The prevalence of chronic respiratory diseases (CRDs), including chronic bronchitis and chronic obstructive pulmonary disease (COPD), has increased significantly over the past decades. Several studies suggested that Helicobacter pylori infection may be related to the development of CRDs, but the results were not consistent. We carried out a meta-analysis to evaluate the potential association of H. pylori infection with CRDs.
MethodsWe conducted a systematic literature search in PubMed, Embase, Ovid, Google Scholar and CNKI from inception to October 31, 2013. The following search terms were used: “chronic respiratory disease,” “chronic bronchitis,” “chronic obstructive pulmonary disease” or “COPD” in combination with “Helicobacter pylori” or “Campylobacter pylori.” According to established inclusion criteria, we selected all eligible published papers and then extracted essential data. To evaluate the association of H. pylori with chronic bronchitis and COPD, an overall analysis and subgroup analyses were conducted.
ResultsA total of 9 case–control studies comprising 782 cases and 815 controls were included in the study. Pooled ORs were 2.30 (95% CI: 1.85–2.85) in the overall analysis, 2.90 (95% CI: 2.04–4.13) in the chronic bronchitis subgroup, and 2.11 (95% CI: 1.35–3.29) in the COPD subgroup.
ConclusionsThe results of the overall analysis and subgroup analyzed suggest a significant association between H. pylori and CRDs. Further studies are needed to clarify the pathogenetic mechanisms involved.
La prevalencia de las enfermedades respiratorias crónicas (ERC), incluida la bronquitis crónica y la enfermedad pulmonar obstructiva crónica (EPOC), ha aumentado de manera significativa a lo largo de las últimas décadas. Varios estudios han sugerido que la infección por Helicobacter pylori puede estar relacionada con la aparición de las ERC, pero los resultados presentados no han sido uniformes. Con el objetivo de evaluar la posible asociación de la infección por H. pylori con las ERC, llevamos a cabo el presente metaanálisis.
MétodosRealizamos una búsqueda bibliográfica sistemática en PubMed, Embase, Ovid, Google Scholar y CNKI desde su inicio hasta el 31 de octubre de 2013. Los términos de búsqueda utilizados fueron los siguientes: «chronic respiratory disease», «chronic bronchitis», «chronic obstructive pulmonary disease» o «COPD» en combinación con «Helicobacter pylori» o «Campylobacter pylori». Según los criterios de inclusión establecidos, seleccionamos todos los artículos publicados elegibles y extrajimos los datos esenciales. Para evaluar la asociación de H. pylori con la bronquitis crónica y la EPOC se realizó un análisis global y se llevaron a cabo diversos análisis de subgrupos, respectivamente.
ResultadosFinalmente se incluyeron en los análisis un total de 9 estudios de casos y controles en los que se incluyeron 782 casos y 815 controles. La OR combinada fue de 2,30 (IC 95%: 1,85–2,85) para el análisis global, de 2,90 (IC 95%: 2,04–4,13) para el análisis del subgrupo de bronquitis crónica y de 2,11 (IC 95%: 1,35–3,29) para el análisis del subgrupo de EPOC.
ConclusionesLos resultados del análisis global y de los análisis de subgrupos sugieren una asociación significativa entre H. pylori y ERC. Serán necesarios nuevos estudios para esclarecer los mecanismos patogénicos.
