Intermediate respiratory care units (IRCU) provide continuous monitoring and non-invasive mechanical ventilation (NIMV) in patients with severe respiratory failure who are usually admitted to intensive care units (ICUs). The usefulness of IRCU in managing severe asthma exacerbations has never been evaluated.
MethodsClinical data were prospectively and systematically compiled from patients admitted to the IRCU with a principal diagnosis of bronchial asthma exacerbation. We assessed therapeutic failure (intubation or exitus) and patient evolution up until 6 months after discharge compared with a group of patients admitted to a conventional hospital ward, paired for age and sex, and with the same principal diagnosis.
ResultsA total of 74 asthma patients were included (37 admitted to IRCU and 37 to the hospital ward) with a mean age (±SD) of 58±20, who were predominantly women (67%), with previous diagnosis of asthma and persistent asthma treatment. The main cause of admittance to the IRCU was severe respiratory failure. The patients who were admitted to the IRCU presented more radiological affectation (alveolar infiltrates) and had significantly higher pCO2. Ten patients admitted to the IRCU required non-invasive mechanical ventilation (NIMV). There were no differences between the two groups regarding either therapeutic failure or the 6-month follow-up after discharge.
ConclusionsPatients with severe asthma exacerbations can be managed in an IRCU while avoiding hospitalization in an ICU and demonstrating a prognosis similar to milder exacerbations treated in conventional hospital wards.
Las unidades de cuidados respiratorios intermedios (UCRI) permiten la monitorización continua y la ventilación mecánica no invasiva (VMNI) en los pacientes con insuficiencia respiratoria grave que habitualmente ingresan en Unidades de Cuidados Intensivos (UCI). La utilidad de las UCRI en el manejo de las agudizaciones graves del asma nunca ha sido evaluada.
MétodosSe recogieron de forma prospectiva y sistemática los datos clínicos de pacientes ingresados en la UCRI con el diagnóstico principal de asma bronquial agudizada, se evaluó el fracaso terapéutico (intubación o éxitus) y su evolución hasta 6 meses tras el alta, comparada con un grupo de pacientes ingresados en planta de hospitalización convencional pareados por edad y sexo, con el mismo diagnóstico principal.
Resultadosse incluyeron un total de 74 pacientes asmáticos (37 ingresan en UCRI y 37 en planta) con edad media (±DS) de 58±20 años, predominantemente mujeres (67%), con diagnostico previo y tratamiento de asma persistente. La causa principal de ingreso en la UCRI fue insuficiencia respiratoria grave. Los pacientes que ingresaron en la UCRI presentaron más afectación radiológica (infiltrados alveolares) y tenían una pCO2 significativamente mayor. Diez pacientes ingresados en UCRI precisaron ventilación mecánica no invasiva (VMNI). No hubo diferencias entre ambos grupos en fracasos terapéuticos, ni en seguimiento a los 6 meses del alta.
ConclusionesLos pacientes con agudizaciones graves del asma pueden ser manejados en una UCRI, evitando ingresos en UCI y con pronóstico similar a las agudizaciones mas leves que son ingresadas en planta de hospitalización convencional.
