Lung transplantation (LT) is the definitive therapy for patients with end-stage lung disease.1,2 However, long-term survival after LT is not as promising as it is after kidney or liver transplantation,1,3,4 and the first year after LT remains a high-risk period for complications requiring hospitalisation and ICU readmission.5 Most recent studies have focused on complications occurring during the early postoperative period (≤30 days post-transplantation).6–8 This report describes the clinical characteristics and comorbidities associated with 1-year mortality in LT recipients who required ICU readmission beyond the 30-day post-transplantation period.
We performed a single-centre study and retrospective analysis from the data of all LT patients who were readmitted to the ICU beyond 30-day post-ICU discharge after the first ICU stay due to the immediate postoperative admission after lung transplantation over 6-years period (from January 1, 2011 to December 31, 2016).
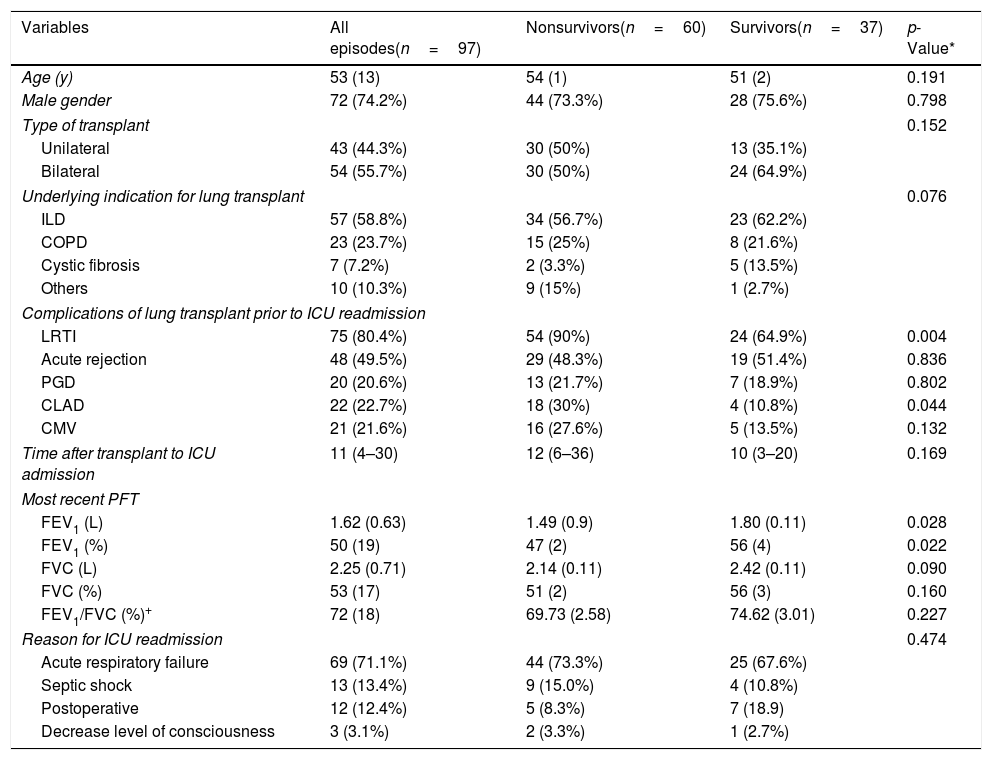
A total of 342 patients underwent LT, and 81 LT recipients (24%) required ICU readmission beyond the initial 30-days after ICU-discharge, with a total of 97 episodes assessed. Sixty-five patients were admitted once, 14 patients were admitted twice, and two patients were readmitted three times. The median time from LT to ICU readmission was 11 (4–30) months. The most common indication for ICU readmission was acute respiratory failure (ARF) (n=69, 71.1%) (Table 1), and the most common predisposing factor was respiratory infection (n=57; 58.8%). Microbiological aetiology could be determined in 37 patients (38.1%) (Table S1). More detailed explanation of complications prior to ICU readmission are reported in Table S2. The characteristics of patients’ included during their course in the ICU are reported in Table S3. If we only consider one time those patients who were readmitted more than once, the overall 1-year mortality was 61.8% which was significantly higher compared to the 11.4% of one-year mortality of those patients who did not need to be readmitted (p<0.001). In the multivariate analysis, the APACHE II score, number of quadrants affected in chest X-ray, and FEV1 were independently associated with mortality (Table S4). After stepwise regression analysis in which we add, once at a time, to the previous described model the apparition of different supportive therapies, the need for MV was the only significant variable associated with an increased risk of death after one year of ICU readmission (OR 35.67; IC 95% [7.73–164.53]; p<0.001) (Table S5). Only 37.1% of mechanically ventilated patients survived at 1-year of follow-up. Among patients who needed mechanical ventilation (MV) during ICU stay, the predicted probability of death at 1 year of ICU readmission was 84% (95% confidence interval 72–96%) (Table S6) (supplementary material).