The prevalence of chronic respiratory diseases (CRDs), including chronic bronchitis and chronic obstructive pulmonary disease (COPD), has increased significantly over the past decades.1 The etiology of CRDs is well known to be complex. Certain risk factors, such as age, tobacco use and atmospheric pollution, are closely related with CRDs.2,3
Helicobacter pylori, a spiral-shaped, gram-negative bacterium, has been implicated in the risk of gastroduodenal ulcer and gastric cancer.4 In previous studies, increased prevalence of H. pylori seropositivity has been observed in association with several diseases, such as certain heart diseases5 and allergies.6
To date, several studies, including systematic reviews and meta-analyses, have been performed to evaluate the association between H. pylori and respiratory diseases such as asthma,7 pulmonary tuberculosis8 and lung cancer.9 However, no quantitative systematic review has studied the relationship between chronic bronchitis or COPD and H. pylori infection. Although the association between H. pylori infection and CRD has been investigated in different studies,10 results were inconsistent, with some studies indicating no evidence for a relationship between H. pylori and CRD,11 and other suggesting a close relationship.12
In order to clarify the association between CRD and H. pylori, we reviewed the literature and produced the first meta-analysis in this area. The possible association may broaden our understanding of the pathological mechanism of CRDs and contribute to their prevention.
Material and MethodsLiterature Search StrategyA systematic search was made of the literature, with no limitations for language, in PubMed, Embase, Ovid, Google Scholar and China National Knowledge Infrastructure (CNKI) from inception to October 31, 2013. Search terms used were “chronic respiratory disease”, “chronic bronchitis”, “chronic obstructive pulmonary disease” or “COPD”, combined with “Helicobacter pylori” or “Campylobacter pylori”. When the search retrieved an article in a language other than English, the abstracts were examined for possible inclusion, and the complete texts were then read for any possibly relevant information. Publications that could be of interest were evaluated by examination of the titles and abstracts. The full texts of clearly relevant articles were then obtained for a more detailed examination. Other relevant articles that could have been missed in the initial search were also screened.
Inclusion and Exclusion CriteriaCriteria for the selection of articles were: (a) the association of H. pylori infection with CRDs had to be clearly described in the studies; (b) the diagnosis of H. pylori infection and the number of cases and controls had to be specified; (c) the sample size, odds ratio (OR) and 95% confidence intervals (CI) or else the data needed for inferring these parameters had to be given; (d) data sourcing and analysis methodology had to be acceptable from a statistical point of view, and (e) studies had to be case-controlled.
The following exclusion criteria were also applied: (a) duplicated publications and reviews; (b) studies with a design and definition manifestly different from the inclusion criteria; (c) non-case–control studies, and (d) lack of information regarding the number of cases and controls and other essential data. After an intensive search, all articles were reviewed according to the above criteria, and a more detailed analysis was made.
Data ExtractionData from all eligible publications were carefully extracted by 2 of the authors, working independently, applying the above-mentioned inclusion criteria. In case of discrepancy, consensus was reached by discussion. If no agreement could be reached, the other author was consulted to settle the controversy, and a final decision was reached by majority vote. Collected data were entered in a database.
Evaluation of Methodological QualityThe methodological quality of all case–control studies was evaluated using the Newcastle–Ottawa Scale (NOS).13 The NOS is based on the semiquantitative principle, and rates quality according to a star system by which studies are awarded 0–9 stars.
Statistical AnalysisOdds ratios (ORs) were estimated for CRDs associated with H. pylori for each study. To detect any possible bias in sample size, the ORs and 95% confidence intervals (CI) of each study were plotted against the corresponding number of participants.
Statistical heterogeneity was analyzed using the Q statistic and a value of P<.05 was considered statistically significant. If the result of the heterogeneity test was I2>50%, the random effects model (DerSimonian and Laird)14 was used for the meta-analysis. Otherwise, the ORs were combined according to the fixed effects model (Mantel and Haenszel).15 The Z-test was used to determine the significance of the combined OR. Publication bias was evaluated by the fail-safe number (Nfs0.05) for P-values lower than .05 (P<.05).16 Statistical analysis was performed using Review Manager 5.2 software.