Bronchial asthma is one of the most common chronic illnesses in the world, with an incidence which varies between 1% and 18% depending on the country.1–3 According to information from this country, the incidence of asthma in adults oscillates between 1% and 5%, depending on the province.4
According to the World Health Organisation asthma causes 250 000 deaths every year.5 During the last decade, several different epidemiological studies showed that the mortality rate has levelled off or decreased in a number of countries.6,7
Asthma progresses with exacerbations which may: (i) develop slowly, in which case it is frequently associated with upper airway respiratory infections or difficulty in controlling the illness or (ii) develop quickly, in which case it is associated with inhaled allergens and the ingestion of drugs (AINE or beta-blockers), certain food-stuffs (due to additives and preservatives) or emotional stress; the latter are initially more serious (with a risk of intubation an death), but the response to treatment is better and faster. The intensity of the exacerbations is variable, in some cases progressing with light symptoms which may go unnoticed by the patient, and in others through a series of extremely serious episodes in which the patient's life may be in danger.8,9
Around 30% of the asthmatic exacerbations attended to in the emergency services of a hospital require hospitalisations.10,11 GINA (Global Initiative for Asthma) classifies the exacerbations as light, moderate, serious and almost fatal, depending on the patient's condition upon being examined.1 Incidence varies considerably depending on the definition used: between 49% and 16% for serious exacerbations and between 26% and 3% for almost fatal ones.10,12 Between 2% and 20% of all serious asthma exacerbations require intensive care, and between 10% and 63% present hypercapnia, while the need for tracheal intubation varies from 2% to 70%.13
Recently, a number of intermediate respiratory intensive care units (ICRUs) have emerged. These units make it possible for the patient to be monitored continuously and mechanical ventilation to be carried under the best possible conditions.14 To date no studies have been published to highlight the role that these units could play in the evolution and prognosis of patients with serious and acute deteriorations of their asthmatic condition.
The aim of the present study is to describe the characteristics and prognosis of asthmatic patients admitted to the ICRU of our centre with a primary diagnosis of acute asthmatic deterioration, as compared with the same number of patients admitted to the conventional hospital ward.
MethodsLocation of the StudyThe University Hospital of Son Dureta (HUSD, now known as the University Hospital of Son Espases) belongs to the Balearic Health-care System (Ib-Salut) and is the main hospital for a population of some 955,045 inhabitants of the Balearic Islands.
The ICRU of the HUSD Pulmonology Service was opened in December 2005. It forms part of the Pulmonology section of the hospital, and has 4 beds with an open physical structure, each of which is equipped with a monitor to register cardio-respiratory activity, ventilation equipment for non-invasive ventilation, a nurse and 24-h medical attention from a pulmonologist. Bearing in mind that the ICRU forms part of the Pulmonology section, and despite the fact that it functions independently of conventional hospitalisation, the costs incurred are not analysed separately. Thus the cost of a bed in the Pulmonology Service, irrespective of whether it is in the ICRU or in a conventional ward, is estimated to be 515 EUR per day. By contrast, in our hospital the cost of a bed in the ICU is estimated at 1100 EUR per day, more than double what it costs in the Pulmonology section.
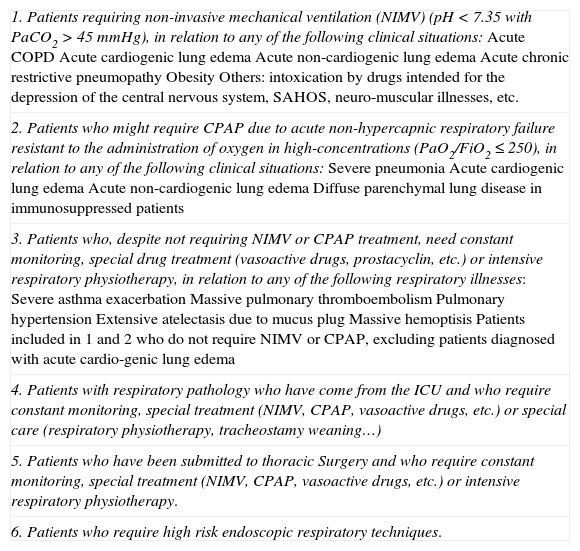
The criteria for admission to the ICRU of the HUSD are shown in Annex 1.
Study DesignThe study is prospective and observational. Between December 2005 and April 2009, inclusive, all the patients admitted to the ICRU with a primary diagnosis of acute bronchial asthma were systematically included in the study, and they were compared with a group of patients who had been admitted to the Pulmonology section of the hospital with the same diagnosis during the same period, according to sex and age. Clinical follow-up was carried out 6 months after discharge. To be precise, the following variables were analysed: (1) characteristics of the patient (age, sex, history of tobacco smoking, respiratory function tests), (2) characteristics of the asthma in question (number of years, clinical seriousness and admissions during the preceding year, treatment received, comorbidity), (3) characteristics of admission (cause, sputum cultures, length of stay in hospital, arterial blood gas examination and peak-flow on admission and discharge, and number of therapeutic failures: in other words, the number of patients who had to be transferred to the ICU and the number of patients who died in the unit) and (4) follow-up after 6 months (number of deteriorations and admissions, exitus).
