The development of bronchial and vascular reconstruction techniques enables us to carry out lung resections that save the parenchyma. In 1947, Price-Thomas1 performed the first sleeve lobectomy in a bronchial adenoma. Later, Allison2 in 1959 reported the first case in a patient with carcinoma while also performing reconstruction of the pulmonary artery that had been infiltrated by the tumor.
Our patient is a 78-year-old male with a smoking history of 80 pack-years who had developed COPD and was being treated with bronchodilators. On the chest CT, we observed a 4-cm tumor in the LUL that was in close contact with the bronchus of the lower lobe. Bronchoscopy demonstrated that the tumor was obstructing the upper left bronchus and extended toward the bronchus of the LLL. On PET, the lesion presented an increased metabolism with bilateral perihilar and hypermetabolic mediastinal lymphadenopathies. Ultrasound-guided bronchoscopy ruled out metastasis in said lymph node stations. FEV1 was 1.610l (61%) and diffusion was 65%. A ventilation/perfusion scintigraphy showed a perfusion of 45% in the left lung.
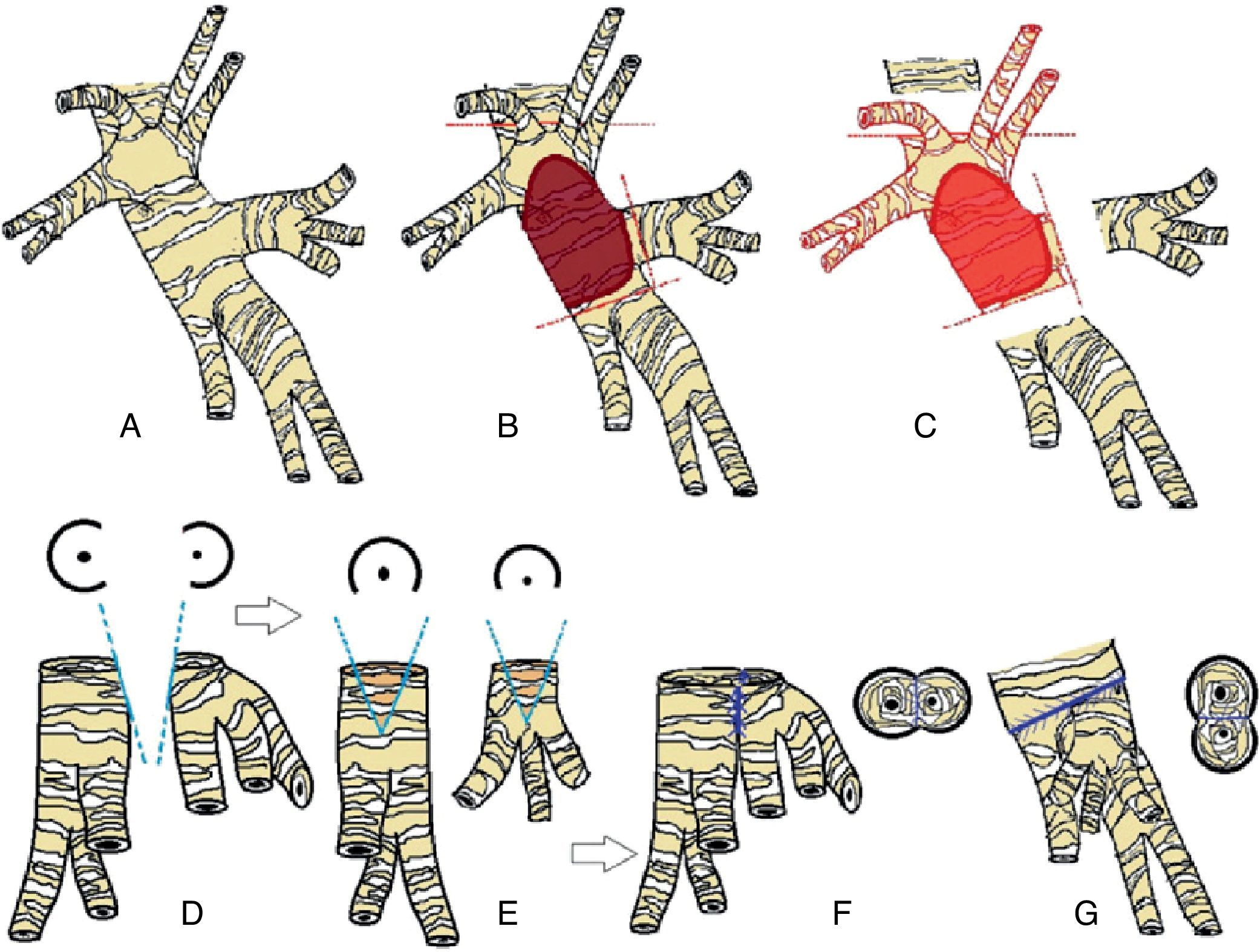
The surgical approach entailed posterolateral thoracotomy through the 5th intercostal space, observing that the tumor retracted the scissure without overpassing it. Two lobar branches of the pulmonary artery were seen to be infiltrated at their ends; therefore we carried out proximal and distal clamping after anti-coagulation with 4000 units of heparin. Later, we proceeded with the sleeve dissection of the main bronchus and bronchus of the LLL. In order to achieve an edge that was free from microscopic infiltration, it was necessary to extend the surgical margin toward the LLL with separation of the bronchus from the sixth segment and the basal pyramid (Fig. 1C). Once the lobectomy was completed, we started to reconstruct the artery with a direct suture and we then approached the bronchus. The bronchial anastomosis was done with a continuous lateral suture between the bronchus of the sixth segment and that of the basal pyramid using a 4/0 reabsorbable suture (Fig. 1F). Previously, we performed a small lateral wedge incision (Fig. 1D and E). Both bronchi joined together were anastomosed to the left main bronchus with a 3/0 reabsorbable suture using individual sutures (Fig. 1G). The discrepancy in calibers was corrected by confronting both bronchi without telescoping. A flap of pericardial fat was placed over the bronchial suture. We carried out lymphadenectomy of the prevascular, aortopulmonary window and subcarinal regions. The anatomic pathology report confirmed an epidermoid carcinoma that was moderately differentiated with disease-free resection margins with affectation of one of the peribronchial lymph nodes (pT2N1M0). The postoperative evolution was satisfactory.
(A) Anatomy of the left bronchus, lateral view. (B) Area of bronchial infiltration. (C) Resection of the affected bronchial area separating the segmental bronchi of the LLL. (D and E) Wedge incision over the bronchus of the basal pyramid and the bronchus of segment six. (F) Lateral anastomosis between segmental bronchi, lateral view. (G) Anastomosis of segmental bronchi to left main bronchus, posterior view.
When other prognostic variables are controlled, such as lymph node affectation, patients with bronchoplastic lobectomies with N0–N1 affectation have better survival than patients who underwent pneumonectomy.3–5 We would like to highlight that sublobar bronchoplastic reconstruction is possible with proper surgical technique. The intervention that we describe represents a good alternative to bronchoplastic lobectomy with segmentectomy of the sixth segment, as demonstrated by the excellent postoperative outcome.
Please cite this article as: Peña E, et al. Reconstrucción broncovascular compleja. Descripción de una técnica novedosa de broncoplastia segmentaria. Arch Bronconeumol. 2012;48:345–6.