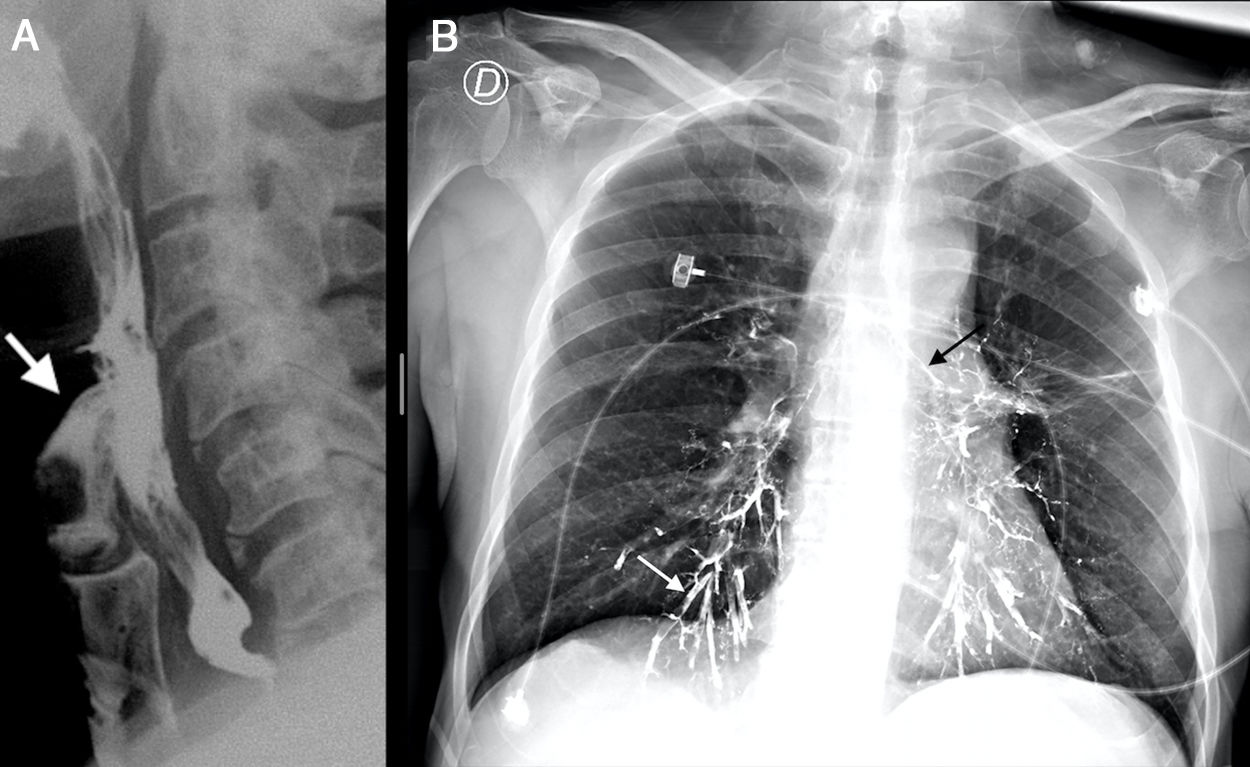
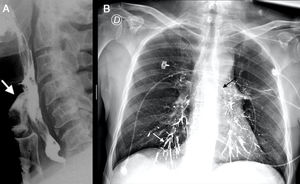
A 70-year-old male patient, with history of chronic obstructive pulmonary disease and EGFR, ALK negative lung adenocarcinoma T1a N3 M0 – Stage IIIB, who was previously treated with Carboplatin, Pemetrexed and radiotherapy, suffered cervical lymph node relapse histologically compatible with adenocarcinoma. He presented to the emergency with a 6-month-history of dysphagia and dysphonia that rapidly progressed in the last seven days. Laryngoscopy revealed left cordal paralysis with deflection to the right of the upper part of the trachea by extrinsic compression. Subsequently, conventional barium esophagography (Fig. 1A) was performed showing the presence of radiopaque material in the upper third of the esophagus. A stenotic lesion prevented the passage of contrast that leaked into the larynx, leading to aspiration which was radiologically and clinically evident with worsening of the respiratory symptoms. The study was immediately suspended and he was transferred to the intensive care unit where new X-rays (Fig. 1B) revealed barium staining of both main stem bronchi, lobar bronchi and basal bronchioles with predominance in lower lobes. He developed respiratory failure leading to endotracheal intubation and mechanical ventilation for four days. Tracheostomy was made, followed by upper digestive endoscopy where an extrinsic expansive lesion without signs of organ invasion was found at 18cm, responsible of the obstruction. Afterwards, gastrostomy was performed for enteral feed. Due to the presence of a locally advanced disease, Pemetrexed, Atezolizumab and radiotherapy was started showing a size reduction of the cervical mass allowing him to start oral feeding again. He was later discharged.
The Impact Factor measures the average number of citations received in a particular year by papers published in the journal during the two preceding years.
© Clarivate Analytics, Journal Citation Reports 2025
SRJ is a prestige metric based on the idea that not all citations are the same. SJR uses a similar algorithm as the Google page rank; it provides a quantitative and qualitative measure of the journal's impact.
See moreSNIP measures contextual citation impact by wighting citations based on the total number of citations in a subject field.
See more