Statistical AnalysisIn the descriptive statistical analysis means and standard deviations were used for the continuous variables, and frequencies and percentages were used for the categories. As regards the comparisons between the groups of patients (ICRU as opposed to conventional hospital), the Student's t test was used for the continuous variables, and the χ2 test or the Fisher exact test for the categories. Values of p<.05 were established as significant. For the statistical processing of the data, the IBM SPSS Statistics 19 programme was used.
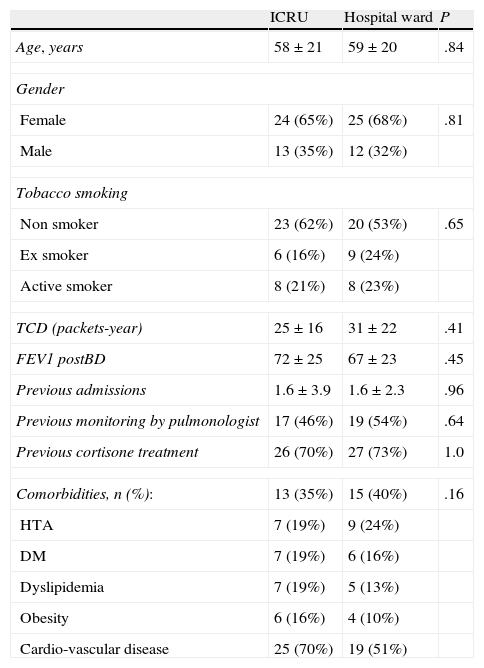
ResultsDuring the period of the study, 37 patients were admitted to the ICRU in our service with a primary diagnosis of deterioration of their asthmatic condition (which was 5.2% of the total number of patients in the ICRU) and 436 patients under conventional hospitalisation conditions with the same diagnosis. The characteristics of the subjects included, both the ICRU group and those hosptialised conventionally are shown in Table 1. When both groups are compared, no significant differences are found in relation to the patients and the illnesses they suffer from.
Characteristics of the Asthma Patients Admitted to the ICRU and the Hospital Wards.
| ICRU | Hospital ward | P | |
| Age, years | 58±21 | 59±20 | .84 |
| Gender | |||
| Female | 24 (65%) | 25 (68%) | .81 |
| Male | 13 (35%) | 12 (32%) | |
| Tobacco smoking | |||
| Non smoker | 23 (62%) | 20 (53%) | .65 |
| Ex smoker | 6 (16%) | 9 (24%) | |
| Active smoker | 8 (21%) | 8 (23%) | |
| TCD (packets-year) | 25±16 | 31±22 | .41 |
| FEV1 postBD | 72±25 | 67±23 | .45 |
| Previous admissions | 1.6±3.9 | 1.6±2.3 | .96 |
| Previous monitoring by pulmonologist | 17 (46%) | 19 (54%) | .64 |
| Previous cortisone treatment | 26 (70%) | 27 (73%) | 1.0 |
| Comorbidities, n (%): | 13 (35%) | 15 (40%) | .16 |
| HTA | 7 (19%) | 9 (24%) | |
| DM | 7 (19%) | 6 (16%) | |
| Dyslipidemia | 7 (19%) | 5 (13%) | |
| Obesity | 6 (16%) | 4 (10%) | |
| Cardio-vascular disease | 25 (70%) | 19 (51%) | |
DM: diabetes mellitus; TCD: total cumulative dosage; FEV1 postBD: measured forced expiratory volume in the second post-broncho-dilator; HTA: arterial hypertension. The data are expressed as numbers and percentages, or with mean standard±deviation (X±SD).
