A study was performed to assess differences in the clinical presentation of tuberculosis between two groups of immigrants. Ninety-four patients seen in the emergency room for newly diagnosed tuberculosis between 2006 and 2012 were included. Forty-nine patients were from Asian countries and 45 from Latin America. Mean age [years (SD)] was 35.3 (13) in Asian patients and 33.9 (10) in Latin American patients. Asian subjects were predominantly male (40/49 vs 25/45; P=0.006). Patients from Latin American countries had a higher rate of pulmonary tuberculosis. A higher percentage of Asian patients lived in overcrowded conditions, whereas HIV infection was more frequent among Latin Americans. Most patients were treated with a quadruple regimen. Resistance to isoniazid was documented in two patients from Latin America.
Se realizó un estudio descriptivo para identificar posibles diferencias en la presentación clínica de la tuberculosis entre 2 grupos de población inmigrante. Se incluyeron 94 pacientes visitados en urgencias y que fueron diagnosticados de tuberculosis activa en el periodo 2006-12. Cuarenta y nueve pacientes era originarios de Asia Central (A) y 45 de Latinoamérica (LA). La edad media (años [DE]) fue de 35,3 (13) años en los procedentes de A por 33,9 (10) en los de LA. Existía un predominio de varones en asiáticos (40/49 vs. 25/45; p=0,006). Los pacientes procedentes de LA tenían mayor porcentaje de tuberculosis pulmonar. Los pacientes de A vivían en condiciones de hacinamiento con mayor frecuencia. Los pacientes de LA tenían más antecedentes de seropositividad para el VIH. La mayoría recibió tratamiento cuádruple. Dos pacientes latinoamericanos eran resistentes a isoniazida.
In recent decades, improvements in social conditions and hygiene and the availability of more effective treatments have contributed to a fall in the incidence of tuberculosis (TB). In Spain, however, this trend is slowing down, partly due to high numbers of immigrants from countries where this disease is highly prevalent.1 The most important factors to consider with regard to immigration are younger age,2 human immunodeficiency virus (HIV) coinfection,2 crowded living conditions, and poor treatment compliance. In 2013 in Barcelona, one of the Spanish cities with the highest flow of immigration, 331 new cases of TB were diagnosed, 126 of which were identified in the districts of Cuitat Vella and Sant Martí. Of these, 56% were from Asian countries, most of whom are registered in Ciutat Vella, where overcrowding is at its worst, and 15% were from Latin American countries. To our knowledge, this is the first study to compare the different characteristics of populations from different origins; differences observed were probably due to their different social conditions. The aim of the study is to determine the differences in the clinical presentation of TB between 2 immigrant populations, and to determine the percentage of resistance in both groups.
Clinical ObservationsA retrospective descriptive study was conducted of new TB cases (diagnosed during the index visit or subsequent follow-up) in patients from Latin America or Asia, seen in the emergency department between 2006 and 2012. We reviewed the discharge reports from the corresponding medical department (emergency room or hospital ward), with the exception of pediatrics, recording a diagnosis of TB, tuberculosis infection or mycobacterial infection. Diagnosis of TB was considered in cases with microbiological confirmation by culture in Löwenstein-Jensen medium and/or BACTEC®. Cases with a clinical picture consistent with TB, pleural effusion and elevated adenosine deaminase (ADA) were also included.