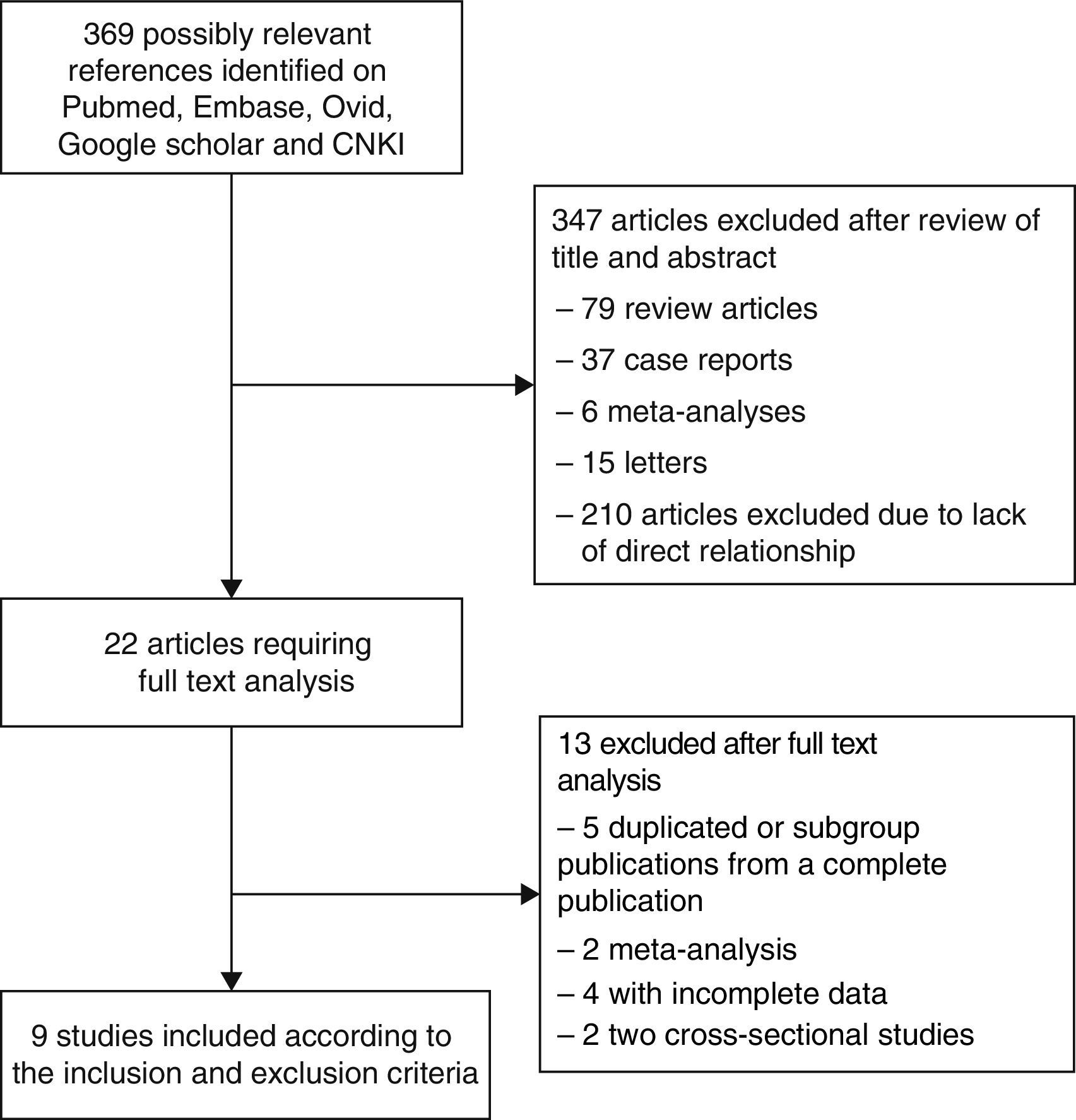
ResultsLiterature Search and Meta-Analysis DatabaseUsing our search strategy, 369 possibly relevant articles were identified, of which 347 titles were discarded for various reasons after perusal of the titles and abstracts (Fig. 1). The full texts of 22 articles were then obtained for more careful examination. After strict application of the inclusion and exclusion criteria, 9 case–control studies11,12,17–23 were finally selected for inclusion in the meta-analysis. All these articles were in English.