With reference to the ICRU, 10 patients were treating themselves at home with short-acting beta-2 adrenergic drugs, 22 patients were receiving treatment with inhaled cortisone, most of them in combination with long-action beta-2 adrenergic drugs, 4 patients were taking systemic cortisone and only 1 patient was not under any kind of treatment. Approximately half of the patients were being monitored regularly by a pulmonologist, and 55% had required one or more hospital admissions due to a deterioration of their bronchial asthmatic condition.
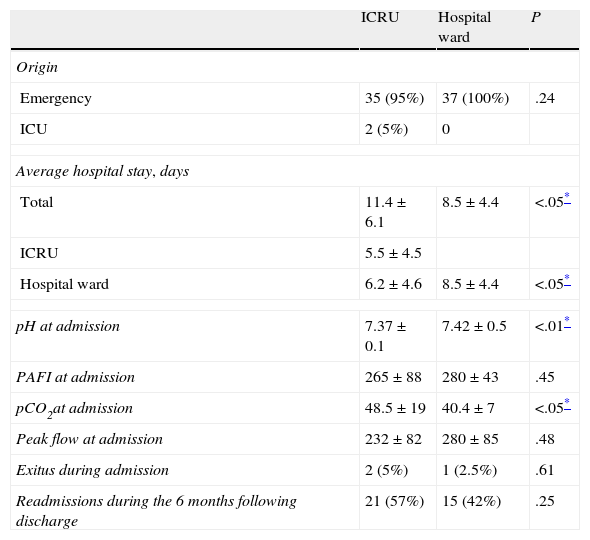
95% of the patients hospitalised in the unit had come from the emergency service, while the rest, 2 patients, had been transferred from the ICU. The most common causes of admission were severe respiratory insufficiency and hypercapnia, with the patients presenting a coefficient value for pressure arterial oxygen/fraction of inspired oxygen (PAFI) of 265±88 and 345±66, pressure arterial carbon dioxide of 48.5±19 and 43.2±7mmHg, and a peak-flow of 232±82 and 394±86l/min upon admission and discharge respectively.
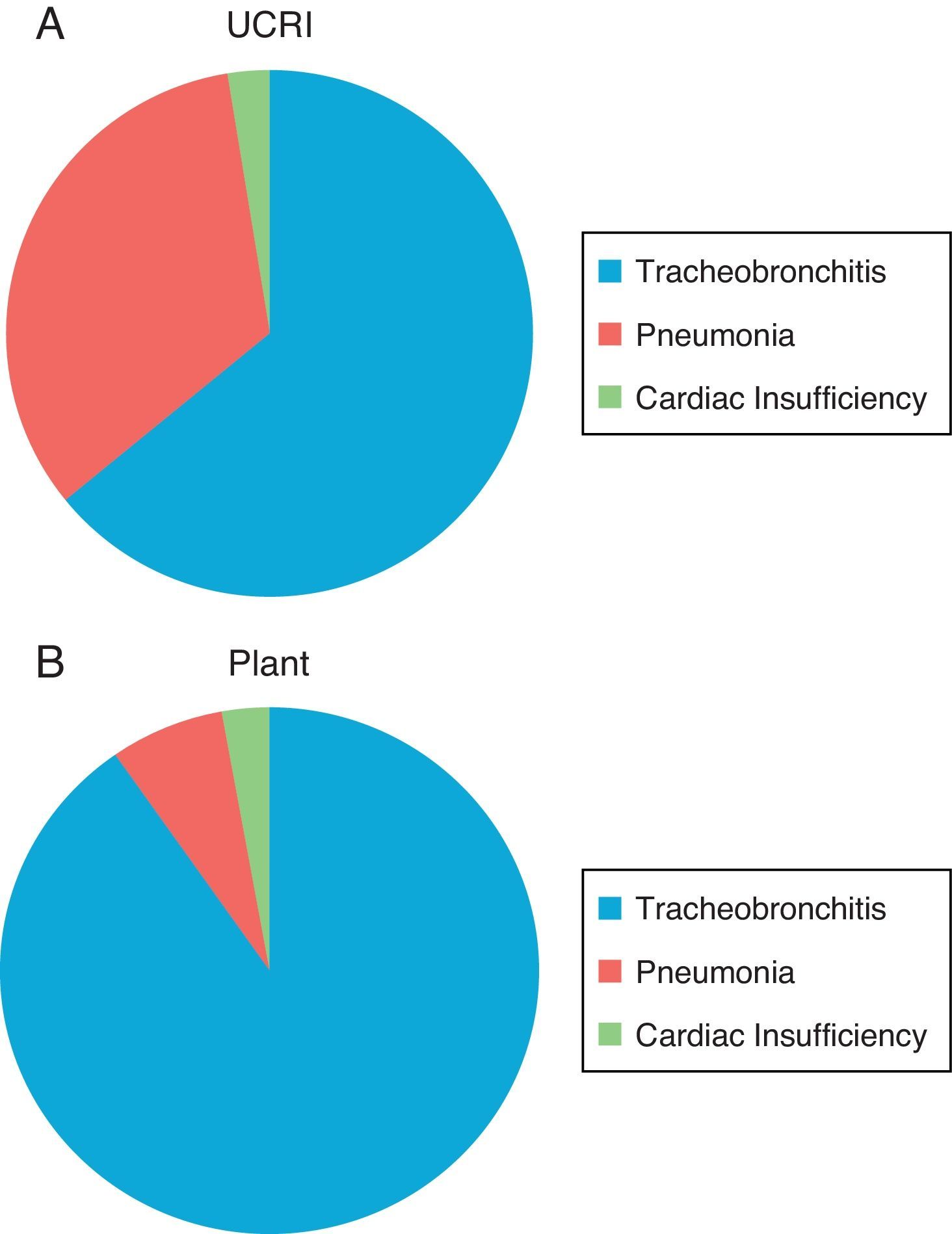
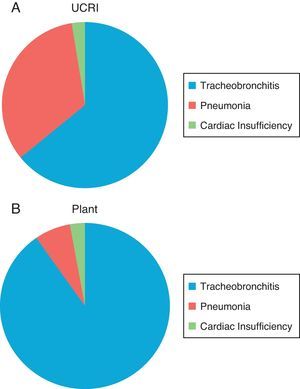
The most frequent cause of exacerbation of the asthma was acute tracheobronchitis (62%) (Fig. 1). Thirteen patients presented fresh alveolar infiltrates in the thoracic X-ray, interpreted as pneumonia/atelectasis and one as cardiac insufficiency. The origin of these episodes was confirmed with sputum cultures in 24% of the cases, the following germs being the most frequent: Streptcoccus pneumoniae (2), Pseudomona aeruginosa (2), Staphylococcus aureus resistant to methicillin tracheostomy (2), Escherichia coli (2) and Klebsiella pneumoniae (1).