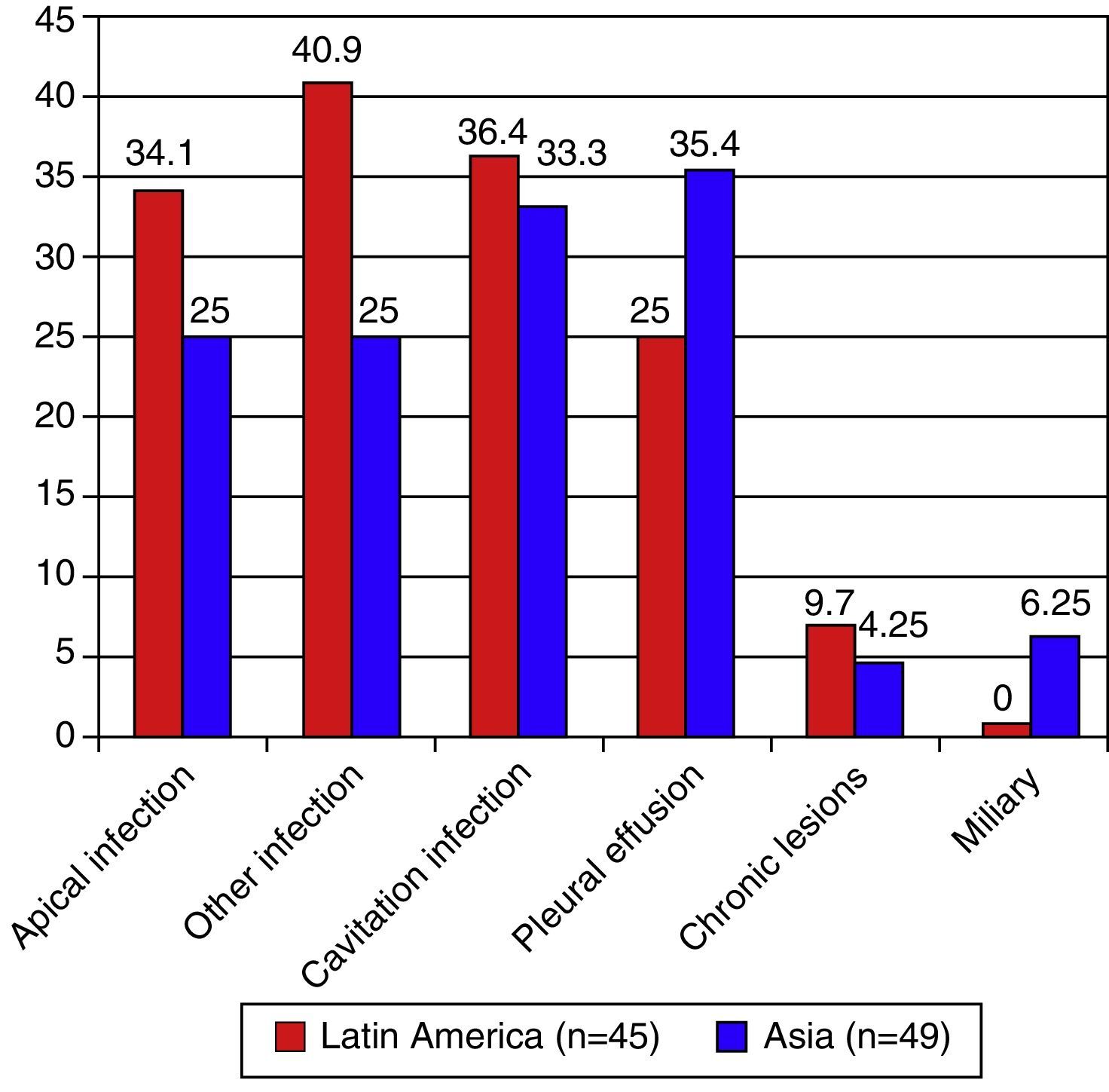
Of the 222 patients with a final diagnosis of TB, 62.6% were immigrants, of whom 49 were from Asia and 45 from Latin America. Countries most represented were Pakistan (37 cases) and Bolivia (11). Table 1 shows the baseline characteristics, most common symptoms and TB site. Radiological findings are shown in Fig. 1. A chest computed tomography (CT) was performed in 9.1% of the Latin American patients and in 28.3% of the Asian patients (P=0.019). Thus, 2 Latin American patients with a negative chest X-ray could be identified as disease carriers. Latin American patients had a greater percentage of pulmonary TB. Extrapulmonary TB, defined as all TB involvement outside the lung parenchyma, was found in 13 Latin American (29.5%) and 24 (29.9%) Asian patients (P=.044). Ten patients had concomitant pulmonary and extrapulmonary TB (6 from Asia and 4 from Latin America). Sputum bacilloscopy was positive in 83.9% of Latin American patients with pulmonary TB and in 88.5% of those from Asia (P=not significant). Most patients received quadruple therapy (100% of Asians and 93.2% of Latin Americans). Isoniazid resistance was documented in 2 Latin American patients.