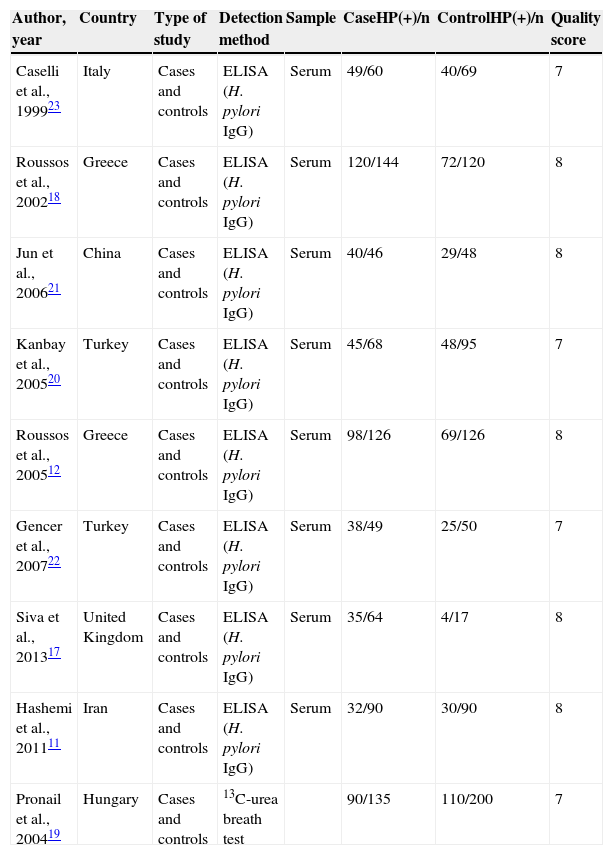
Information extracted from each article was used to create a database that included the following data points: first author, years of publication, number of cases and controls in each study, and number of subjects with positive H. pylori among the cases and the controls. Table 1 shows the quality scores of the studies included. Mean quality was 7.5 stars. All cases had a diagnosis of chronic bronchitis or COPD, according to the following, strictly implemented, diagnostic criteria. Chronic bronchitis was clinically defined as chronic productive cough for 3 months, in at least 2 consecutive years, in a patient in whom other causes of chronic cough were ruled out. If incomplete reversal of airway obstruction was confirmed by spirometry (postbronchodilator forced expired volume in 1s [FEV1] <80% predicted, along with FEV1/FVC <70%), a diagnosis of COPD was given. Of the studies included, 8 used radioimmunoassay (ELISA) for IgG serological detection of H. pylori11,12,17,18,20–23 and only 1 used the 13C-urea breath test.19 Other necessary data were included in the meta-analysis forest plot (Fig. 2).
Characteristics of Studies on Helicobacter pylori in Patients With Chronic Respiratory Disease and Controls.
| Author, year | Country | Type of study | Detection method | Sample | CaseHP(+)/n | ControlHP(+)/n | Quality score |
|---|---|---|---|---|---|---|---|
| Caselli et al., 199923 | Italy | Cases and controls | ELISA (H. pylori IgG) | Serum | 49/60 | 40/69 | 7 |
| Roussos et al., 200218 | Greece | Cases and controls | ELISA (H. pylori IgG) | Serum | 120/144 | 72/120 | 8 |
| Jun et al., 200621 | China | Cases and controls | ELISA (H. pylori IgG) | Serum | 40/46 | 29/48 | 8 |
| Kanbay et al., 200520 | Turkey | Cases and controls | ELISA (H. pylori IgG) | Serum | 45/68 | 48/95 | 7 |
| Roussos et al., 200512 | Greece | Cases and controls | ELISA (H. pylori IgG) | Serum | 98/126 | 69/126 | 8 |
| Gencer et al., 200722 | Turkey | Cases and controls | ELISA (H. pylori IgG) | Serum | 38/49 | 25/50 | 7 |
| Siva et al., 201317 | United Kingdom | Cases and controls | ELISA (H. pylori IgG) | Serum | 35/64 | 4/17 | 8 |
| Hashemi et al., 201111 | Iran | Cases and controls | ELISA (H. pylori IgG) | Serum | 32/90 | 30/90 | 8 |
| Pronail et al., 200419 | Hungary | Cases and controls | 13C-urea breath test | 90/135 | 110/200 | 7 |
ELISA: enzyme-linked immunosorbent assay; HP: Helicobacter pylori; Ig: immunoglobulin.