Ten patients required NIMV during an average of 5.8±4.7 days, and all of them presented associated pathologies such as obesity (n=5), kyphoscoliosis (n=3) or bronchiectasis (n=2). In 9 of the 10 cases, the reason for the NIMV was acute hypercapnic respiratory failure. The average stay in the unit was 5.5±4.5 days. Therapeutic failure occurred in 8% of the cases (defined as the need for tracheal intubation or exitus), 1 patient with asthma aggravated by pneumonia due to Legionella had to be transferred to the ICU and required intubation with mechanical ventilation and 2 patients, for whom aggressive manipulation would not have been appropriate, were exitus.
Six months after discharge, 6% of the patients died and 65% required readmission.
Upon comparison between the group admitted to the ICRU and the group hospitalised under conventional conditions, it was observed that the ICRU group had a tendency towards greater comorbidity, presented more cases of pneumonia as a cause of bronchial asthmatic exacerbation (13 vs 3, P>.05) and in the blood gases examination there was a lower pH content (7.37±0.11 vs 7.42±0.04, P<.05) and a higher pCO2 content (48.6±19.3 vs 40.4±6.8mmHg, P<.05). Besides the ICRU group, 10 other patients received NIMV treatment, while in the group from the conventional hospital ward only 1 did, which he had already been under treatment with at home. As regards the evolution of the condition during hospitalisation and 6 months after discharge, no differences were observed between the groups in terms of readmission or mortality. Table 2 shows the results of the variables recorded during hospitalisation for both groups.