Differences on baseline characteristics of the lung transplant recipients between 1-year survivors and nonsurvivors.
| Variables | All episodes(n=97) | Nonsurvivors(n=60) | Survivors(n=37) | p-Value* |
|---|---|---|---|---|
| Age (y) | 53 (13) | 54 (1) | 51 (2) | 0.191 |
| Male gender | 72 (74.2%) | 44 (73.3%) | 28 (75.6%) | 0.798 |
| Type of transplant | 0.152 | |||
| Unilateral | 43 (44.3%) | 30 (50%) | 13 (35.1%) | |
| Bilateral | 54 (55.7%) | 30 (50%) | 24 (64.9%) | |
| Underlying indication for lung transplant | 0.076 | |||
| ILD | 57 (58.8%) | 34 (56.7%) | 23 (62.2%) | |
| COPD | 23 (23.7%) | 15 (25%) | 8 (21.6%) | |
| Cystic fibrosis | 7 (7.2%) | 2 (3.3%) | 5 (13.5%) | |
| Others | 10 (10.3%) | 9 (15%) | 1 (2.7%) | |
| Complications of lung transplant prior to ICU readmission | ||||
| LRTI | 75 (80.4%) | 54 (90%) | 24 (64.9%) | 0.004 |
| Acute rejection | 48 (49.5%) | 29 (48.3%) | 19 (51.4%) | 0.836 |
| PGD | 20 (20.6%) | 13 (21.7%) | 7 (18.9%) | 0.802 |
| CLAD | 22 (22.7%) | 18 (30%) | 4 (10.8%) | 0.044 |
| CMV | 21 (21.6%) | 16 (27.6%) | 5 (13.5%) | 0.132 |
| Time after transplant to ICU admission | 11 (4–30) | 12 (6–36) | 10 (3–20) | 0.169 |
| Most recent PFT | ||||
| FEV1 (L) | 1.62 (0.63) | 1.49 (0.9) | 1.80 (0.11) | 0.028 |
| FEV1 (%) | 50 (19) | 47 (2) | 56 (4) | 0.022 |
| FVC (L) | 2.25 (0.71) | 2.14 (0.11) | 2.42 (0.11) | 0.090 |
| FVC (%) | 53 (17) | 51 (2) | 56 (3) | 0.160 |
| FEV1/FVC (%)+ | 72 (18) | 69.73 (2.58) | 74.62 (3.01) | 0.227 |
| Reason for ICU readmission | 0.474 | |||
| Acute respiratory failure | 69 (71.1%) | 44 (73.3%) | 25 (67.6%) | |
| Septic shock | 13 (13.4%) | 9 (15.0%) | 4 (10.8%) | |
| Postoperative | 12 (12.4%) | 5 (8.3%) | 7 (18.9) | |
| Decrease level of consciousness | 3 (3.1%) | 2 (3.3%) | 1 (2.7%) | |
Data are presented as mean±SD, median (interquartile range) or No./total (%).
FEV1/FVC normal values should be>70–75%.
ICU denotes intensive care unit, ILD interstitial lung disease, COPD chronic obstructive pulmonary disease, LRTI lower respiratory tract infection, PGD primary graft dysfunction, CLAD chronic lung allograft dysfunction, CMV cytomegalovirus infection, FEV1 forced expiratory volume in one second, FVC forced vital capacity.
