Between 4% and 10% of respiratory problems in pulmonology departments involve pleural effusion (PE), and more than 3000 individuals per million inhabitants are affected.1 In the last decade, there has been a significant advance in diagnostic and therapeutic techniques in this disease that have led to modifications in management algorithms.2–5 However, the management of PE in our setting has not been fully characterized. Surveys or clinical audits are evaluation strategies aimed at improving the quality of the processes and outcomes of a clinical service. In other countries, such as the United Kingdom, some scientific societies have conducted audits focused on collecting data in clinical practice, which has allowed them to define and assess areas for improvement.6–8
An understanding of the organization and specific aspects of care in this disease could help us develop recommendations to try to achieve quality care. For this reason, and with the aim of assessing the current state of affairs, we conducted this study. The main objective was to describe clinical care and to collect data on patient management, safety aspects, ethical and legal considerations, and on teaching and research activity in PE.
Between July and October 2016, we carried out a multicenter cross-sectional study in Spain, with a survey that was sent to pulmonology department heads, managers, and physicians specializing in pleural diseases in public sector hospitals of different levels of complexity. Hospital complexity was classified according to criteria used in other studies performed in Spain.9 Study sites were selected randomly, and 129 hospitals were included. The respondents were contacted by email, and invited to complete the survey on an online platform. This survey included 22 items on different organizational, care, teaching and research aspects.
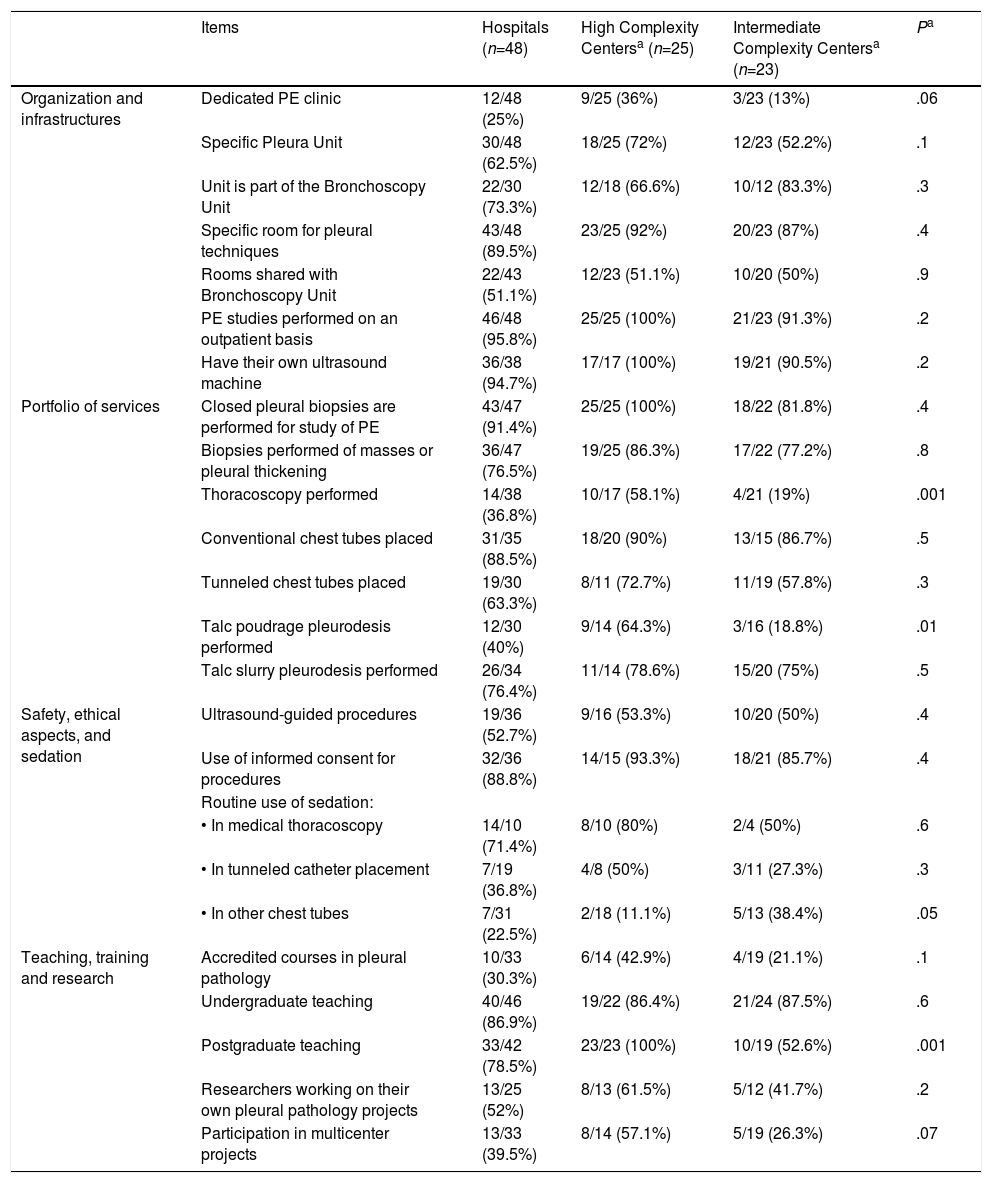
The survey was completed by 48 (37%) professionals, 24 (50%) heads of department, 11 (23%) heads of unit, and 13 specialists in PE; 23 (48%) hospitals were centers of medium complexity (between 200 and 500 beds and more than 50 interns) and 25 (52%) were high complexity (ample technological resources, more than 500 beds and between 160 and 300 interns). The survey was not completed by any low complexity center. Table 1 shows the results of the analysis of the different items by complexity of the center.