Characteristics of the Asthmatic Exacerbation Episode Among ICRU Patients as Compared With Conventionally Hospitalised Ones.
| ICRU | Hospital ward | P | |
| Origin | |||
| Emergency | 35 (95%) | 37 (100%) | .24 |
| ICU | 2 (5%) | 0 | |
| Average hospital stay, days | |||
| Total | 11.4±6.1 | 8.5±4.4 | <.05* |
| ICRU | 5.5±4.5 | ||
| Hospital ward | 6.2±4.6 | 8.5±4.4 | <.05* |
| pH at admission | 7.37±0.1 | 7.42±0.5 | <.01* |
| PAFI at admission | 265±88 | 280±43 | .45 |
| pCO2at admission | 48.5±19 | 40.4±7 | <.05* |
| Peak flow at admission | 232±82 | 280±85 | .48 |
| Exitus during admission | 2 (5%) | 1 (2.5%) | .61 |
| Readmissions during the 6 months following discharge | 21 (57%) | 15 (42%) | .25 |
A reduction was observed in the number of patients requiring admission to the ICU during the study due to deterioration of the bronchial asthma as the primary diagnosis (9 patients), compared with the same period of time (41 months) prior to the opening of the ICRU (19 patients).
DiscussionThe present study demonstrates that there is a group of asthmatic patients with greater comorbidity and more severe deteriorations of their bronchial asthmatic condition, frequently associated with respiratory acidosis, who benefit from treatment in an intermediate care unit. This benefit is based on the fact that the rate of admission to the ICU and a prognosis after 6 months is similar to deteriorations requiring admission to a conventional hospital ward, with a corresponding saving in health service costs, as, in the absence of these units, the patients in question would be admitted directly to the ICU.
Approximately 30% of the bronchial asthma deteriorations10 require hospitalisation, and up to 20% require ICU treatment.13Up to 40% of the patients in medical ICUs and 30% in surgical ICUs are admitted for the purpose of continuous monitoring, and not with a view to carrying out any specific therapeutic action.15 It has been observed that it is possible to reduce costs and improve the quality of ICUs in general by means of the use of ICRUs for patients coming out of an ICU, or for semi-critical patients or those whose condition is an intermediate degree of severity.15–17
To date there are two Spanish studies which have published data concerning a ICRU linked to a Pulmonology service collected during the course of one year. Sala et al. presented their data from the unit's activity obtained during the year 2006, with 206 admissions, 8 of which (3.9%) were due to asthmatic deteriorations.18 Similar results were obtained by the group at the Galdákano hospital, where out of a total of 212 admissions, 7 (3.3%) were due to acute asthmatic deterioration, 4 of whom required NIMV and 1 was exitus 90 days after discharge.19
The results of our study show that the asthmatic patients who are admitted to the ICRU are patients with greater comorbidity, a greater degree of hypercapnia and are shown in scans to be more severely affected than asthmatic patients admitted to the conventional hospital wards. Examinations of patients with severe deterioration have shown these factors to point to a negative prognosis.20,21 The microbiological profile encountered in these patients, with prevalence of Gram negatives and germs predominantly associated with hospital environments, confirms the greater severity characterising the condition of these patients.