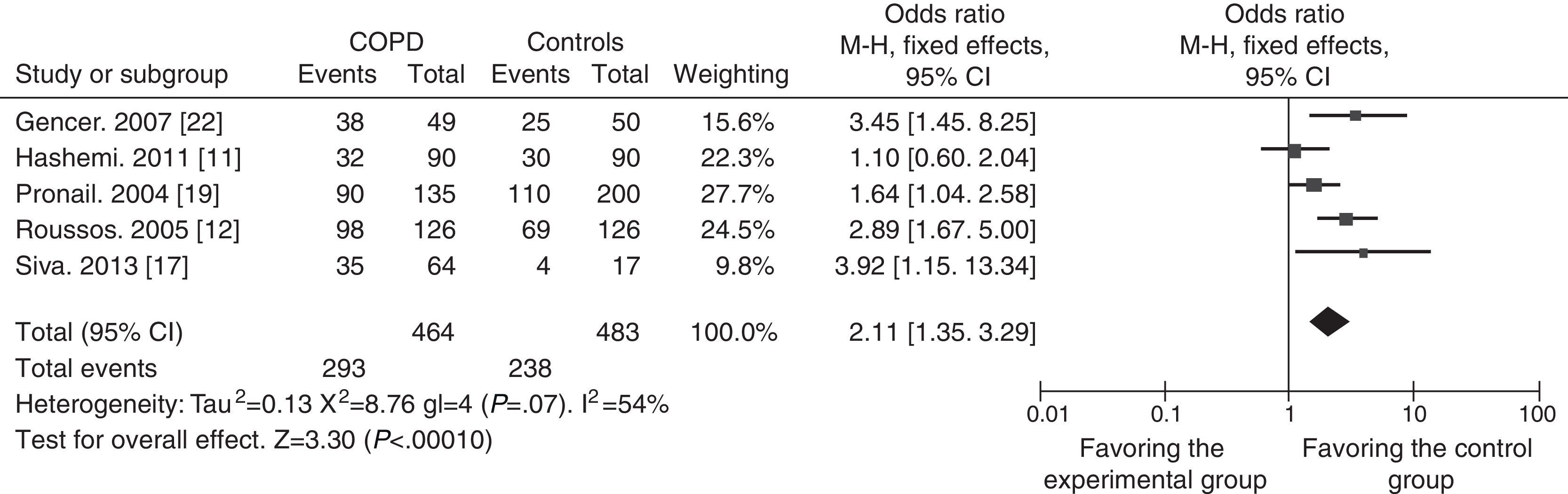
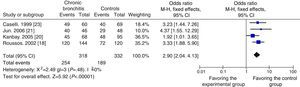
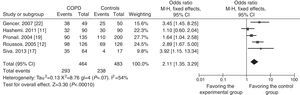
All data were analyzed for heterogeneity. The I2 index was 43%, therefore, a fixed effects model was used to calculate overall OR. Heterogeneity was also analyzed after dividing the data into subgroups. I2 index for the chronic bronchitis subgroup, however, was 0%, so the association between chronic bronchitis and H. pylori was analyzed using the fixed effects model. In contrast, the I2 index in the COPD subgroup was 54%, so the random effects model was used.
