Diffuse alveolar hemorrhage (DAH) is a clinical condition characterized by hemoptysis, anemia and dyspnea. The radiological pattern of this disease is defined by ground-glass consolidations and interlobular septal thickening (crazy-paving pattern). Causes are multiple and include malignancy, infections, autoimmune diseases, coagulopathies and pulmonary hypertension. Pheochromocytoma is a tumor derived from chromaffin cells that typically presents as arterial hypertension (HT) associated with diaphoresis, tachycardia and headache. We describe below the case of a patient whose initial clinical manifestation of pheochromocytoma was massive hemoptysis and acute coronary syndrome. This case demonstrates the importance of considering pheochromocytoma as a possible diagnosis in cases of DAH with no apparent cause.
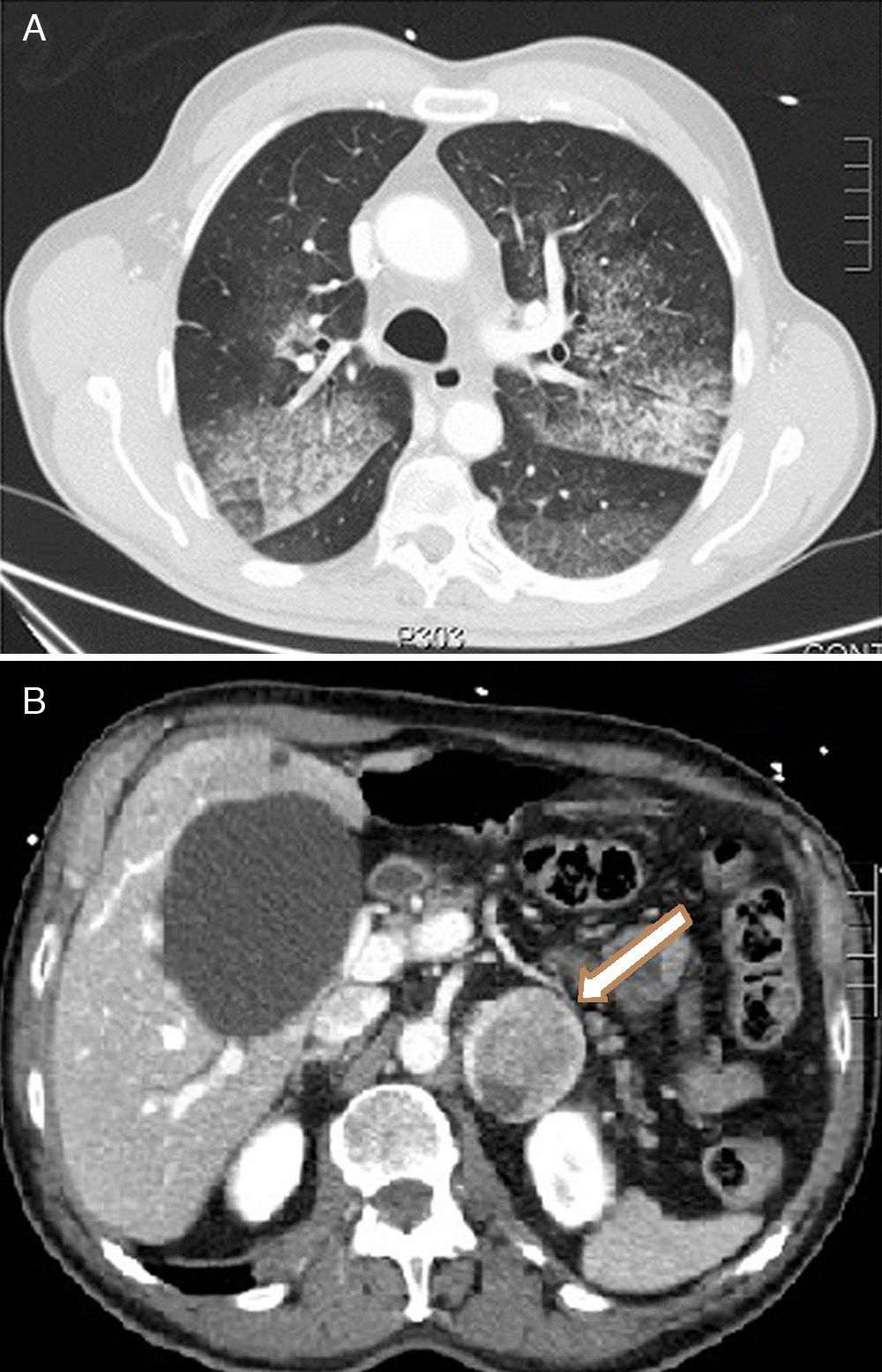
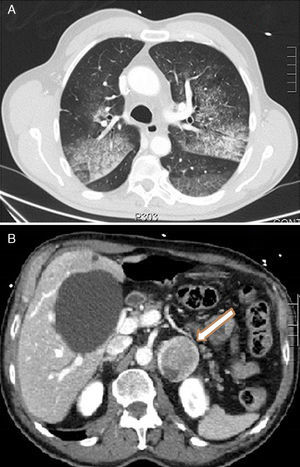
A 68-year-old male was seen in the emergency room after an episode of frank hemoptysis associated with oppressive chest pain, nausea, sweating and pallor. Dyspnea, cold sweats and pallor were confirmed on physical examination. BP>180/100mmHg, HR 120bpm. There were no significant changes on ECG and bilateral diffuse alveolar pattern was observed on chest X-ray. Laboratory test parameters of note included blood glucose 257mg/dl, leukocytosis with neutrophilia, hemoglobin 14g/dl (MCV normal), creatinine 1.19mg/dl, urea 62mg/dl, troponin T 596.6ng/l and CK 186U/l. Arterial blood gases were compatible with hypoxemic respiratory failure (PaO2 51.4mmHg). Non-ST segment elevation acute coronary syndrome with hemoptysis was suspected, so the patient was admitted to the ICU where double antiplatelet therapy was initiated but not anticoagulation, due to hemoptysis. The patient had another episode of frank hemoptysis associated with a hypertensive crisis requiring oxygen therapy and intravenous bolus administration of methylprednisolone. The clinical picture improved within hours with normalization of renal function and anemia (Hb 10.9g/dl). When the patient was interviewed again, he reported episodes of headache, sweating and palpitations on performing Valsalva manoeuvers. CT showed a