Overall Survey Results and Differences in Organizational Aspects, Care, Teaching and Research Depending on the Complexity of the Center.
| Items | Hospitals (n=48) | High Complexity Centersa (n=25) | Intermediate Complexity Centersa (n=23) | Pa | |
|---|---|---|---|---|---|
| Organization and infrastructures | Dedicated PE clinic | 12/48 (25%) | 9/25 (36%) | 3/23 (13%) | .06 |
| Specific Pleura Unit | 30/48 (62.5%) | 18/25 (72%) | 12/23 (52.2%) | .1 | |
| Unit is part of the Bronchoscopy Unit | 22/30 (73.3%) | 12/18 (66.6%) | 10/12 (83.3%) | .3 | |
| Specific room for pleural techniques | 43/48 (89.5%) | 23/25 (92%) | 20/23 (87%) | .4 | |
| Rooms shared with Bronchoscopy Unit | 22/43 (51.1%) | 12/23 (51.1%) | 10/20 (50%) | .9 | |
| PE studies performed on an outpatient basis | 46/48 (95.8%) | 25/25 (100%) | 21/23 (91.3%) | .2 | |
| Have their own ultrasound machine | 36/38 (94.7%) | 17/17 (100%) | 19/21 (90.5%) | .2 | |
| Portfolio of services | Closed pleural biopsies are performed for study of PE | 43/47 (91.4%) | 25/25 (100%) | 18/22 (81.8%) | .4 |
| Biopsies performed of masses or pleural thickening | 36/47 (76.5%) | 19/25 (86.3%) | 17/22 (77.2%) | .8 | |
| Thoracoscopy performed | 14/38 (36.8%) | 10/17 (58.1%) | 4/21 (19%) | .001 | |
| Conventional chest tubes placed | 31/35 (88.5%) | 18/20 (90%) | 13/15 (86.7%) | .5 | |
| Tunneled chest tubes placed | 19/30 (63.3%) | 8/11 (72.7%) | 11/19 (57.8%) | .3 | |
| Talc poudrage pleurodesis performed | 12/30 (40%) | 9/14 (64.3%) | 3/16 (18.8%) | .01 | |
| Talc slurry pleurodesis performed | 26/34 (76.4%) | 11/14 (78.6%) | 15/20 (75%) | .5 | |
| Safety, ethical aspects, and sedation | Ultrasound-guided procedures | 19/36 (52.7%) | 9/16 (53.3%) | 10/20 (50%) | .4 |
| Use of informed consent for procedures | 32/36 (88.8%) | 14/15 (93.3%) | 18/21 (85.7%) | .4 | |
| Routine use of sedation: | |||||
| • In medical thoracoscopy | 14/10 (71.4%) | 8/10 (80%) | 2/4 (50%) | .6 | |
| • In tunneled catheter placement | 7/19 (36.8%) | 4/8 (50%) | 3/11 (27.3%) | .3 | |
| • In other chest tubes | 7/31 (22.5%) | 2/18 (11.1%) | 5/13 (38.4%) | .05 | |
| Teaching, training and research | Accredited courses in pleural pathology | 10/33 (30.3%) | 6/14 (42.9%) | 4/19 (21.1%) | .1 |
| Undergraduate teaching | 40/46 (86.9%) | 19/22 (86.4%) | 21/24 (87.5%) | .6 | |
| Postgraduate teaching | 33/42 (78.5%) | 23/23 (100%) | 10/19 (52.6%) | .001 | |
| Researchers working on their own pleural pathology projects | 13/25 (52%) | 8/13 (61.5%) | 5/12 (41.7%) | .2 | |
| Participation in multicenter projects | 13/33 (39.5%) | 8/14 (57.1%) | 5/19 (26.3%) | .07 |
PE: pleural effusion.