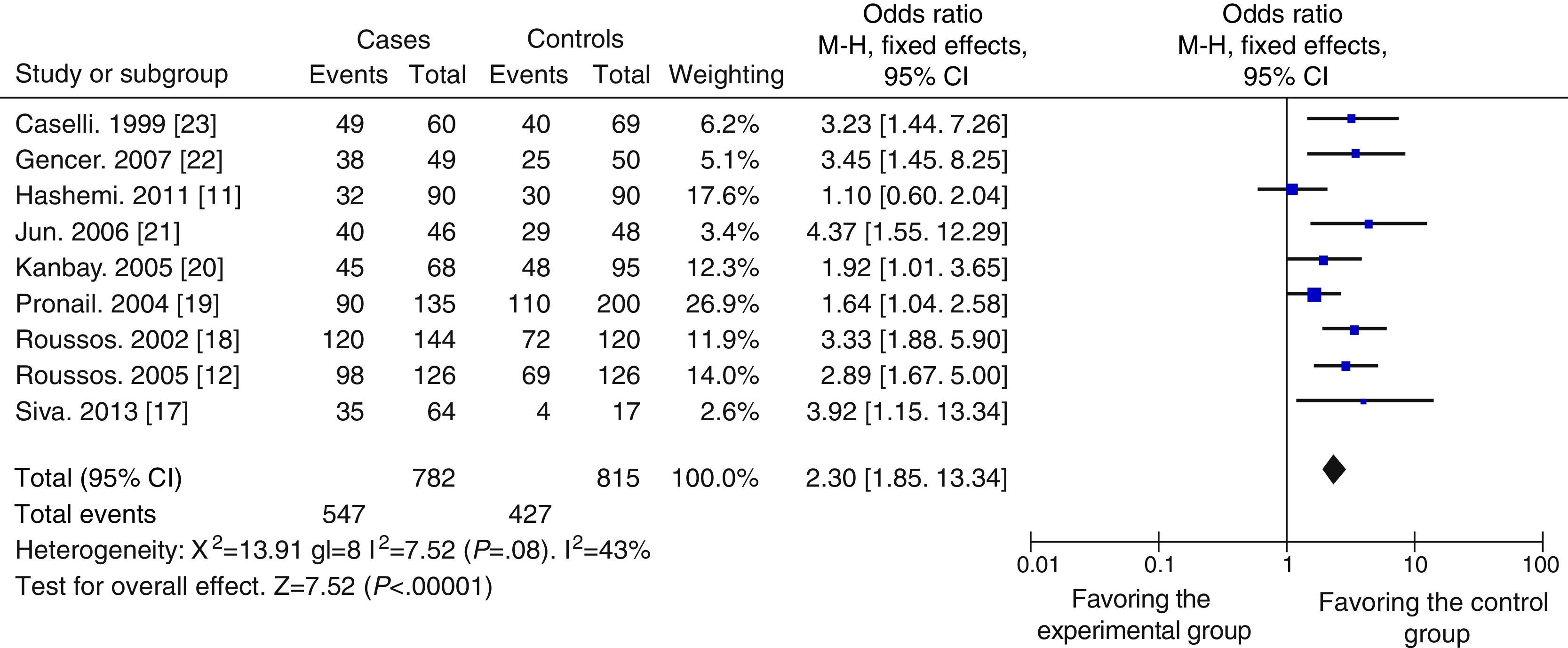
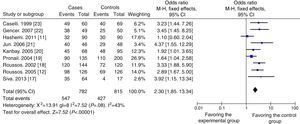
Quantitative SynthesisTo evaluate the possible relation between H. pylori infection and CRD, data were obtained from 9 case–control studies for inclusion in the meta-analysis. A total of 782 cases and 815 controls were included, of which 547 cases and 427 controls were H. pylori-positive, while 235 cases and 388 controls were H. pylori-negative. As shown in Fig. 2, the overall OR was 2.30 (95% CI: 1.85–2.85) and the Z-value for the overall effect test was 7.52 (P<.05).
