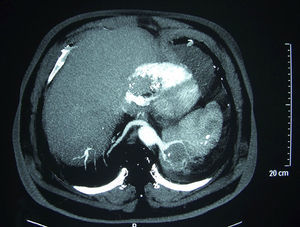
We present the case of a 64-year-old man, ex-smoker, with clinical indicators of chronic bronchitis. He had been on home oxygen for more than 10 years and was on treatment for sleep apnoea-hypopnoea syndrome (SAHS) with nocturnal continuous positive airway pressure (CPAP). He was admitted in 1990 for pneumonia in the left lower lobe (LLL), secondary to symptoms of near-drowning in seawater. During the follow-up, triangular consolidation persisted in the LLL, but both computed tomography (CT) and fibrobronchoscopy failed to provide a diagnosis. CT-guided transthoracic needle aspiration was performed, with cytology negative for malignancy and a negative microbiological study. The patient was admitted on several occasions in recent years for exacerbation of COPD. A new chest CT scan was requested in 2004 due to consolidation in the LLL, and he was diagnosed with possible left intralobar pulmonary sequestration (PS). The patient refused any further studies. In 2009, he was admitted for pneumonia. The chest CT scan (Fig. 1) showed a 6–7-cm complex formation, in a medial location in the LLL, supplied by a large vessel originating in the inferior thoracic artery with drainage to pulmonary veins, corresponding to an intralobar PS with probable superinfection; in a symmetrical location, contralateral, there was another abnormal vessel, also originating in the aorta, corresponding to another intralobar PS in the right region. After improvement with treatment, he was discharged for follow-up at the clinic, but did not attend his check-ups. Most intralobar PS are unilateral, and bilateral PS are very rare.1 For Kohler, PS was first described by Rokitanski and Rektorzik in 1861, but it was not until 1946 when Pryce2 made it known as a clinical entity. In 1972, Felson et al.3 reported a case of bilateral PS confirmed by pathological examination. In 1977, Karp et al.1 described another case in a 13-year-old girl who presented a mass in the LLL, discovered after a chest radiograph. CT scanning and pulmonary arteriography were carried out, showing a left intralobar PS, already suspected, and a right PS that was not previously observed. A few cases have been published since then, similar in that they concern paediatric or adolescent patients. In 2009, Yamamura et al.4 explained the surgical procedure performed on a 44-year-old patient who presented bilateral intra- and extralobar PS. Wei and Li5 analysed 2625 cases of PS in 2011, among which only 3 were bilateral and 2 of these intralobar. The case presented is doubly unique in that this is an older patient with bilateral intralobar PS. He presented recurrent pneumonia with a changing aspect in the LLL, in which diagnostic tests were inconclusive. The possibility of PS had already been described in the CT scan prior to his current admission. The existence of recurrent consolidations, especially if they occur in the LLL, requires us to consider the differential diagnosis of various conditions such as PS, long-standing pneumonia, chronic obstructive disease or lung tumours.6 The diagnosis of PS has traditionally required pulmonary angiography to demonstrate abnormal vascularisation. However, new techniques such as next-generation CT angiography enable high resolution vascular reconstructions that could circumvent arteriography, as well as revealing congenital malformations, thereby avoiding more invasive techniques. With respect to treatment, we would propose acting on the left PS (as it is the symptomatic one) using surgery or VATS, the latter technique being less invasive.
Please cite this article as: Fontalba Navas M, et al. Secuestro pulmonar bilateral en el adulto: aportación de un caso y revisión de la literatura. Arch Bronconeumol.2013;49:410–11.