Significant differences can be observed among Spanish hospitals in terms of organization of the care of pleural disease, associated mainly with the complexity of the centers. According to data from the White Paper on Respiratory Medicine,10 which surveyed nearly 500 pneumologists in 2014, there were only specific pleura clinics in 12% of the centers with less than 750 beds and in 20% of those with more than 750 beds. Although in our survey, 52% and 72% of the hospitals of medium and high complexity, respectively, claimed to have a pleura unit, this was integrated into the bronchoscopy unit in 83% and 66% of the sites, respectively. Only 13% of hospitals of medium complexity and 36% of high complexity had dedicated pleura clinics: these results are similar to those published in the White Paper.10 In 96% of the centers, PE is studied on an outpatient basis, with no differences between centers. In a previous study, we found that ambulatory care can be delivered with a high level of efficiency and equal level of safety.11
The number of centers that perform advanced procedures such as thoracoscopy or tunneled drainage is limited, especially in hospitals of medium complexity. However, the percentage of hospitals that include conventional chest tubes or talc slurry pleurodesis in their portfolio of services is higher, and both procedures are therapeutic alternatives in infectious or malignant PE.4,5 The White Paper found that 35% of pulmonologists do not perform ultrasound, tube placement, pleurodesis, or fibrinolysis.10 The results for some of these procedures were different in this survey, but this may be because some were inappropriately recorded. It would appear necessary that all pleural techniques be centralized, thus justifying the creation and development of specific units to which value may be added by incorporating more advanced procedures.
In 2015, the British Thoracic Society published the details of their second audit.8 They found a greater use of informed consent and an increase in the use of ultrasound guidance for chest tube insertion, from 52% to 69%. Ultrasound was available in 82% of the hospitals.8 In our survey, although 94% of the centers had an ultrasound machine, only 52% used it.
A quality criterion in pleural pathology is obtaining informed consent, which was done in nearly 90% of cases. The use of sedation and anesthesia has been shown to decrease the risk of complications and patient anxiety or pain.12 In our study, its indication was limited, especially in pleural drainage.
Specialized pleural disease units are the perfect setting for training specialists and for developing quality translational and clinical research.13,14 The postgraduate training program in pulmonology states that interns must acquire a high level of competence in thoracentesis, although a recent study shows that this group of professionals had certain shortcomings in knowledge and practice, the use of anesthesia, performing the procedure without ultrasound, and processing samples.15 This survey underlines the need to improve training in the diagnostic and therapeutic management of PE, particularly in the performance of thoracentesis.15 Another of the areas studied was training and teaching. Only 30% of the respondent hospitals ran accredited courses, with slightly higher rates in high complexity centers. Teaching activities correlated with the complexity of the hospital, especially postgraduate teaching. Research leads to improved quality of care and, in addition to care, teaching and management, is a corporate objective. The number of research projects, whether conducted exclusively in the center or in a multicenter setting, was low.
Although pleural units have been shown to deliver effective management of the patient with pleural disease, standardization in clinical practice between the centers is difficult. We must offer better training programs and the management of patients with PE must be protocolized and adapted to the standards recommended by the scientific societies and clinical practice guidelines.4,5,12 Quality plans and improvement strategies supported by scientific societies must be encouraged.
A limitation of this study was the low percentage of professionals who completed the survey, as in other similar studies. Although a larger study might allow us to make a better comparison between the care of these patients in centers of the same complexity and establish recommendations for better management of these processes, we believe that this paper provides valuable information for all professionals interested in pleural pathology.
Conflict of InterestsThe authors declare that they have no conflict of interests directly or indirectly related with the contents of this manuscript.
Dr. Victor del Campo Pérez, Preventive Medicine, Hospital Álvaro Cunqueiro, SEPAR Integrated Research Program in Interventional Pulmonology
Please cite this article as: Botana-Rial M, Núñez-Delgado M, Leiro-Fernández V, Fernández-Villar A. Resultados de una encuesta nacional sobre la situación actual del manejo del derrame pleural. Arch Bronconeumol. 2019;55:274–276.