Our report is the largest on ICU readmissions beyond the early postoperative period, and the risk factors for 1-year mortality after ICU readmission in LT patients. There is a lack of studies reporting the outcomes of long-term survivors of LT who had been readmitted to the ICU beyond 30-day from the initial ICU discharge after the ICU admission for the immediate postoperative transplantation period, even though the first year after LT and remains a high-risk period for unplanned readmissions. In a previous study reported an increased risk for within the first three months after LT.9 Other studies did not focus on ICU readmissions, analysed small samples of LT patients, or described outcomes in the early postoperative period.6,7,10,11 Of note, LT recipients who are admitted due to acute respiratory failure (ARF) have a lower survival rate compared with other solid transplant recipients.12 As observed in previous studies, high acute severity scores, and MV have been identified as significant prognostic factors.6
Despite adequate multidisciplinary medical treatment, the prognosis of LT patients with ARF who required MV is ominous. The majority of the nonsurvivors (86.7%) required MV, in contrast to 37.8% of survivors. In a previous study of 73 ICU readmissions, less than half of the patients were discharged alive from the hospital after requiring MV.13 We report less than 30% of critically ill patients requiring MV, in contrast with previous reports in which more than 50% of patients required MV.14 This may be a consequence of increased utilisation of noninvasive respiratory support techniques, such as high-flow nasal cannula and noninvasive ventilation, in immunocompromised patients during the last years.
We observed that acute infectious insults causing ARF are determinant for future prognosis, even if ARF appears to be non-severe, as suggested by the median PaO2/FiO2 ratio of ∼200 in this study. As found in previous reports, acute infection was a major risk factor for complications and ICU readmission in LT recipients.5 Indeed, previous studies found that the absence of infection has been associated with increased survival.11 As in other reports, LRTI and sepsis are usually involved in the vast majority of immediate and long-term infectious complications in LT recipients.5,6 The use of higher levels of immunosuppression and the direct exposure of the transplanted organ to the environment both increase the risk of more severe infections leading to ARF and the need for MV.
Most LT recipients who survive the first year after LT experience at least one hospital readmission10, which more likely occurs within the first 1–3 months after LT.9,10 However, ICU readmissions after this period, the number of readmissions, and the time to readmission are also determinant of LT patients’ survival. Although 80–90% of LT recipients are readmitted after LT discharge, in some institutions, the median time to first hospital readmission was 71 (28–240) days.5 Other studies have been consistent with these findings10,13. Mollberg et al. found the overall risk of death to be significantly higher with each readmission during the first year (hazard ratio, 1.22; 95% confidence interval, 1.13–1.31, p<0.0001).10 Hadjiliadis et al. reported a median time to ICU readmission of 544 days (∼18 months) to ICU admission13. In our study, the median time to ICU readmission was 11 months, which can be explained by the slightly higher median age of our sample and the worse FEV1 baseline values (50%±19 vs 67.8%±23.6) at ICU admission. As multiple readmissions have been associated with worse prognosis during the first year after transplant,5,10 interventions for improving the surveillance of patients with predisposing risk factors may decrease the change of hospital readmission.10
The increasing number of patients receiving LT entails an increased risk of complications leading to ICU unplanned readmissions. ICU readmission beyond the 30-day post-transplant period is associated with detrimental consequences. The impact of preventive interventions in that period, such as closer long-term follow-up, should be assessed.
The main limitation of this study is the lack of information on donors. Also, delays in ICU readmission were not evaluated in patients with sepsis.6 However, only 17% of ICU readmissions presented this complication.
FundingThis research has not received specific aid from agencies of the public sector, commercial sector or non-profit entities.
Conflicts of interestDr. Roca provides consultancy to Hamilton Medical, but he did not receive any personal fee. All compensations were received by the Institute of Research of his Institution. He also discloses a research grant from Hamilton Medical and speaker fees from Hamilton Medical, Ambu and Aerogen Ltd, and non-financial research support from Timpel and Masimo Corporation. All conflicts of interest are outside the submitted work. All other authors disclose no conflicts of interest.
The authors are pleased to acknowledge all healthcare staff involved in the treatment of LT patients, who provided invaluable professional interventions and humanised care to give the patients the best chances of survival.