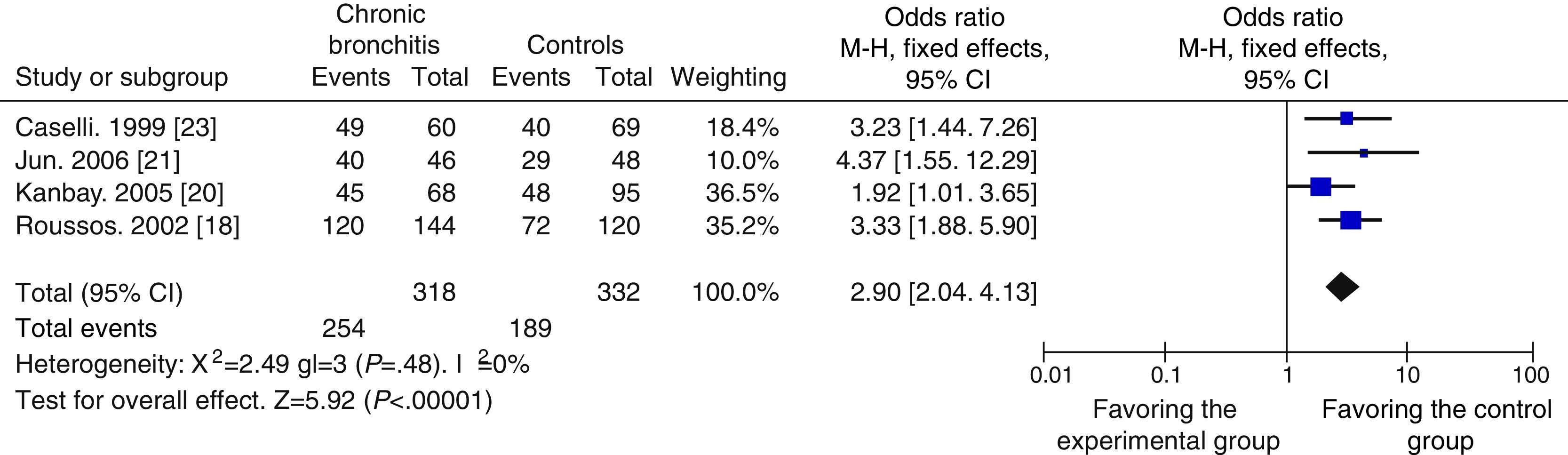
In view of possible differences between the influence of chronic bronchitis and of COPD on the results, a subgroup analysis was also performed to evaluate the relationship. Four case–control studies with 318 cases and 332 controls18,20,21,23 were included in the chronic bronchitis subgroup, and the other 5 studies, with 464 cases and 483 controls,11,12,17,19,22 were included in the COPD subgroup. The OR for the chronic bronchitis subgroup was 2.90 (95% CI: 2.04–4.13) and the Z-value for the overall effect test was 5.92 (P<.05) (Fig. 3). As shown in Fig. 4, the OR for the COPD subgroup was 2.11 (95% CI: 1.35–3.29), and the Z-value for the overall effect test was 3.30 (P<.05).
To compare the difference and evaluate the sensitivity of the overall analysis, the random effects model was also applied. The combined OR and 95% CI for all the studies pooled was 2.40 (95% CI: 1.77–3.26), and the Z-value for the overall effect test was 5.66 (P<.05), similar to the results obtained in the fixed effects model. Likewise, the random effects and fixed effects models were used to evaluate sensitivity and to compare the differences between the subgroup analyses. The results obtained were largely similar.