crazy-paving lung pattern, ground-glass consolidations and interlobular septal thickening, compatible with alveolar hemorrhage (Fig. 1A) and heterogeneous left adrenal lesion 46mm×40mm (Fig. 1B). Raised catecholamine and metanephrine levels in urine (noradrenaline 1208.4μg/24h, adrenaline 532μg/24h, normetanephrine 5748.6μg/24h, metanephrine 12,281.6μg/24h) confirmed the diagnosis of pheochromocytoma. The patient was treated with alpha blockers (phenoxybenzamine 10mg/8h), later combined with a beta blocker (propranolol 10mg/8h). After 7 days of progressive improvement, fiberoptic laryngoscopy revealed pharynx and larynx free of bleeding and bronchoscopy was normal. Bronchoalveolar lavage contained no malignant cells and abundant hemosiderophages (>20%). Anti-DNA, c-ANCA, anti-MPO and anti-GBM antibodies and cultures were negative. After the patient stabilized, left adrenalectomy was performed by laparoscopy; the pathology examination revealed pheochromocytoma with malignant histological features. During follow-up the patient remained asymptomatic and all tests requested were normal (2 months after the episode, the patient had a PaO2 of 85mmHg).
On rare occasions pheochromocytoma can present with atypical manifestations such as hemoptysis, acute coronary syndrome with normal coronary catheterization or dilated cardiomyopathy.1 Pathophysiological mechanisms most often involved in hemoptysis are lung metastases and coagulation disorders.2,3 When all of these have been ruled out, hemoptysis may be related to the hypertensive crisis triggered by cromaffin tumor secretion.4,5 In these cases, the paroxystic HT crises will produce pulmonary vein hypertension causing capillary rupture and the passage of erythrocytes to the alveolar space, resulting in hemoptysis. The interest in this case is that the presence of pheochromocytoma should be considered in the differential diagnosis of DAH of unknown origin, and that failure to diagnose may be potentially fatal.
Please cite this article as: Querol Ripoll R, del Olmo García MI, Cámara Gómez R, Merino-Torres JF. Hemorragia alveolar difusa como primera manifestación clínica de un feocromocitoma. Arch Bronconeumol. 2014;50:412–413.