchi, Sakai, Chen and others found that changes in atmospheric pressure have no influence on the occurrence of SP.7,8,10,11,13,15,17
Our results are in line with Zhang and Sakai, insofar as we found statistically significant differences in air temperature (both increase and decrease) on days of SP occurrence versus days without SP.11,12 However, we cannot confirm the conclusions of Obuchi and Smit, who both found an increase in air temperature to have a significant effect on SP 1 or 2 days before occurrence.13,15 Other authors, such as Celik, Alifano and others found no effect of changes in air temperature on development of SP.1,2,7,8
Our results regarding the effects of wind speed on the development of SP are somewhat contradictory. On the one hand, we found significant differences in wind speed on the onset date of SP, where the wind speed was higher in the SP group, but on the other hand, the same SP group showed significantly lower minimum and maximum values of wind speed over the 5 days prior to onset of SP. This relationship was paradoxically identified by multivariate analysis as the most statistically significant factor of SP development. Of the foregoing authors, only Schieman reported significant conclusions regarding wind speed in his study: like us, he recorded significantly stronger wind speed on the days of SP compared to those without SP.5 We cannot explain why temperature and wind speed changes influence development of SP; we merely present statistically significant results. We can only assume that it can be associated with pressure changes related to wind speed or temperature changes.
Probably the most interesting results of our study, in view of the existing literature, were obtained by examination of the impact of the combination of parameters. Air temperature seems to be a decisive factor both in the “OR” and in the “AND” combinations. By combining “OR” changes in air temperature and wind speed, we managed to explain the occurrence of more than 99% of SPs studied (3.24-fold higher risk of SP). We believe that this is probably the most important finding of our study. However, even the results of our “AND” combination (2.04-fold higher risk of developing SP) analyses indicate that changes in the weather phenomena studied have a significant effect, and that this effect is magnified when the phenomena occur simultaneously. Of the foregoing authors, both Özpolat and Schieman conducted a similar analysis, and reached the same conclusion regarding the effects of pressure or air temperature; Schieman, however, found a greater difference in wind speed than that found in our study.3,5
Unlike Alifano or Smit, for example, we found no correlation between the occurrence of storms or lightning and onset of SP.1,15 Similarly, we found no monthly or seasonal differences in onset of SP, a finding echoed by most authors.5,7,10,18
ConclusionOur findings show that certain weather phenomena, such as changes in atmospheric pressure, air temperature and wind speed, are undoubtedly involved in the development of SP. However, they would not seem to be the only factors causing rupture of blebs or emphysematous bullae. Other risk factors, such as sport activity, definitely play an important role. Our findings are unclear insofar as we could not find any factor, or combination of factors, that would show a clear separation of risk and non-risk days in relation to the development of SP. More detailed information in this area could be obtained from further studies with more SP cases over a shorter period of time.
FundingSupported by the MZ IGANT14227, NS9644 and NT14332-3 grants.
Authors’ ContributionJosef Vodička – study design, collection of data, data analysis/interpretation, writing of the manuscript. Šárka Vejvodová – study design, collection of data. David Šmíd – collection of data, data analysis/interpretation. Jakub Fichtl - collection of data, data analysis/interpretation. Vladimír Špidlen – collection of data. Stanislav Kormunda – data analysis/interpretation, writing of the manuscript. Jiří Hostýnek – study design, collection of data. Jiří Moláček – revision of the manuscript.
Conflict of InterestsThe authors declare they have no conflict of interest directly or indirectly related to the manuscript contents.
Please cite this article as: Vodička J, Vejvodová Š, Šmíd D, Fichtl J, Špidlen V, Kormunda S, et al. ¿Tienen los fenómenos meteorológicos alguna influencia en la aparición de neumotórax espontáneo? Arch Bronconeumol. 2016;52:239–243.