Bias AssessmentThe fail-safe number (Nfs0.05) for the evaluation of meta-analysis reliability is defined as the number of negative results that could overturn significant results. The Nfs0.05 for the overall meta-analysis was 196, suggesting that the results of the overall meta-analysis were almost entirely unaffected by publication bias. Nfs0.05 was also used to evaluate publication bias in the subgroups. The results were between 50 and 44, suggesting very little publication bias in the results of the subgroup analyses.
DiscussionIn this quantitative meta-analysis, we examined the possible relationship between H. pylori infection and CRD by analyzing published case–control studies. To the best of our knowledge, this is the first meta-analysis to be published that is evaluating this association.
Our meta-analysis revealed a significant association between H. pylori infection and CRDs. Summary OR was 2.30 (95% CI: 1.85–2.85), and the Z-value for the overall effect test was 7.52 (P<.05), indicating that H. pylori infection may be closely related with CRDs. In view of possible differences between the influence of chronic bronchitis and COPD on the results, a subgroup analysis was also performed, yielding similar results.
Although several previous meta-analyses found no significant association between H. pylori and asthma,7,24 the results of our meta-analysis, evaluating the possible relationship between H. pylori infection and CRD, were positive. This raises the interesting concept that H. pylori is closely associated with chronic bronchitis and COPD. Moreover, our results were similar to those reported in meta-analyses that found a close association between H. pylori infection and pulmonary tuberculosis8 or lung cancer.9
The pathogenic mechanisms underlying the positive relationship detected between H. pylori infection and CRD have not yet been clarified.25 One theory suggests that the persistent inflammatory airway response induced by mediators released during H. pylori infection leads to the development of CRD.10,26 Another possible pathogenic mechanism is the increased sensitivity of lung cells and bronchial tissue to external stimulants such as smoke and dust induced by H. pylori infection in the lung,9 thus increasing CRD morbidity.
Our study has several limitations. Firstly, although the results of the case–control studies were quite reliable,24 they could have been affected by some confounding factors, such as sex, age, socioeconomic level and smoking habit.27 The initial publications provided only incomplete information on these factors, making it impossible to perform the corresponding subgroup analyses. Secondly, given the limited number of studies and the low sample sizes, results must be interpreted cautiously. Thirdly, only articles published in open access until October 2013 were retrieved, so some published or unpublished studies meeting the inclusion criteria may have been omitted. Consequently, some unavoidable bias is to be expected, even though the Nfs0.05 did not find any significant publication bias in our study. Fourthly, studies suggest that H. pylori Cag A+ seropositivity is more closely related with CRDs than anti-H. pylori IgG antibody seropositivity.21 However, the relationship between H. pylori Cag A+ strains and CRD was not evaluated because additional details on Cag A seropositivity were provided in only 3 studies.11,12,21 Fifthly, H. pylori seropositivity rates may vary widely, depending on the different detection methods used. In the series included in our study, the 13C-urea breath test was used for the detection of H. pylori in only 1 study,19 while an ELISA11,12,17,18,20–23 method was used in the others.
In conclusion, the results of the overall analysis and subgroup analysis suggest a significant association between H. pylori and CRD. Perhaps the time has come to conduct well-designed studies in large series to clarify the pathogenic mechanisms and to answer questions on the effects of eradication treatment on diseases of the respiratory tract.
FundingThis study was funded by Shandong Cancer Hospital.
Conflict of InterestThe authors state that they have no financial or personal relationship with other persons or organizations that might inappropriately influence their work and they have no professional or personal interests of any other type, nature or class in any product, service and/or company that could be interpreted as influential in the opinion presented in this article.
We thank the Shandong Cancer Hospital.
Please cite this article as: Wang L, Guan Y, Li Y, Liu X, Zhang Y, Wang F, et al. Asociación entre enfermedades respiratorias crónicas y Helicobacter pylori: un metaanálisis. Arch Bronconeumol. 2015;51:273-278.