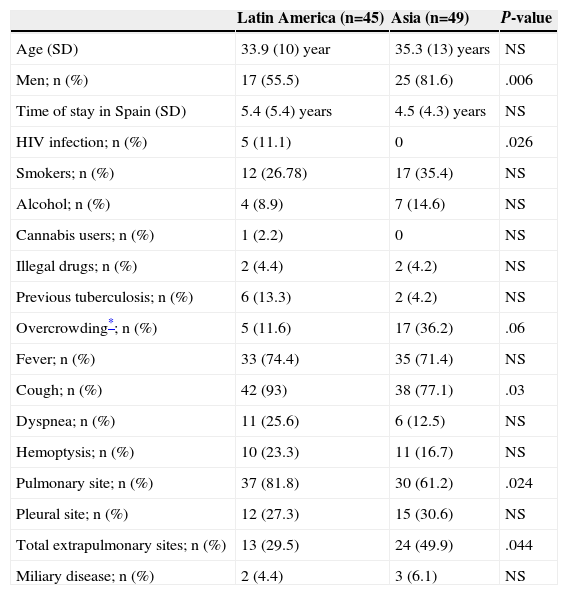
Baseline Characteristics of the Study Groups, Most Common Symptoms and Tuberculosis Site.
| Latin America (n=45) | Asia (n=49) | P-value | |
|---|---|---|---|
| Age (SD) | 33.9 (10) year | 35.3 (13) years | NS |
| Men; n (%) | 17 (55.5) | 25 (81.6) | .006 |
| Time of stay in Spain (SD) | 5.4 (5.4) years | 4.5 (4.3) years | NS |
| HIV infection; n (%) | 5 (11.1) | 0 | .026 |
| Smokers; n (%) | 12 (26.78) | 17 (35.4) | NS |
| Alcohol; n (%) | 4 (8.9) | 7 (14.6) | NS |
| Cannabis users; n (%) | 1 (2.2) | 0 | NS |
| Illegal drugs; n (%) | 2 (4.4) | 2 (4.2) | NS |
| Previous tuberculosis; n (%) | 6 (13.3) | 2 (4.2) | NS |
| Overcrowding*; n (%) | 5 (11.6) | 17 (36.2) | .06 |
| Fever; n (%) | 33 (74.4) | 35 (71.4) | NS |
| Cough; n (%) | 42 (93) | 38 (77.1) | .03 |
| Dyspnea; n (%) | 11 (25.6) | 6 (12.5) | NS |
| Hemoptysis; n (%) | 10 (23.3) | 11 (16.7) | NS |
| Pulmonary site; n (%) | 37 (81.8) | 30 (61.2) | .024 |
| Pleural site; n (%) | 12 (27.3) | 15 (30.6) | NS |
| Total extrapulmonary sites; n (%) | 13 (29.5) | 24 (49.9) | .044 |
| Miliary disease; n (%) | 2 (4.4) | 3 (6.1) | NS |
HIV: human immunodeficiency virus; SD: standard deviation.
This study highlights differences in 2 groups of immigrants, depending on their place of origin. It is of interest that all HIV-positive patients (11%) were from Latin America, although the rate of coinfection is similar to that described by González-Moreno et al.,3 and is slightly higher than the figures reported by the European TB surveillance report.4 The proportion of cases of extrapulmonary disease is high in both groups, and almost half the Asian patients had this form (similar to rates in the HIV population1). Possible causes for these findings may due to the different social conditions of the patients, both in Spain and in their home countries, and to possible differences in infection dynamics (primary infection or recurrence). Unfortunately, although only 4.2% of the Asian patients had previously documented TB, no reliable data are available in this area. It is interesting to note the high percentage of positive bacilloscopies in both patients compared to Spanish registries,3 and the low percentage of resistance (4.5%), similar to that found in other Spanish series.1,5
To our knowledge, this is the first study performed in our geographical region that evaluates the characteristics of 2 different immigrant populations of patients with TB at the time of receiving care in an emergency department. More studies are needed to detect possible differences in the characteristics of TB in other immigrant populations and in other geographical regions.
Please cite this article as: Supervía A, Pallàs O, Piccari L, Herrera Fernández S, Domínguez Álvarez M, Cirera I, et al. Diferencias en los hallazgos clínicos en dos grupos de población inmigrante afecta de tuberculosis. Arch Bronconeumol. 2015;51:e29-e31.