Of the 37 patients admitted to our ICRU, 10 received NIMV treatment, of whom 2 died and 12 required admission to the ICU with tracheal intubation. The NIMV in the event of acute respiratory failure provides adequate ventilation support until the illness causing the deterioration improves or is dealt with by the appropriate medical treatment. In a number of different illnesses such as exacerbation of chronic obstructive pulmonary disease or acute lung edema, NIMV has been shown to be effective, as it reduces the need for tracheal intubation and mortality.22,23 The use of NIMV in asthmatic exacerbation is controversial. In 2009, a Cochrane review was published, the purpose of which was to determine the effectiveness of NIMV in the deterioration of asthma. It was only possible to include one clinical assay which demonstrated that the use of NIMV reduced the number of hospital admissions, increased the number of discharges from emergency services and improved the respiratory frequency and the parameters of lung function. But despite this its use remains controversial, which is the reason why more studies are needed.24Recently a review was published concerning the use of NIMV in asthmatic exacerbations. Despite the contradictory nature of certain studies with very small study populations, the authors conclude that, in an appropriate environment such as an ICU or ICRU, and with an experienced respiratory medical team, NIMV can be tried on certain patients.25 The rate of intubation and connection to a mechanical ventilator in severe asthmatic exacerbations varies between 2 and 60%.26–28
One of the aims of the ICRU is to reduce costs, by avoiding transfer to an ICU and encouraging rapid discharge from the latter.15–17 In the specific case of our hospital, in which the ICU bed incurs approximately double the cost of a ICRU bed, and is similar to that of a bed in a normal ward, our patients benefit from close monitoring without a corresponding increase in the cost of health care.
The present study has a series of limitations: (a) it is an observational study, which means that the results obtained cannot be used to establish causal relationships between the variables being studied, (b) it does not compare the results obtained in the ICRU with patients transferred to the ICU with the same characteristics, (c) the study sample is small, due to the clinical characteristics of the pathology being studied and (d) it did not take account of exposure to allergens as a cause of exacerbation.
In conclusion, this study provides information concerning patients with severe asthmatic exacerbations admitted to a ICRU linked to the Pulmonology Service which could be a useful alternative to admission to an ICU. Furthermore, it could serve to promote the development of other ICRUs in hospitals across the Spanish National Health Service.
FundingNone.
Conflict of InterestNone.
The authors wish to thank Maria Eugenia Torres, Joan Tortell Marimón and Francisco Javier Sansó Gayá from the computer and clinical documentation departments of the Son Espases University Hospital for their help in obtaining the necessary information.
Admission criteria for the Intermediate Respiratory Care Unit of the Son Dureta University Hospital
| 1. Patients requiring non-invasive mechanical ventilation (NIMV) (pH<7.35 with PaCO2>45mmHg), in relation to any of the following clinical situations:Acute COPDAcute cardiogenic lung edemaAcute non-cardiogenic lung edemaAcute chronic restrictive pneumopathyObesityOthers: intoxication by drugs intended for the depression of the central nervous system, SAHOS, neuro-muscular illnesses, etc. |
| 2. Patients who might require CPAP due to acute non-hypercapnic respiratory failure resistant to the administration of oxygen in high-concentrations (PaO2/FiO2≤250), in relation to any of the following clinical situations:Severe pneumoniaAcute cardiogenic lung edemaAcute non-cardiogenic lung edemaDiffuse parenchymal lung disease in immunosuppressed patients |
| 3. Patients who, despite not requiring NIMV or CPAP treatment, need constant monitoring, special drug treatment (vasoactive drugs, prostacyclin, etc.) or intensive respiratory physiotherapy, in relation to any of the following respiratory illnesses:Severe asthma exacerbationMassive pulmonary thromboembolismPulmonary hypertensionExtensive atelectasis due to mucus plugMassive hemoptisisPatients included in 1 and 2 who do not require NIMV or CPAP, excluding patients diagnosed with acute cardio-genic lung edema |
| 4. Patients with respiratory pathology who have come from the ICU and who require constant monitoring, special treatment (NIMV, CPAP, vasoactive drugs, etc.) or special care (respiratory physiotherapy, tracheostamy weaning…) |
| 5. Patients who have been submitted to thoracic Surgery and who require constant monitoring, special treatment (NIMV, CPAP, vasoactive drugs, etc.) or intensive respiratory physiotherapy. |
| 6. Patients who require high risk endoscopic respiratory techniques. |
Please cite this article as: Núñez B, et al. Características de pacientes asmáticos ingresados en una unidad de cuidados respiratorios intermedios. Arch Bronconeumol. 2013;49:146–50.